J Korean Med Sci.
2023 Dec;38(50):e388. 10.3346/jkms.2023.38.e388.
Impact of an Emergency Department Isolation Policy for Patients With Suspected COVID-19 on Door-toElectrocardiography Time and Clinical Outcomes in Patients With Acute Myocardial Infarction
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea
- 3Disaster Medicine Research Center, Seoul National University Medical Research Center, Seoul, Korea
- KMID: 2549957
- DOI: http://doi.org/10.3346/jkms.2023.38.e388
Abstract
- Background
Rapid electrocardiography diagnosis within 10 minutes of presentation is critical for acute myocardial infarction (AMI) patients in the emergency department (ED). However, the coronavirus disease 2019 (COVID-19) pandemic has significantly impacted the emergency care system. Screening for COVID-19 symptoms and implementing isolation policies in EDs may delay the door-to-electrocardiography (DTE) time.
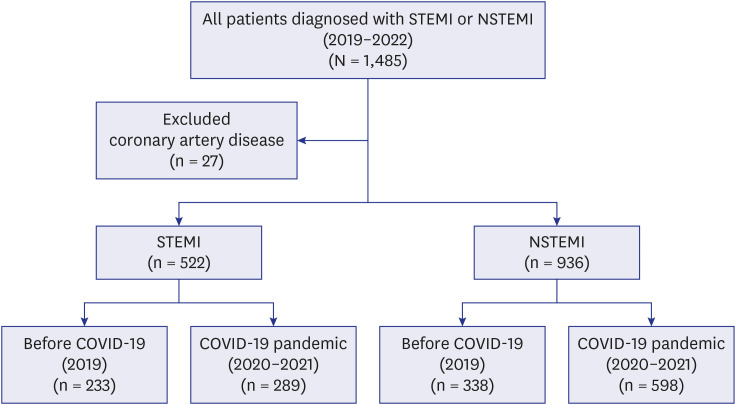
Methods
We conducted a cross-sectional study of 1,458 AMI patients who presented to a single ED in South Korea from January 2019 to December 2021. We used multivariate logistic regression analysis to assess the impact of COVID-19 pandemic and ED isolation policies on DTE time and clinical outcomes.
Results
We found that the mean DTE time increased significantly from 5.5 to 11.9 minutes (P < 0.01) in ST segment elevation myocardial infarction (STEMI) patients and 22.3 to 26.7 minutes (P < 0.01) in non-ST segment elevation myocardial infarction (NSTEMI) patients. Isolated patients had a longer mean DTE time compared to non-isolated patients in both STEMI (9.2 vs. 24.4 minutes) and NSTEMI (22.4 vs. 61.7 minutes) groups (P < 0.01). The adjusted odds ratio (aOR) for the effect of COVID-19 duration on DTE ≥ 10 minutes was 1.93 (95% confidence interval [CI], 1.51–2.47), and the aOR for isolation status was 5.62 (95% CI, 3.54–8.93) in all patients. We did not find a significant association between in-hospital mortality and the duration of COVID-19 (aOR, 0.9; 95% CI, 0.52–1.56) or isolation status (aOR, 1.62; 95% CI, 0.71–3.68).
Conclusion
Our study showed that ED screening or isolation policies in response to the COVID-19 pandemic could lead to delays in DTE time. Timely evaluation and treatment of emergency patients during pandemics are essential to prevent potential delays that may impact their clinical outcomes.
Keyword
Figure
Reference
-
1. Bates ER, Jacobs AK. Time to treatment in patients with STEMI. N Engl J Med. 2013; 369(10):889–892. PMID: 24004114.2. Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guidelines for the management of patients with unstable angina and non–ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on the management of patients with unstable angina). J Am Coll Cardiol. 2000; 36(3):970–1062. PMID: 10987629.3. Phelan MP, Glauser J, Smith E, Martin C, Schrump S, Mahone P, et al. Improving emergency department door-to-electrocardiogram time in ST segment elevation myocardial infarction. Crit Pathw Cardiol. 2009; 8(3):119–121. PMID: 19726931.4. Chhabra S, Eagles D, Kwok ES, Perry JJ. Interventions to reduce emergency department door-to- electrocardiogram times: a systematic review. CJEM. 2019; 21(5):607–617. PMID: 31088589.5. Garcia S, Stanberry L, Schmidt C, Sharkey S, Megaly M, Albaghdadi MS, et al. Impact of COVID-19 pandemic on STEMI care: an expanded analysis from the United States. Catheter Cardiovasc Interv. 2021; 98(2):217–222. PMID: 32767652.6. Vlachakis PK, Tentolouris A, Kanakakis I. Concerns for management of STEMI patients in the COVID-19 era: a paradox phenomenon. J Thromb Thrombolysis. 2020; 50(4):809–813. PMID: 32734526.7. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020; 41(19):1852–1853. PMID: 32297932.8. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020; 13(4):e006631. PMID: 32182131.9. McLaren JT, Taher AK, Chartier LB. Flattening the other curve: reducing emergency department STEMI delays during the COVID-19 pandemic. Am J Emerg Med. 2021; 49:367–372. PMID: 34246966.10. Park J, Lim T. Korean triage and acuity scale (KTAS). J Korean Soc Emerg Med. 2017; 28(6):547–551.11. Kim JH, An JAR, Min PK, Bitton A, Gawande AA. How South Korea responded to the COVID-19 outbreak in Daegu. NEJM Catal Innov Care Deliv. 2020; 1(4):12. Diercks DB, Kirk JD, Lindsell CJ, Pollack CV Jr, Hoekstra JW, Gibler WB, et al. Door-to-ECG time in patients with chest pain presenting to the ED. Am J Emerg Med. 2006; 24(1):1–7. PMID: 16338501.13. Bruoha S, Yosefy C, Gallego-Colon E, Rieck J, Orlov Y, Osherov A, et al. Impact in total ischemic time and ST-segment elevation myocardial infarction admissions during COVID-19. Am J Emerg Med. 2021; 45:7–10. PMID: 33640628.14. Chew NW, Sia CH, Wee HL, Benedict LJ, Rastogi S, Kojodjojo P, et al. Impact of the COVID-19 pandemic on door-to-balloon time for primary percutaneous coronary intervention—results from the Singapore western STEMI Network—. Circ J. 2021; 85(2):139–149. PMID: 33162491.15. Moroni F, Gramegna M, Ajello S, Beneduce A, Baldetti L, Vilca LM, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020; 2(10):1620–1624. PMID: 32835261.16. Nourazari S, Davis SR, Granovsky R, Austin R, Straff DJ, Joseph JW, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2021; 42:203–210. PMID: 33279331.17. Chun SY, Kim HJ, Kim HB. The effect of COVID-19 pandemic on the length of stay and outcomes in the emergency department. Clin Exp Emerg Med. 2022; 9(2):128–133. PMID: 35843613.18. Kim C, Lee J, Cho Y, Oh J, Kang H, Lim TH, et al. The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department. Clin Exp Emerg Med. 2023; 10(1):92–98. PMID: 36652942.19. Fu XY, Shen XF, Cheng YR, Zhou MY, Ye L, Feng ZH, et al. Effect of COVID-19 outbreak on the treatment time of patients with acute ST-segment elevation myocardial infarction. Am J Emerg Med. 2021; 44:192–197. PMID: 33039221.20. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020; 41(22):2083–2088. PMID: 32412631.21. Gu S, Dai Z, Shen H, Bai Y, Zhang X, Liu X, et al. Delayed stroke treatment during COVID-19 pandemic in China. Cerebrovasc Dis. 2021; 50(6):715–721. PMID: 34247153.22. Chang H, Yu JY, Yoon SY, Hwang SY, Yoon H, Cha WC, et al. Impact of COVID-19 pandemic on the overall diagnostic and therapeutic process for patients of emergency department and those with acute cerebrovascular disease. J Clin Med. 2020; 9(12):3842. PMID: 33256204.23. Lee CK, Meng SW, Lee MH, Chen HC, Wang CL, Wang HN, et al. The impact of door-to-electrocardiogram time on door-to-balloon time after achieving the guideline-recommended target rate. PLoS One. 2019; 14(9):e0222019. PMID: 31498823.24. Kim H, Lee SW. Impacts of pain on clinical features and outcomes in patients presenting to the emergency department with acute myocardial infarction. J Korean Soc Emerg Med. 2005; 16(5):511–518.25. Kim MW, Oh SH, Park KN, Lee JM, Lee YM, Kim HJ, et al. Effect of emergency bell on door to ECG time in walk-in patients presented to emergency department with chest pain. Qual Improv Health Care. 2014; 20(1):12–24.26. Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, et al. The comparison of emergency medical service responses to and outcomes of out-of-hospital cardiac arrest before and during the COVID-19 pandemic in an area of Korea. J Korean Med Sci. 2021; 36(36):e255. PMID: 34519188.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of an Infection Control Protocol for Coronavirus Disease in Emergency Mechanical Thrombectomy
- Impact of the COVID-19 Pandemic on Patient Delay and Clinical Outcomes for Patients With Acute Myocardial Infarction
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- Comparison of Prognosis According to the Use of Emergency Medical Services in Patients with ST-Segment Elevation Myocardial Infarction
- Regional Cardiocerebrovascular Center Project in the Treatment of Acute Myocardial Infarction