Korean J Pain.
2024 Jan;37(1):73--83. 10.3344/kjp.23246.
Trends in the prescription of opioids and gabapentinoids in patients with failed back surgery syndrome in Korea: a population-based study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kyungpook National University School of Medicine, Kyunpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2550134
- DOI: http://doi.org/10.3344/kjp.23246
Abstract
- Background
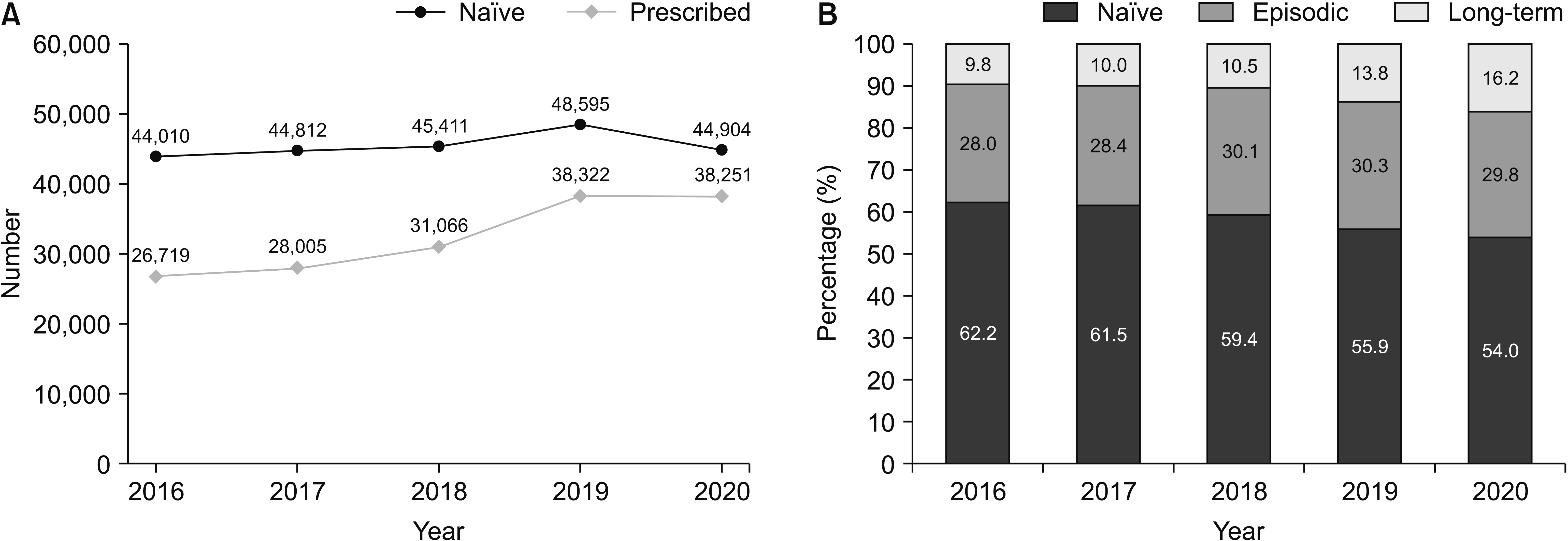
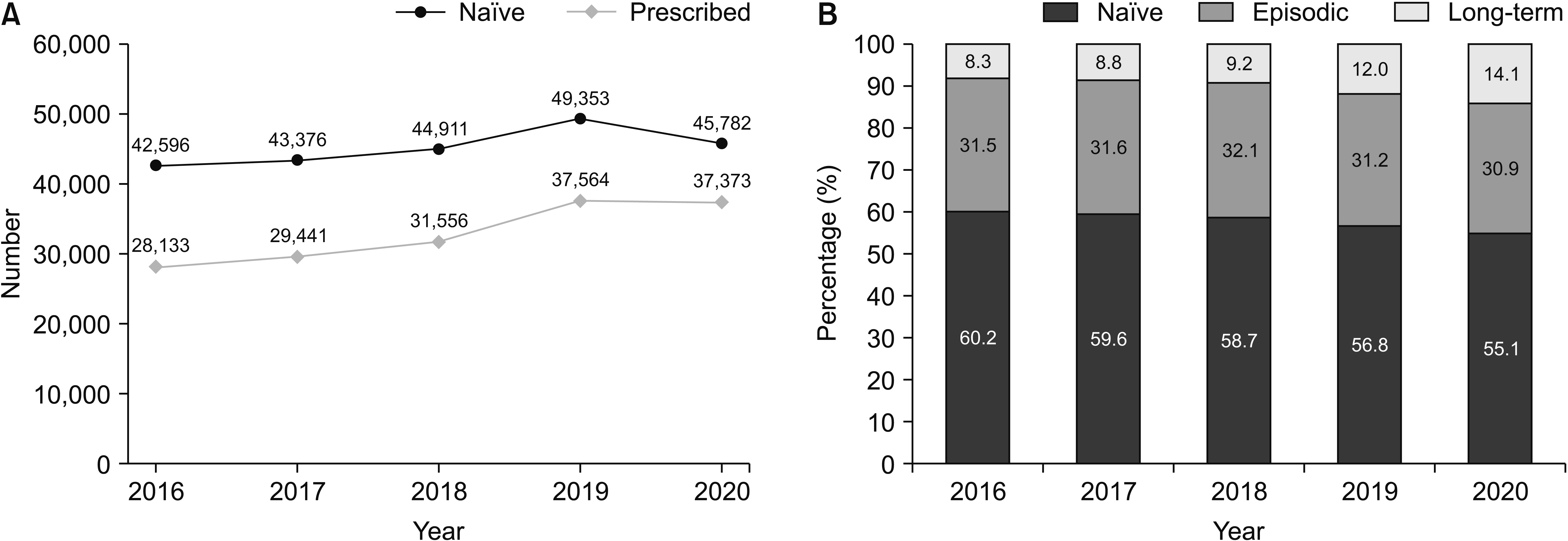
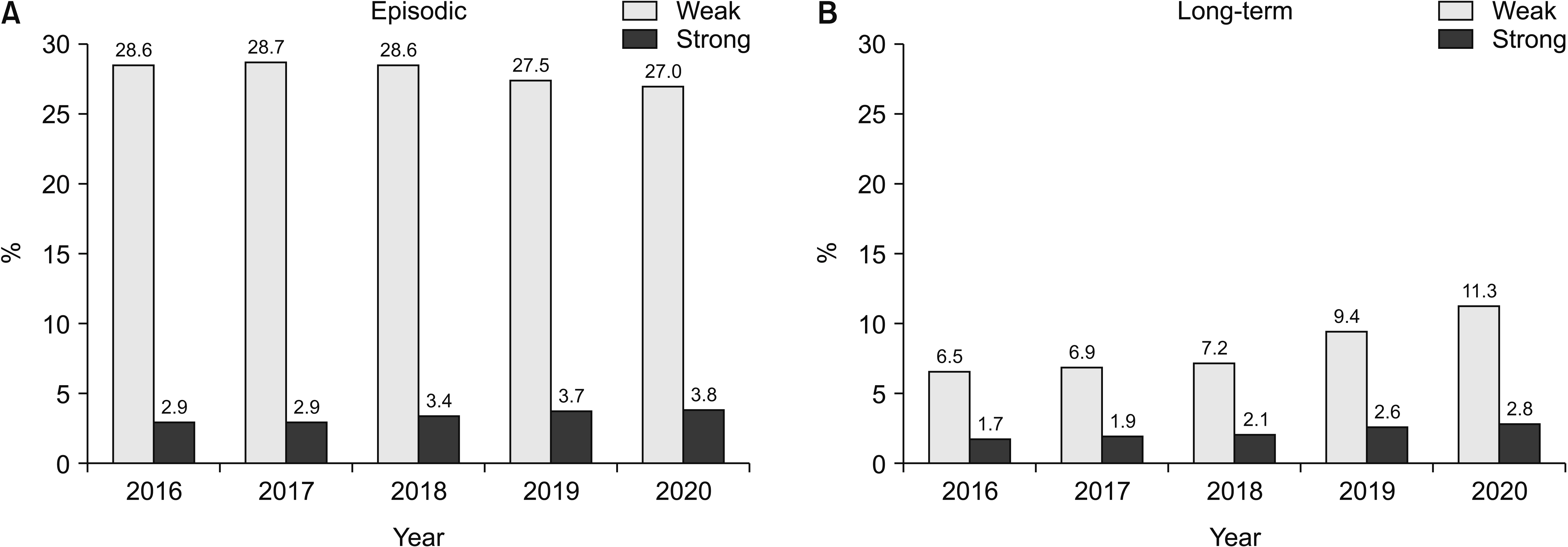
Failed back surgery syndrome (FBSS) is a chronic condition that is characterized by persistent back pain following one or more spinal surgeries. Pharmacological interventions, such as the use of opioids and gabapentinoids, are frequently used in the treatment of FBSS. However, prolonged and excessive use of these medications can lead to dependence and adverse effects. This study investigates trends in opioid and gabapentinoid prescriptions among patients with FBSS in Korea from 2016 to 2020.
Methods
Data from the Health Insurance and Review Agency were analyzed, and claims listing FBSS were selected for the study. Prescription patterns of opioids and gabapentinoids were classified based on the number of days prescribed per year.
Results
Of the 390,095 patients diagnosed with FBSS, 41.6% of the patients were prescribed gabapentinoids, and 42.0% of them were prescribed opioids, while 10.6% of the patients were classified as long-term gabapentinoid users, 11.4% as long-term opioid users, and 7.4% of the patients were found to have long-term prescriptions for both drugs. The proportion of patients who received both gabapentinoid and opioid prescriptions increased annually. The doses of opioids prescribed have also increased along with the increase in the number of patients receiving opioid prescriptions.
Conclusions
The prescription rates of opioids and gabapentinoids among patients with FBSS in Korea continue to increase steadily, posing potential risks of addiction and adverse effects. Further research is needed to better understand the actual status of addiction in patients with FBSS.
Keyword
Figure
Reference
-
1. Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. 2020; Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 8:299. DOI: 10.21037/atm.2020.02.175. PMID: 32355743. PMCID: PMC7186678.2. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. 2005; United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 30:1441–5. DOI: 10.1097/01.brs.0000166503.37969.8a. PMID: 15959375.3. National Health Insurance Service. 2021. 2020 Annual report of major surgery statistics [Internet]. National Health Insurance Service;Available at: https://www.nhis.or.kr/nhis/together/wbhaec06800m01.do?mode=view&articleNo=10813594.4. Baber Z, Erdek MA. 2016; Failed back surgery syndrome: current perspectives. J Pain Res. 9:979–87. DOI: 10.2147/JPR.S92776. PMID: 27853391. PMCID: PMC5106227.5. Waguespack A, Schofferman J, Slosar P, Reynolds J. 2002; Etiology of long-term failures of lumbar spine surgery. Pain Med. 3:18–22. DOI: 10.1046/j.1526-4637.2002.02007.x. PMID: 15102214.6. Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, et al. 2015; Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 473:1988–99. DOI: 10.1007/s11999-015-4193-1. PMID: 25694267. PMCID: PMC4419014.7. Chen YC, Lee CY, Chen SJ. 2019; Narcotic addiction in failed back surgery syndrome. Cell Transplant. 28:239–47. DOI: 10.1177/0963689718796072. PMID: 30168351. PMCID: PMC6425112. PMID: 8007cb7d552d4576831d4209eee4374f.8. Goodman CW, Brett AS. 2019; A clinical overview of off-label use of gabapentinoid drugs. JAMA Intern Med. 179:695–701. DOI: 10.1001/jamainternmed.2019.0086. PMID: 30907944.9. Evoy KE, Covvey JR, Peckham AM, Ochs L, Hultgren KE. 2019; Reports of gabapentin and pregabalin abuse, misuse, dependence, or overdose: an analysis of the Food and Drug Administration Adverse Events Reporting System (FAERS). Res Social Adm Pharm. 15:953–8. DOI: 10.1016/j.sapharm.2018.06.018. PMID: 31303196.10. Von Korff M, Saunders K, Thomas Ray G, Boudreau D, Campbell C, Merrill J, et al. 2008; De facto long-term opioid therapy for noncancer pain. Clin J Pain. 24:521–7. Erratum in: Clin J Pain 2014; 30: 830. DOI: 10.1097/AJP.0b013e318169d03b. PMID: 18574361. PMCID: PMC3286630.11. Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E. 2001; Equianalgesic dose ratios for opioids. a critical review and proposals for long-term dosing. J Pain Symptom Manage. 22:672–87. DOI: 10.1016/S0885-3924(01)00294-9. PMID: 11495714.12. Swarm RA, Paice JA, Anghelescu DL, Are M, Bruce JY, Buga S, et al. 2019; Adult Cancer Pain, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 17:977–1007. DOI: 10.6004/jnccn.2019.0038. PMID: 31390582.13. Petersen EA, Schatman ME, Sayed D, Deer T. 2021; Persistent spinal pain syndrome: new terminology for a new era. J Pain Res. 14:1627–30. DOI: 10.2147/JPR.S320923. PMID: 34135626. PMCID: PMC8197591.14. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. 2019; Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 160:19–27. DOI: 10.1097/j.pain.0000000000001384. PMID: 30586067.15. Thomson S, Jacques L. 2009; Demographic characteristics of patients with severe neuropathic pain secondary to failed back surgery syndrome. Pain Pract. 9:206–15. DOI: 10.1111/j.1533-2500.2009.00276.x. PMID: 19281499.16. Patel R, Dickenson AH. 2016; Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect. 4:e00205. DOI: 10.1002/prp2.205. PMID: 27069626. PMCID: PMC4804325.17. Robertson K, Marshman LAG, Plummer D, Downs E. 2019; Effect of gabapentin vs pregabalin on pain intensity in adults with chronic sciatica: a randomized clinical trial. JAMA Neurol. 76:28–34. Erratum in: JAMA Neurol 2019; 76: 117. DOI: 10.1001/jamaneurol.2018.3077. PMID: 30326006. PMCID: PMC6439871.18. Mu A, Weinberg E, Moulin DE, Clarke H. 2017; Pharmacologic management of chronic neuropathic pain: review of the Canadian Pain Society consensus statement. Can Fam Physician. 63:844–52. PMID: 29138154. PMCID: PMC5685445.19. Johansen ME. 2018; Gabapentinoid use in the United States 2002 through 2015. JAMA Intern Med. 178:292–4. DOI: 10.1001/jamainternmed.2017.7856. PMID: 29297045. PMCID: PMC5838608.20. Hudson TJ, Edlund MJ, Steffick DE, Tripathi SP, Sullivan MD. 2008; Epidemiology of regular prescribed opioid use: results from a national, population-based survey. J Pain Symptom Manage. 36:280–8. DOI: 10.1016/j.jpainsymman.2007.10.003. PMID: 18619768. PMCID: PMC4741098.21. Sullivan MD, Von Korff M, Banta-Green C, Merrill JO, Saunders K. 2010; Problems and concerns of patients receiving chronic opioid therapy for chronic non-cancer pain. Pain. 149:345–53. DOI: 10.1016/j.pain.2010.02.037. PMID: 20334974. PMCID: PMC3318978.22. Chaparro LE, Furlan AD, Deshpande A, Mailis-Gagnon A, Atlas S, Turk DC. 2013; Opioids compared to placebo or other treatments for chronic low-back pain. Cochrane Database Syst Rev. (8):CD004959. DOI: 10.1002/14651858.CD004959.pub4. PMCID: PMC6481826.23. Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, et al. 2018; Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA. 319:872–82. DOI: 10.1001/jama.2018.0899. PMID: 29509867. PMCID: PMC5885909.24. Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden JB, Martin BC. 2008; Trends in use of opioids for non-cancer pain conditions 2000-2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 138:440–9. DOI: 10.1016/j.pain.2008.04.027. PMID: 18547726. PMCID: PMC2668925.25. Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. 2008; Expenditures and health status among adults with back and neck problems. JAMA. 299:656–64. Erratum in: JAMA 2008; 299: 2630. DOI: 10.1001/jama.299.6.656. PMID: 18270354.26. Song IA, Choi HR, Oh TK. 2022; Long-term opioid use and mortality in patients with chronic non-cancer pain: ten-year follow-up study in South Korea from 2010 through 2019. EClinicalMedicine. 51:101558. DOI: 10.1016/j.eclinm.2022.101558. PMID: 35875817. PMCID: PMC9304910.27. Long DM, Filtzer DL, BenDebba M, Hendler NH. 1988; Clinical features of the failed-back syndrome. J Neurosurg. 69:61–71. DOI: 10.3171/jns.1988.69.1.0061. PMID: 2967891.28. Volkow ND, McLellan AT. 2016; Opioid abuse in chronic pain--misconceptions and mitigation strategies. N Engl J Med. 374:1253–63. DOI: 10.1056/NEJMra1507771. PMID: 27028915.29. Kobus AM, Smith DH, Morasco BJ, Johnson ES, Yang X, Petrik AF, et al. 2012; Correlates of higher-dose opioid medication use for low back pain in primary care. J Pain. 13:1131–8. DOI: 10.1016/j.jpain.2012.09.003. PMID: 23117108. PMCID: PMC3641146.30. Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. 2010; Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 152:85–92. DOI: 10.7326/0003-4819-152-2-201001190-00006. PMID: 20083827. PMCID: PMC3000551.31. Busse JW, Craigie S, Juurlink DN, Buckley DN, Wang L, Couban RJ, et al. 2017; Guideline for opioid therapy and chronic noncancer pain. CMAJ. 189:E659–66. DOI: 10.1503/cmaj.170363. PMID: 28483845. PMCID: PMC5422149.32. Häuser W, Bock F, Hüppe M, Nothacker M, Norda H, Radbruch L, et al. Koautoren für die Konsensusgruppe der 2. 2020; Aktualisierung der S3-Leitlinie LONTS. Recommendations of the second update of the LONTS guidelines: long-term opioid therapy for chronic noncancer pain. Schmerz. 34:204–44. German. Erratum in: Schmerz 2021; 35: 59-60. DOI: 10.1007/s00482-020-00472-y. PMID: 32377861.33. Moisset X, Martinez V. 2016; Opioid use for the management of chronic non-cancer pain: French guidelines. Rev Neurol (Paris). 172:337–8. DOI: 10.1016/j.neurol.2016.05.004. PMID: 27342007.34. Schwan S, Sundström A, Stjernberg E, Hallberg E, Hallberg P. 2010; A signal for an abuse liability for pregabalin--results from the Swedish spontaneous adverse drug reaction reporting system. Eur J Clin Pharmacol. 66:947–53. DOI: 10.1007/s00228-010-0853-y. PMID: 20563568.35. Peckham AM, Fairman KA, Sclar DA. 2017; Prevalence of gabapentin abuse: comparison with agents with known abuse potential in a commercially insured US population. Clin Drug Investig. 37:763–73. DOI: 10.1007/s40261-017-0530-3. PMID: 28451875.36. Campbell LS, Coomer TN, Jacob GK, Lenz RJ. 2021; Gabapentin controlled substance status. J Am Pharm Assoc (2003). 61:e218–24. DOI: 10.1016/j.japh.2021.01.025. PMID: 33674205.37. Bao H, Wu Z, Wang Q, Wang J, Zhang L, Meng L, et al. 2021; The efficacy of gabapentin combined with opioids for neuropathic cancer pain: a meta-analysis. Transl Cancer Res. 10:637–44. DOI: 10.21037/tcr-20-2692. PMID: 35116397. PMCID: PMC8798151.38. Knezevic NN, Aijaz T, Camacho-Ortega A, Candido KD. 2021; A retrospective analysis of gabapentinoid and opioids to opioid monotherapy for pain relief in patients with chronic neck and low back pain. Pain Med. 22:1760–6. DOI: 10.1093/pm/pnab006. PMID: 33502505.39. Peckham AM, Fairman KA, Sclar DA. 2018; All-cause and drug-related medical events associated with overuse of gabapentin and/or opioid medications: a retrospective cohort analysis of a commercially insured US population. Drug Saf. 41:213–28. DOI: 10.1007/s40264-017-0595-1. PMID: 28956286.40. Peet ED, Dana B, Sheng FY, Powell D, Shetty K, Stein BD. 2023; Trends in the concurrent prescription of opioids and gabapentin in the US, 2006 to 2018. JAMA Intern Med. 183:162–4. DOI: 10.1001/jamainternmed.2022.5268. PMID: 36409473. PMCID: PMC9679956.41. Højsted J, Nielsen PR, Guldstrand SK, Frich L, Sjøgren P. 2010; Classification and identification of opioid addiction in chronic pain patients. Eur J Pain. 14:1014–20. DOI: 10.1016/j.ejpain.2010.04.006. PMID: 20494598.42. O'Brien T, Christrup LL, Drewes AM, Fallon MT, Kress HG, McQuay HJ, et al. 2017; European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur J Pain. 21:3–19. DOI: 10.1002/ejp.970. PMID: 27991730. PMCID: PMC6680203.43. Elkholy MAE, Nagaty A, Abdelbar AE, Simry HAM, Raslan AM. 2023; Effect of spinal cord stimulation on quality of life and opioid consumption in patients with failed back surgery syndrome. Pain Pract. doi: 10.1111/papr.13300. DOI: 10.1111/papr.13300. PMID: 37753793.44. De La Porte C, Van de Keift E. 1993; Spinal cord stimulation in failed back surgery syndrome. Pain. 52:55–61. DOI: 10.1016/0304-3959(93)90113-4. PMID: 8446436.45. Van Buyten JP, Van Zundert J, Vueghs P, Vanduffel L. 2001; Efficacy of spinal cord stimulation: 10 years of experience in a pain centre in Belgium. Eur J Pain. 5:299–307. DOI: 10.1053/eujp.2001.0249. PMID: 11558985.46. de la Porte C, Siegfried J. 1983; Lumbosacral spinal fibrosis (spinal arachnoiditis). Its diagnosis and treatment by spinal cord stimulation. Spine (Phila Pa 1976). 8:593–603. DOI: 10.1097/00007632-198309000-00005. PMID: 6228017.47. Ohnmeiss DD, Rashbaum RF, Bogdanffy GM. 1996; Prospective outcome evaluation of spinal cord stimulation in patients with intractable leg pain. Spine (Phila Pa 1976). 21:1344–50. DOI: 10.1097/00007632-199606010-00013. PMID: 8725927.48. Nissen M, Ikäheimo TM, Huttunen J, Leinonen V, Jyrkkänen HK, von Und Zu Fraunberg M. 2021; Higher preimplantation opioid doses associated with long-term spinal cord stimulation failure in 211 patients with failed back surgery syndrome. Neuromodulation. 24:102–11. DOI: 10.1111/ner.13297. PMID: 33073907. PMCID: PMC7894290.49. Dhruva SS, Murillo J, Ameli O, Morin PE, Spencer DL, Redberg RF, et al. 2023; Long-term outcomes in use of opioids, nonpharmacologic pain interventions, and total costs of spinal cord stimulators compared with conventional medical therapy for chronic pain. JAMA Neurol. 80:18–29. DOI: 10.1001/jamaneurol.2022.4166. PMID: 36441532. PMCID: PMC9706399.50. Yousef AA, EL-Deen AS, Al-Deeb AE. 2010; The role of adding hyaluronidase to fluoroscopically guided caudal steroid and hypertonic saline injection in patients with failed back surgery syndrome: a prospective, double-blinded, randomized study. Pain Pract. 10:548–53. DOI: 10.1111/j.1533-2500.2009.00357.x. PMID: 20412501.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Failed Back Surgery Syndrome: A Review Article
- The Factors Affecting the Fovorable Outcomes in the Treatment of the Failed Back Surgery Syndrome
- Raiofrequency Neurotomy for Lumbar Facet Joint Pain in the Patients with Failed Back Surgery Syndrome
- Treatment of Chronic Low Back and Leg Pain Using a Spinal Cord Stimulator: Two case reports
- Anterior Lumbar Interbody Fusion Using BAK Cage for Treatment of Failed Back Surgery Syndrome