Clin Endosc.
2024 Jan;57(1):96-104. 10.5946/ce.2022.248.
Rotatable sphincterotome as a rescue device for endoscopic retrograde cholangiopancreatography cannulation: a single-center experience
- Affiliations
-
- 1Department of Hepato-Biliary-Pancreatic Medicine, Cancer Institute Hospital of Japanese Foundation for Cancer Research, Tokyo, Japan
- KMID: 2551198
- DOI: http://doi.org/10.5946/ce.2022.248
Abstract
- Background/Aims
Selective bile duct or pancreatic duct cannulation remains a significant initial hurdle in endoscopic retrograde cholangiopancreatography (ERCP) despite advances in endoscopy and accessories. This study evaluated our experience with a rotatable sphincterotome in cases of difficult cannulation.
Methods
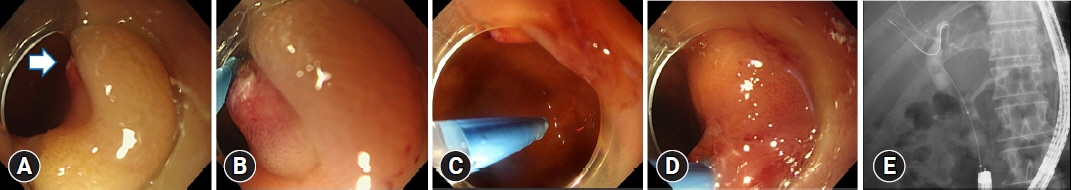
We retrospectively reviewed ERCP cases using TRUEtome, a rotatable sphincterotome, as a rescue device for cannulation at a cancer institute in Japan from October 2014 to December 2021.
Results
TRUEtome was used in 88 patients. Duodenoscopes were used for 51 patients, while single-balloon enteroscopes (SBE) were used for 37 patients. TRUEtome was used for biliary and pancreatic duct cannulation (84.1%), intrahepatic bile duct selection (12.5%), and strictures of the afferent limb (3.4%). Cannulation success rates were similar in the duodenoscope and SBE groups (86.3% vs. 75.7%, p=0.213). TRUEtome was more commonly used in cases with steep cannulation angles in the duodenoscope group and in cases requiring cannulation in different directions in the SBE group. There were no significant differences in adverse events between the two groups.
Conclusions
The cannulation sphincterotome was useful for difficult cannulations in both unaltered and surgically altered anatomies. It may be an option to consider before high-risk procedures such as precut and endoscopic ultrasound-guided rendezvous techniques.
Keyword
Figure
Reference
-
1. Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008; 40:296–301.2. Varadarajulu S, Kilgore ML, Wilcox CM, et al. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006; 64:338–347.3. Williams EJ, Taylor S, Fairclough P, et al. Are we meeting the standards set for endoscopy?: results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007; 56:821–829.4. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001; 54:425–434.5. Testoni PA, Mariani A, Giussani A, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010; 105:1753–1761.6. Op den Winkel M, Schirra J, et al. Biliary cannulation in endoscopic retrograde cholangiography: how to tackle the difficult papilla. Dig Dis. 2022; 40:85–96.7. Tse F, Yuan Y, Moayyedi P, et al. Double-guidewire technique in difficult biliary cannulation for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy. 2017; 49:15–26.8. Facciorusso A, Ramai D, Gkolfakis P, et al. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: systematic review and network meta-analysis. Gastrointest Endosc. 2022; 95:60–71.9. Testoni PA, Mariani A, Aabakken L, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016; 48:657–683.10. Ryozawa S, Itoi T, Katanuma A, et al. Japan Gastroenterological Endoscopy Society guidelines for endoscopic sphincterotomy. Dig Endosc. 2018; 30:149–173.11. Harewood GC, Baron TH. An assessment of the learning curve for precut biliary sphincterotomy. Am J Gastroenterol. 2002; 97:1708–1712.12. Akaraviputh T, Lohsiriwat V, Swangsri J, et al. The learning curve for safety and success of precut sphincterotomy for therapeutic ERCP: a single endoscopist's experience. Endoscopy. 2008; 40:513–516.13. Rossos PG, Kortan P, Haber G. Selective common bile duct cannulation can be simplified by the use of a standard papillotome. Gastrointest Endosc. 1993; 39:67–69.14. Cortas GA, Mehta SN, Abraham NS, et al. Selective cannulation of the common bile duct: a prospective randomized trial comparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999; 50:775–779.15. Schwacha H, Allgaier HP, Deibert P, et al. A sphincterotome-based technique for selective transpapillary common bile duct cannulation. Gastrointest Endosc. 2000; 52:387–391.16. Laasch HU, Tringali A, Wilbraham L, et al. Comparison of standard and steerable catheters for bile duct cannulation in ERCP. Endoscopy. 2003; 35:669–674.17. Kurita A, Kudo Y, Yoshimura K, et al. Comparison between a rotatable sphincterotome and a conventional sphincterotome for selective bile duct cannulation. Endoscopy. 2019; 51:852–857.18. Zhu F, Guan Y, Wang J. Efficacy and safety of the rotatable sphincterotome during ERCP in patients with prior Billroth II gastrectomy (with videos). Surg Endosc. 2021; 35:4849–4856.19. Maluf-Filho F, Kumar A, Ferreria de Souza T, et al. Rotatable sphincterotome facilitates bile duct cannulation in patients with altered ampullary anatomy. Gastroenterol Hepatol (N Y). 2008; 4:59–62.20. Boston Scientific Corporation. TRUEtome product brochure [Internet]. Marlborough: Boston Scientific;2022. [cited 2022 Feb 16]. Available from: https://www.bostonscientific.com/en-US/products/sphincterotomes/truetome-cannulating-sphincterotome.html.21. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.22. Okamoto T, Nakamura K, Yabuta M, et al. Retrograde endosonography-guided hepaticojejunostomy after failed rendezvous in a patient with Child’s resection. Endoscopy. 2022; 54:E131–E132.23. Yoshida A, Minaga K, Takeda O, et al. Successful biliary cannulation using a novel rotatable sphincterotome in a patient with situs inversus totalis. Endoscopy. 2020; 52:E333–E334.24. Matsubara S, Oka M, Nagoshi S. Rotatable sphincterotome as a salvage for guidewire manipulation in endoscopic ultrasound-guided hepaticogastrostomy. Dig Endosc. 2021; 33:e119–e120.25. Takenaka M, Minaga K, Kamata K, et al. Efficacy of a modified double-guidewire technique using an uneven double lumen cannula (uneven method) in patients with surgically altered gastrointestinal anatomy (with video). Surg Endosc. 2020; 34:1432–1441.26. Moxon DR, Hong K, Brown RD, et al. Selective intrahepatic ductal cannulation during ERCP with a sphincterotome. Gastrointest Endosc. 2003; 57:738–743.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
- The Usefulness of Cap-assisted Endoscopic Retrograde Cholangiopancreatography for Cannulation Complicated by a Periampullary Diverticulum
- Prevention of Post-endoscopic Retrograde Cholangiopancreatography Pancreatitis: An Endoscopic Perspective
- Prevention of Postendoscopic Retrograde Cholangiopancreatography Pancreatitis: The Endoscopic Technique
- Endoscopic Retrograde Cholangiopancreatography in Post Gastrectomy Patients