Korean J Gastroenterol.
2024 Jan;83(1):17-22. 10.4166/kjg.2023.093.
Rare Cause of Hematochezia in Children: Solitary Rectal Ulcer, Single Center Experience
- Affiliations
-
- 1Departments of Pediatric Gastroenterology, Hepatology, and Nutrition, İnönü University, Faculty of Medicine; 2 Department of Pathology, Faculty of Medicine, Malatya, Turkey
- KMID: 2552238
- DOI: http://doi.org/10.4166/kjg.2023.093
Abstract
- Background/Aims
Solitary rectal ulcer syndrome (SRUS) can be overlooked, diagnosed late, or misdiagnosed, particularly in childhood. This study reviewed the 13-year experience of the authors’ institution to increase clinicians' awareness of SRUS in the presence of symptoms. This paper reports the endoscopic and histopathological findings in children presenting with hematochezia.
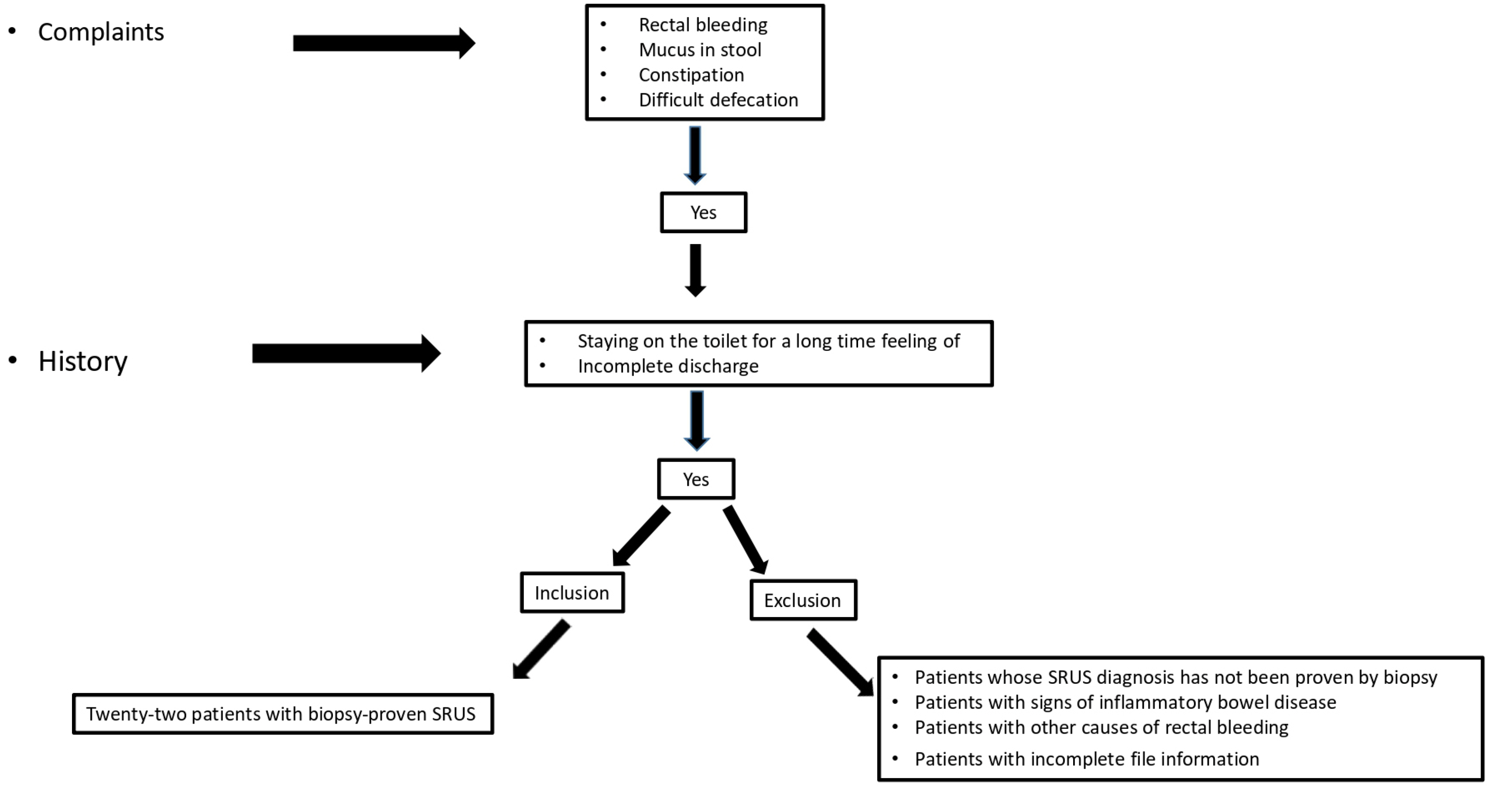
Methods
The clinical and laboratory findings of 22 patients diagnosed with biopsy-proven SRUS in the authors’ clinic between 2007 and 2020 were evaluated retrospectively.
Results
The mean age at diagnosis was 12.5±2.6 years, and 59.1% of the patients were male. The median time of diagnosis was 24 months. A single ulcer lesion was found by colonoscopy in 18 patients (81.8%), two ulcers in two patients (9%), and more than two ulcers in two patients (9%). The pathology reports of all biopsies taken from the lesions were consistent with a solitary rectal ulcer. In the first stage, the treatment was started with toilet training, a high-fiber diet, and laxatives. In 11 patients (50%) who did not respond to the initial treatment, a 5-ASA enema was added. A glucocorticoid enema was added to treatment in five patients (22%) whose complaints did not regress despite this treatment. Clinical remission was achieved in five of the patients (18.1%). The time to diagnosis was significantly shorter in those in remission than those not in remission (p=0.04).
Conclusions
This study is the first large series on Turkish children. An increased awareness of SRUS in children will increase the rate of early diagnosis and treatment, allowing remission in more patients.
Keyword
Figure
Reference
-
1. Keshtgar AS. 2008; Solitary rectal ulcer syndrome in children. Eur J Gastroenterol Hepatol. 20:89–92. DOI: 10.1097/MEG.0b013e3282f402c1. PMID: 18188026.2. Martin CJ, Parks TG, Biggart JD. 1981; Solitary rectal ulcer syndrome in Northern Ireland. 1971-1980. Br J Surg. 68:744–747. DOI: 10.1002/bjs.1800681021. PMID: 7284739.3. Perito ER, Mileti E, Dalal DH, et al. 2012; Solitary rectal ulcer syndrome in children and adolescents. J Pediatr Gastroenterol Nutr. 54:266–270. DOI: 10.1097/MPG.0b013e318240bba5. PMID: 22094902. PMCID: PMC3719860.4. Ertem D, Acar Y, Karaa EK, Pehlivanoglu E. 2002; A rare and often unrecognized cause of hematochezia and tenesmus in childhood: solitary rectal ulcer syndrome. Pediatrics. 110:e79. DOI: 10.1542/peds.110.6.e79. PMID: 12456946.5. Martín de Carpi J, Vilar P, Varea V. 2007; Solitary rectal ulcer syndrome in childhood: a rare, benign, and probably misdiagnosed cause of rectal bleeding. Report of three cases. Dis Colon Rectum. 50:534–539. DOI: 10.1007/s10350-006-0720-1. PMID: 17080282.6. Madigan MR, Morson BC. 1969; Solitary ulcer of the rectum. Gut. 10:871–881. DOI: 10.1136/gut.10.11.871. PMID: 5358578. PMCID: PMC1553062.7. Zhu QC, Shen RR, Qin HL, Wang Y. 2014; Solitary rectal ulcer syndrome: clinical features, pathophysiology, diagnosis and treatment strategies. World J Gastroenterol. 20:738–744. DOI: 10.3748/wjg.v20.i3.738. PMID: 24574747. PMCID: PMC3921483.8. Cruveilhier J. 1829. Ulcere chronique du rectum. Anatomie Pathologique du Corps Humain. JB Bailliere;Paris: p. 1829–1842.9. Tjandra JJ, Fazio VW, Church JM, Lavery IC, Oakley JR, Milsom JW. 1992; Clinical conundrum of solitary rectal ulcer. Dis Colon Rectum. 35:227–234. DOI: 10.1007/BF02051012. PMID: 1740066.10. Godbole P, Botterill I, Newell SJ, Sagar PM, Stringer MD. 2000; Solitary rectal ulcer syndrome in children. J R Coll Surg Edinb. 45:411–414.11. Kiriştioğlu I, Balkan E, Kiliç N, Doğruyol H. 2000; Solitary rectal ulcer syndrome in children. Turk J Pediatr. 42:56–60.12. Thirumal P, Sumathi B, Nirmala D. 2020; A clinical entity often missed-solitary rectal ulcer syndrome in children. Front Pediatr. 8:396. DOI: 10.3389/fped.2020.00396. PMID: 32766189. PMCID: PMC7379901.13. Poddar U, Yachha SK, Krishnani N, Kumari N, Srivastava A, Sen Sarma M. 2020; Solitary rectal ulcer syndrome in children: A report of 140 cases. J Pediatr Gastroenterol Nutr. 71:29–33. DOI: 10.1097/MPG.0000000000002680. PMID: 32097373.14. Urgancı N, Kalyoncu D, Eken KG. 2013; Solitary rectal ulcer syndrome in children: a report of six cases. Gut Liver. 7:752–755. DOI: 10.5009/gnl.2013.7.6.752. PMID: 24312719. PMCID: PMC3848538.15. Gabra HO, Roberts JP, Variend S, Shawis RN. 2005; Solitary rectal ulcer syndrome in children. A report of three cases. Eur J Pediatr Surg. 15:213–216. DOI: 10.1055/s-2004-821180. PMID: 15999319.16. Somani SK, Ghosh A, Avasthi G, Goyal R, Gupta P. 2010; Healing of a bleeding solitary rectal ulcer with multiple sessions of argon plasma. Gastrointest Endosc. 71:578–582. DOI: 10.1016/j.gie.2009.10.038. PMID: 20189517.17. Dehghani SM, Bahmanyar M, Geramizadeh B, Alizadeh A, Haghighat M. 2016; Solitary rectal ulcer syndrome: Is it really a rare condition in children? World J Clin Pediatr. 5:343–348. DOI: 10.5409/wjcp.v5.i3.343. PMID: 27610352. PMCID: PMC4978629.18. Anjum MN, Cheema HA, Malik HS, Hashmi MA. 2017; Clinical spectrum of solitary rectal ulcer in children presenting with per-rectal bleed. J Ayub Med Coll Abbottabad. 29:74–77.19. Suresh N, Ganesh R, Sathiyasekaran M. 2010; Solitary rectal ulcer syndrome: a case series. Indian Pediatr. 47:1059–1061. DOI: 10.1007/s13312-010-0177-0. PMID: 20453265.20. Kowalska-Duplaga K, Lazowska-Przeorek I, Karolewska-Bochenek K, et al. 2017; Solitary rectal ulcer syndrome in children: A case series study. Adv Exp Med Biol. 1020:105–112. DOI: 10.1007/5584_2017_2. PMID: 28255911.21. Blackburn C, McDermott M, Bourke B. 2012; Clinical presentation of and outcome for solitary rectal ulcer syndrome in children. J Pediatr Gastroenterol Nutr. 54:263–265. DOI: 10.1097/MPG.0b013e31823014c0. PMID: 22266488.