Clin Endosc.
2024 Jan;57(1):105-111. 10.5946/ce.2023.054.
Increasing trend of endoscopic drainage utilization for the management of pancreatic pseudocyst: insights from a nationwide database
- Affiliations
-
- 1Department of Internal Medicine, SBH Health System, New York, NY, USA
- 2Department of Internal Medicine, Warren Alpert Medical School, Brown University, Providence, RI, USA
- 3Division of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN, USA
- 4Department of Internal Medicine, University of Missouri-Kansas City School of Medicine, Kansas City, MO, USA
- 5Department of Internal Medicine, Icahn School of Medicine at Mount Sinai, Queens, NY, USA
- 6Division of Gastroenterology, SBH Health System, New York, NY, USA
- 7Division of Gastroenterology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA
- KMID: 2551199
- DOI: http://doi.org/10.5946/ce.2023.054
Abstract
- Background/Aims
The pancreatic pseudocyst (PP) is a type of fluid collection that typically develops as a delayed complication of acute pancreatitis. Drainage is indicated for symptomatic patients and/or associated complications, such as infection and bleeding. Drainage modalities include percutaneous, endoscopic, laparoscopic, and open drainage. This study aimed to assess trends in the utilization of different drainage modalities for treating PP from 2016 to 2020. The trends in mortality, mean length of hospital stay, and mean hospitalization costs were also assessed.
Methods
The National Inpatient Sample database was used to obtain data. The variables were generated using International Classification of Diseases-10 diagnostic and procedural codes.
Results
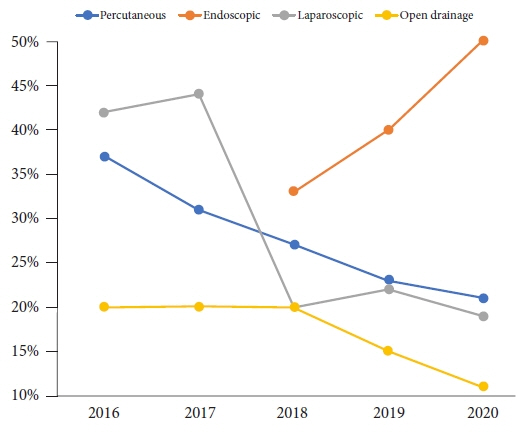
Endoscopic drainage was the most commonly used drainage modality in 2018–2020, with an increasing trend over time (385 procedures in 2018 to 515 in 2020; p=0.003). This is associated with a decrease in the use of other drainage modalities. A decrease in the hospitalization cost for PP requiring drainage was also noted (29,318 United States dollar [USD] in 2016 to 18,087 USD in 2020, p<0.001).
Conclusions
Endoscopic drainage is becoming the most commonly used modality for the treatment of PP in hospitals located in the US. This new trend is associated with decreasing hospitalization costs.
Figure
Reference
-
1. ASGE Standards of Practice Committee, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of inflammatory pancreatic fluid collections. Gastrointest Endosc. 2016; 83:481–488.2. Farias GF, Bernardo WM, De Moura DT, et al. Endoscopic versus surgical treatment for pancreatic pseudocysts: systematic review and meta-analysis. Medicine (Baltimore). 2019; 98:e14255.3. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project-HCUP a federal-state-industry partnership [Internet]. Rockville: Agency for Healthcare Research and Quality;2020. [cited 2023 Apr 5]. Available from: https://hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2020.pdf.4. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) NIS Notes: bedsize of hospital [Internet]. Rockville: Agency for Healthcare Research and Quality;2008. [cited 2023 Apr 27]. Available from: https://hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.5. Wang Y, Omar YA, Agrawal R, et al. Comparison of treatment modalities in pancreatic pseudocyst: a population based study. World J Gastrointest Surg. 2019; 11:365–372.6. Rebhun J, Nassani N, Pan A, et al. Outcomes of open, laparoscopic, and percutaneous drainage of infected walled-off pancreatic necrosis: a nationwide inpatient sample study. Cureus. 2021; 13:e12972.7. Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009; 15:38–47.8. Tyberg A, Karia K, Gabr M, et al. Management of pancreatic fluid collections: a comprehensive review of the literature. World J Gastroenterol. 2016; 22:2256–2270.9. Varadarajulu S, Bang JY, Sutton BS, et al. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology. 2013; 145:583–590.10. Zhao X, Feng T, Ji W. Endoscopic versus surgical treatment for pancreatic pseudocyst. Dig Endosc. 2016; 28:83–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Management of Mediastinal Pancreatic Pseudocyst with Endoscopic Transmural Nasopancreatic Drainage
- Metal versus Plastic Stent for Transmural Drainage of Pancreatic Fluid Collections
- Endoscopic Drainage of Pseudocysts
- Endoscopic Management of Peri-Pancreatic Fluid Collections
- Percutaneous Catheter Drainage of Pancreatic Pseudocyst through the Kidney: A case Report