Korean J Women Health Nurs.
2023 Dec;29(4):328-336. 10.4069/kjwhn.2023.12.14.
Factors influencing health-related quality of life in older adult women with sarcopenia: analysis of the Korean National Health and Nutrition Examination Survey 2019
- Affiliations
-
- 1Department of Nursing, Presbyterian Medical Center, Jeonju, Korea
- 2College of Nursing, Jeonbuk National University, Jeonju, Korea
- 3Research Institute of Nursing Science, Jeonbuk National University, Jeonju, Korea
- KMID: 2550996
- DOI: http://doi.org/10.4069/kjwhn.2023.12.14
Abstract
- Purpose
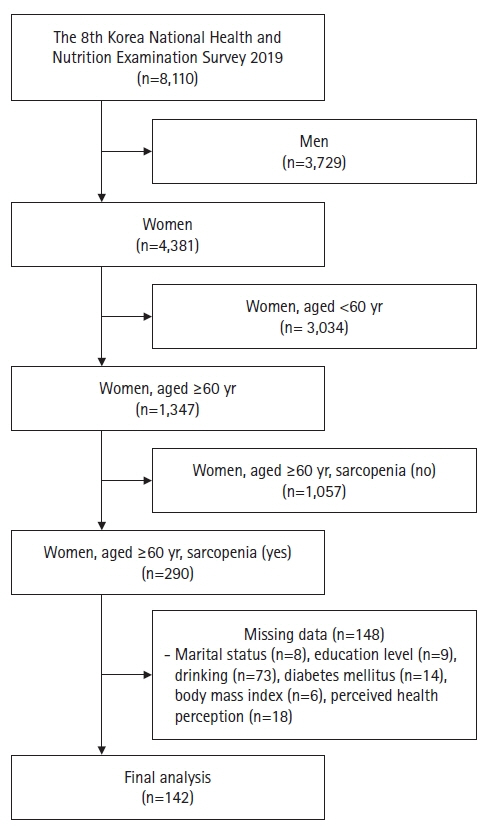
This study aimed to identify factors influencing the health-related quality of life (HRQoL) of older adult women with sarcopenia. Methods: The study was secondary data analysis using data from the 2019 Korea National Health and Nutrition Examination Survey. The final sample consisted of 142 women aged 60 years and older with sarcopenia and were selected from 8,110 women. The participants was analyzed using complex descriptive statistics, independent t-test, and regression. Results: In terms of HRQoL, three general characteristics were found to be influential, with an explanatory power of 56.0%: difficulty climbing stairs, difficulty working, and perceived health status. Having no or mild difficulty when climbing stairs (B=.20, p=.001; B=.21, p<.001) and no or mild difficulty when working (B=.25, p=. 002; B=.208, p=.013) had a significant effect on HRQoL compared to severe difficulty. Having good or ordinary perceived health status had a significant effect on the HRQoL (B=.11, p<.001; B=.09, p<.001). Conclusion: Based on study findings that the HRQoL of older adult women with sarcopenia were influenced by difficulty climbing stairs and working, as well as good perceived health status, healthcare providers should assist elderly women to maintain physical activities in their daily lives.
Keyword
Figure
Reference
-
References
1. Kim KA, Hwang SY. Impact of physical activity, central obesity and depression on the quality of life according to the presence of cardiovascular risk among menopausal middle-aged women: secondary data analysis. Korean J Adult Nurs. 2017; 29(4):382–392. https://doi.org/10.7475/kjan.2017.29.4.382.
Article2. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21(3):300–307.e2. https://doi.org/10.1016/j.jamda.2019.12.012.
Article3. Park HM. Current status of sarcopenia in Korea: a focus on Korean geripausal women. Ann Geriatr Med Res. 2018; 22(2):52–61. https://doi.org/10.4235/agmr.2018.22.2.52.
Article4. Yang L, Smith L, Hamer M. Gender-specific risk factors for incident sarcopenia: 8-year follow-up of the English longitudinal study of ageing. J Epidemiol Community Health. 2019; 73(1):86–88. https://doi.org/10.1136/jech-2018-211258.
Article5. Wu YH, Hwang AC, Liu LK, Peng LN, Chen LK. Sex differences of sarcopenia in Asian populations: The implications in diagnosis and management. J Clin Gerontol Geriatr. 2016; 7(2):37–43. https://doi.org/10.1016/j.jcgg.2016.04.001.
Article6. Cho Y, Shin SY, Shin MJ. Sarcopenic obesity is associated with lower indicators of psychological health and quality of life in Koreans. Nutr Res. 2015; 35(5):384–392. https://doi.org/10.1016/j.nutres.2015.04.002.
Article7. Veronese N, Koyanagi A, Cereda E, Maggi S, Barbagallo M, Dominguez LJ, et al. Sarcopenia reduces quality of life in the long-term: longitudinal analyses from the English longitudinal study of ageing. Eur Geriatr Med. 2022; 13(3):633–639. https://doi.org/10.1007/s41999-022-00627-3.
Article8. Sun S, Lee H, Yim HW, Won HS, Ko YH. The impact of sarcopenia on health-related quality of life in elderly people: Korean National Health and Nutrition Examination Survey. Korean J Intern Med. 2019; 34(4):877–884. https://doi.org/10.3904/kjim.2017.182.
Article9. Xu J, Wan CS, Ktoris K, Reijnierse EM, Maier AB. Sarcopenia is associated with mortality in adults: a systematic review and meta-analysis. Gerontology. 2022; 68(4):361–376. https://doi.org/10.1159/000517099.
Article10. Nho JH, Kim EJ. Factors affecting the quality of life in low-income older adults with sarcopenia: a cross-sectional study. J Korean Acad Nurs. 2023; 53(1):1–11. https://doi.org/10.4040/jkan.22126.
Article11. Seo SJ, Nho JH. Factors affecting the health-related quality of life of older adults with unmet healthcare needs based on the 2018 Korean National Health and Nutrition Examination Survey: a cross-sectional study. J Korean Acad Fundam Nurs. 2022; 29(2):258–268. https://doi.org/10.7739/jkafn.2022.29.2.258.
Article12. Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nurs Scholarsh. 2005; 37(4):336–342. https://doi.org/10.1111/j.1547-5069.2005.00058.x.
Article13. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995; 273(1):59–65. https://doi.org/10.1001/jama.1995.03520250075037.
Article14. Shin Y, Hong YH, Kim HO. Prevalence of sarcopenia in association with ADL, nutritional status and depression among community dwelling elderly women. J Korea Acad-Ind Coop Soc. 2016; 17(1):126–134. https://doi.org/10.5762/KAIS.2016.17.1.126.
Article15. van Reenen M, Oppe M. EQ-5D-3L user guide: basic information on how to use the EQ-5D-3L instrument. ver. 5.1. Rotterdam: EuroQoL Group;2015. p. 22.16. Kim HR. Comparison of prevalence for osteoarthritis and its risk factors between age 60-74 and 75 and over. J Korean Biol Nurs Sci. 2013; 15(4):219–229. https://doi.org/10.7586/jkbns.2013.15.4.219.
Article17. Korean Society for the Study of Obesity (KSSO). KSSO guidelines for obesity treatment, 2020 [Internet]. Seoul: Author;2020. [cited 2022 Oct 17]. Available from: http://general.kosso.or.kr/html/user/core/view/reaction/main/kosso/inc/data/Quick_reference_guideline.pdf.18. Lee JH, Kang HG, Jeong WS, Chae YM, Ji YG. The impact of employment on elder’s quality of life. J Korean Gerontol Soc. 2008; 28(1):143–156.19. Kwon Y, Byun S. The influence of the participation in elderly job project upon job satisfaction, self-efficacy, life satisfaction. J Hum Soc Sci. 2022; 13(2):689–704. https://doi.org/10.22143/HSS21.13.2.49.
Article20. Tang Y, Hu HJ, Lee JW. Two paths for active aging policy: social contribution activity support program for the new middle aged and elderly employment program. Kookmin Soc Science Rev. 2022; 34(2):121–156.
Article21. Lim ES, Lee KJ. Effect of physical ability, depression and social support on quality of life in low income elders living at home. J Korean Gerontol Nurs. 2003; 5(1):38–49.22. Hongu N, Shimada M, Miyake R, Nakajima Y, Nakajima I, Yoshitake Y. Promoting stair climbing as an exercise routine among healthy older adults attending a community-based physical activity program. Sports (Basel). 2019; 7(1):23. https://doi.org/10.3390/sports7010023.
Article23. Kwon M, Park M, Kim HJ, Kim JI, Kim SA. Factors influencing the muscle strength of the elderly without activity restrictions by gender. J Korean Gerontol Nurs. 2021; 23(1):43–53. https://doi.org/10.17079/jkgn.2021.23.1.43.
Article24. Moon JW, Yoon YS, Lee HJ, Jeong TH, Hwang YH, Kim HS. Effects of stair climbing on blood pressure, lipid profiles, and physical fitness. Korean J Sports Med. 2019; 37(1):17–28. https://doi.org/10.5763/kjsm.2019.37.1.17.
Article25. Heo JH, Cho YT. Activity limitations and health behaviors by socioeconomic status among the elderly Seoul population. J Korea Gerontol Soc. 2008; 28(1):87–104.26. Ko YH. The relationships among the physical competence, subjective health status, and health promoting behavior of elderly participating in health activity program. J Digital Converg. 2016; 14(12):571–581. https://doi.org/10.14400/JDC.2016.14.12.571.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influencing Factors on Health-Related Quality of Life in Childbearing Women Based on the Korea National Health and Nutrition Examination Survey (KNHANES) 2019 Data
- Factors Influencing Health-related Quality of Life among Older Korean Women with Osteoporosis: Using Data from Korea National Health and Nutrition Examination Survey 2015 to 2016
- Health and dietary characteristics of the men and women in their middle age according to health-related quality of life: using the Korea National Health and Nutrition Examination Survey data in 2019 and 2021
- Comparison of quality of life and related factors according to premature menopause using the Korea National Health and Nutrition Examination Survey (2014-2017)
- Factors related to Quality of Life among Older Women in South Korea: The Impact of Residential Areas