J Korean Med Sci.
2024 Jan;39(4):e42. 10.3346/jkms.2024.39.e42.
Cardiac Magnetic Resonance Imaging Findings and Clinical Features of COVID-19 Vaccine-Associated Myocarditis, Compared With Those of Other Types of Myocarditis
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Radiology, Chonnam National University Hwasun Hospital, Hwasun, Korea
- 3Department of Radiology, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2551971
- DOI: http://doi.org/10.3346/jkms.2024.39.e42
Abstract
- Background
To compare the clinical and cardiac magnetic resonance (CMR) imaging findings of coronavirus disease 2019 (COVID-19) vaccine-associated myocarditis (VAM) with those of other types of myocarditis.
Methods
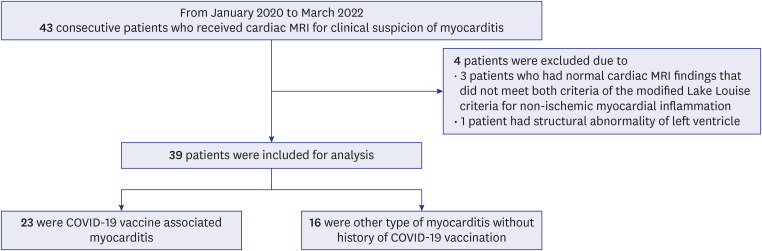
From January 2020 to March 2022, a total of 39 patients diagnosed with myocarditis via CMR according to the Modified Lake Louise criteria were included in the present study. The patients were classified into two groups based on their vaccination status: COVID-19 VAM and other types of myocarditis not associated with COVID-19 vaccination. Clinical outcomes, including the development of clinically significant arrhythmias, sudden cardiac arrest, and death, and CMR imaging features were compared between COVID-19 VAM and other types of myocarditis.
Results
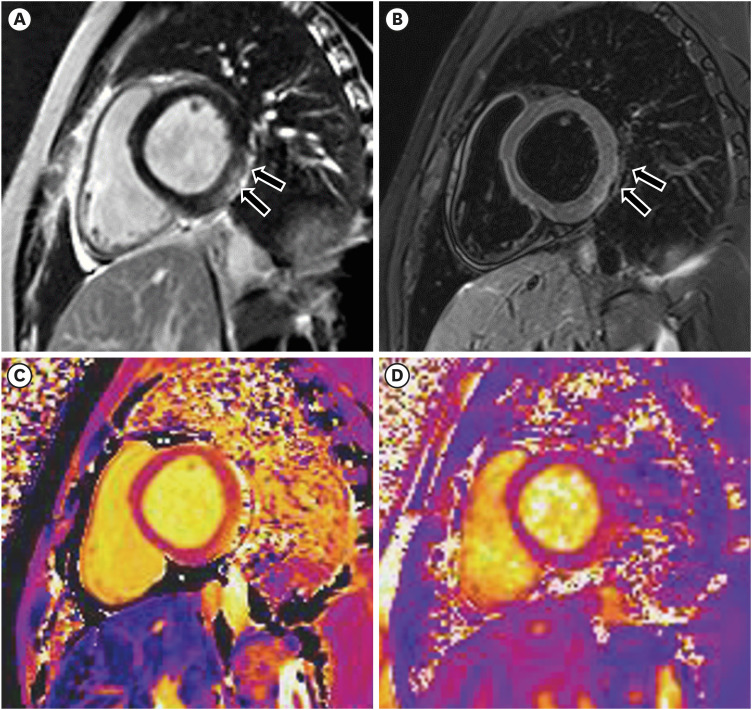
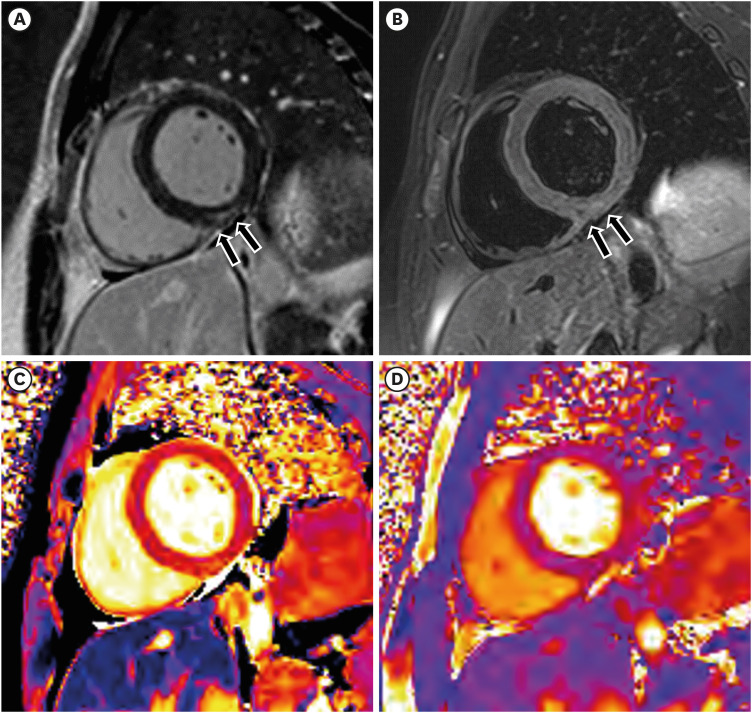
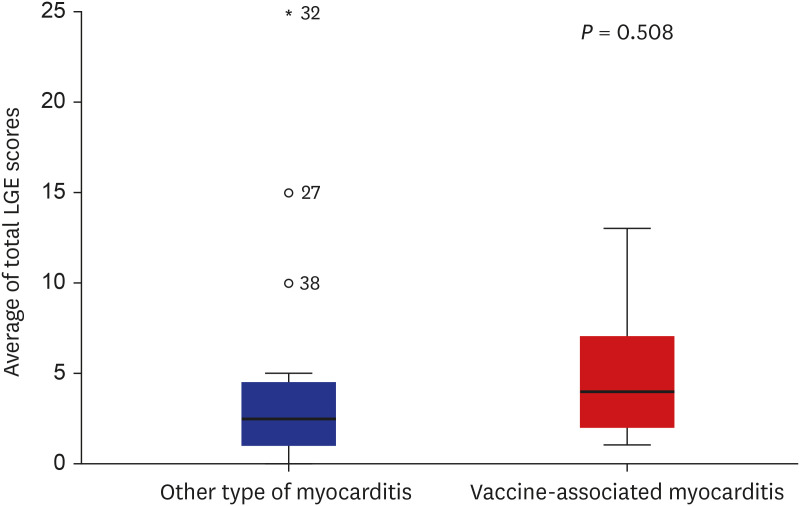
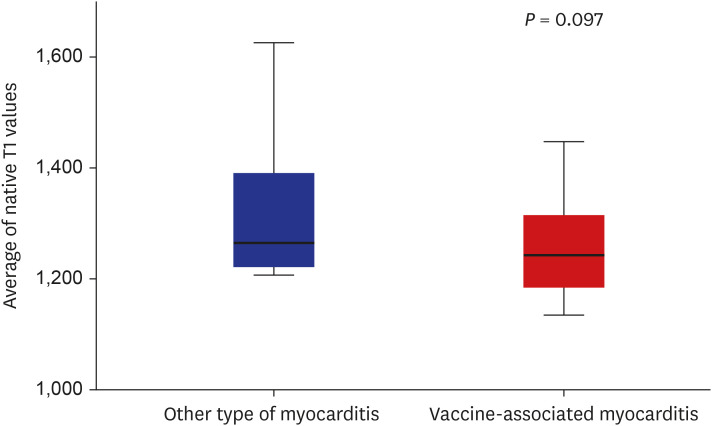
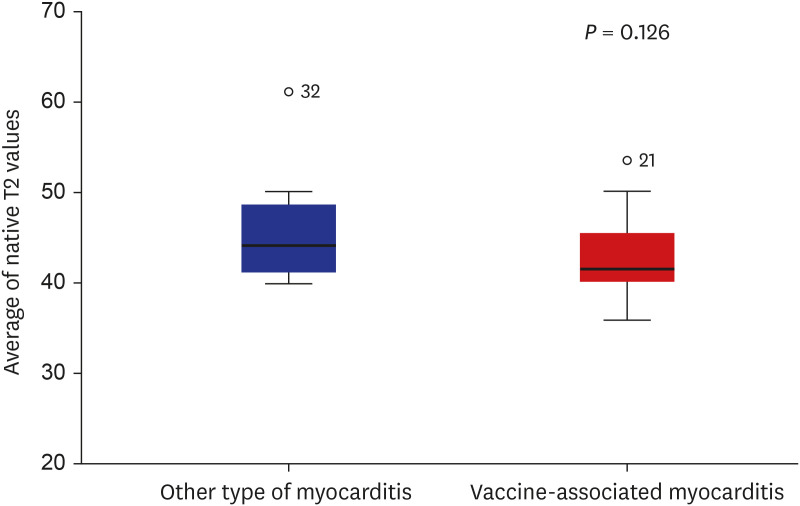
Of the 39 included patients (mean age, 39 years ± 16.4 [standard deviation]; 23 men), 23 (59%) had COVID-19 VAM and 16 (41%) had other types of myocarditis. The occurrence of clinical adverse events did not differ significantly between the two groups. As per the CMR imaging findings, the presence and dominant pattern of late gadolinium enhancement did not differ significantly between the two groups. The presence of high native T1 or T2 values was not significantly different between the two groups. Although the native T1 and T2 values tended to be lower in COVID-19 VAM than in other types of myocarditis, there were no statistically significant differences between the native T1 and T2 values in the two groups.
Conclusion
The present study demonstrated that the CMR imaging findings and clinical outcomes of COVID-19 VAM did not differ significantly from those of other types of myocarditis during hospitalization.
Keyword
Figure
Reference
-
1. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013; 34(33):2636–2648. 2648a–d. PMID: 23824828.2. Knowlton KU, Badorff C. The immune system in viral myocarditis: maintaining the balance. Circ Res. 1999; 85(6):559–561. PMID: 10488059.3. Magno Palmeira M, Umemura Ribeiro HY, Garcia Lira Y, Machado Jucá Neto FO, da Silva Rodrigues IA, Fernandes da Paz LN, et al. Heart failure due to cytomegalovirus myocarditis in immunocompetent young adults: a case report. BMC Res Notes. 2016; 9(1):391. PMID: 27495246.4. Pillay J, Gaudet L, Wingert A, Bialy L, Mackie AS, Paterson DI, et al. Incidence, risk factors, natural history, and hypothesised mechanisms of myocarditis and pericarditis following COVID-19 vaccination: living evidence syntheses and review. BMJ. 2022; 378:e069445. PMID: 35830976.5. Aquaro GD, Perfetti M, Camastra G, Monti L, Dellegrottaglie S, Moro C, et al. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am Coll Cardiol. 2017; 70(16):1977–1987. PMID: 29025554.6. Pan JA, Lee YJ, Salerno M. Diagnostic performance of extracellular volume, native T1, and T2 mapping versus Lake Louise Criteria by cardiac magnetic resonance for detection of acute myocarditis: a meta-analysis. Circ Cardiovasc Imaging. 2018; 11(7):e007598. PMID: 30012826.7. Sanchez Tijmes F, Thavendiranathan P, Udell JA, Seidman MA, Hanneman K. Cardiac MRI assessment of nonischemic myocardial inflammation: state of the art review and update on myocarditis associated with COVID-19 vaccination. Radiol Cardiothorac Imaging. 2021; 3(6):e210252. PMID: 34934954.8. Fronza M, Thavendiranathan P, Chan V, Karur GR, Udell JA, Wald RM, et al. Myocardial injury pattern at MRI in COVID-19 vaccine-associated myocarditis. Radiology. 2022; 304(3):553–562. PMID: 35166587.9. Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018; 72(24):3158–3176. PMID: 30545455.10. Jain SS, Steele JM, Fonseca B, Huang S, Shah S, Maskatia SA, et al. COVID-19 vaccination-associated myocarditis in adolescents. Pediatrics. 2021; 148(5):e2021053427. PMID: 34389692.11. Voinsky I, Baristaite G, Gurwitz D. Effects of age and sex on recovery from COVID-19: analysis of 5769 Israeli patients. J Infect. 2020; 81(2):e102–e103.12. Kellman P, Arai AE. Cardiac imaging techniques for physicians: late enhancement. J Magn Reson Imaging. 2012; 36(3):529–542. PMID: 22903654.13. Kellman P, Arai AE, Xue H. T1 and extracellular volume mapping in the heart: estimation of error maps and the influence of noise on precision. J Cardiovasc Magn Reson. 2013; 15(1):56. PMID: 23800276.14. Wassmuth R, Prothmann M, Utz W, Dieringer M, von Knobelsdorff-Brenkenhoff F, Greiser A, et al. Variability and homogeneity of cardiovascular magnetic resonance myocardial T2-mapping in volunteers compared to patients with edema. J Cardiovasc Magn Reson. 2013; 15(1):27. PMID: 23537111.15. Gräni C, Eichhorn C, Bière L, Kaneko K, Murthy VL, Agarwal V, et al. Comparison of myocardial fibrosis quantification methods by cardiovascular magnetic resonance imaging for risk stratification of patients with suspected myocarditis. J Cardiovasc Magn Reson. 2019; 21(1):14. PMID: 30813942.16. Park YJ, Park SJ, Kim EK, Park KM, Lee SC, On YK, et al. Semi-quantitative versus quantitative assessments of late gadolinium enhancement extent for predicting spontaneous ventricular tachyarrhythmia events in patients with hypertrophic cardiomyopathy. Sci Rep. 2020; 10(1):2920. PMID: 32076039.17. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging. 2002; 18(1):539–542. PMID: 12135124.18. Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson. 2017; 19(1):75. PMID: 28992817.19. Kim PK, Hong YJ, Im DJ, Suh YJ, Park CH, Kim JY, et al. Myocardial T1 and T2 mapping: techniques and clinical applications. Korean J Radiol. 2017; 18(1):113–131. PMID: 28096723.20. Oster ME, Shay DK, Su JR, Gee J, Creech CB, Broder KR, et al. Myocarditis cases reported after mRNA-based COVID-19 vaccination in the US from December 2020 to August 2021. JAMA. 2022; 327(4):331–340. PMID: 35076665.21. Wong HL, Hu M, Zhou CK, Lloyd PC, Amend KL, Beachler DC, et al. Risk of myocarditis and pericarditis after the COVID-19 mRNA vaccination in the USA: a cohort study in claims databases. Lancet. 2022; 399(10342):2191–2199. PMID: 35691322.22. Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022; 28(2):410–422. PMID: 34907393.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Magnetic Resonance Imaging of COVID-19 Myocarditis
- A Case of Myocarditis Presenting With a Hyperechoic Nodule After the First Dose of COVID-19 mRNA Vaccine
- Cardiac Imaging of Acute Myocarditis Following COVID-19 mRNA Vaccination
- Can FDG PET Serve as a Clinically Relevant Tool for Detecting Active Non‑sarcoidotic Myocarditis?
- Diagnosis of Acute Global Myocarditis Using Cardiac MRI with Quantitative T1 and T2 Mapping: Case Report and Literature Review