Korean J Gastroenterol.
2023 Dec;82(6):295-299. 10.4166/kjg.2023.105.
Plug-Assisted Retrograde Transvenous Obliteration for the Treatment of Duodenal Variceal Bleeding - A Case Report and Literature Review
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 2Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2549813
- DOI: http://doi.org/10.4166/kjg.2023.105
Abstract
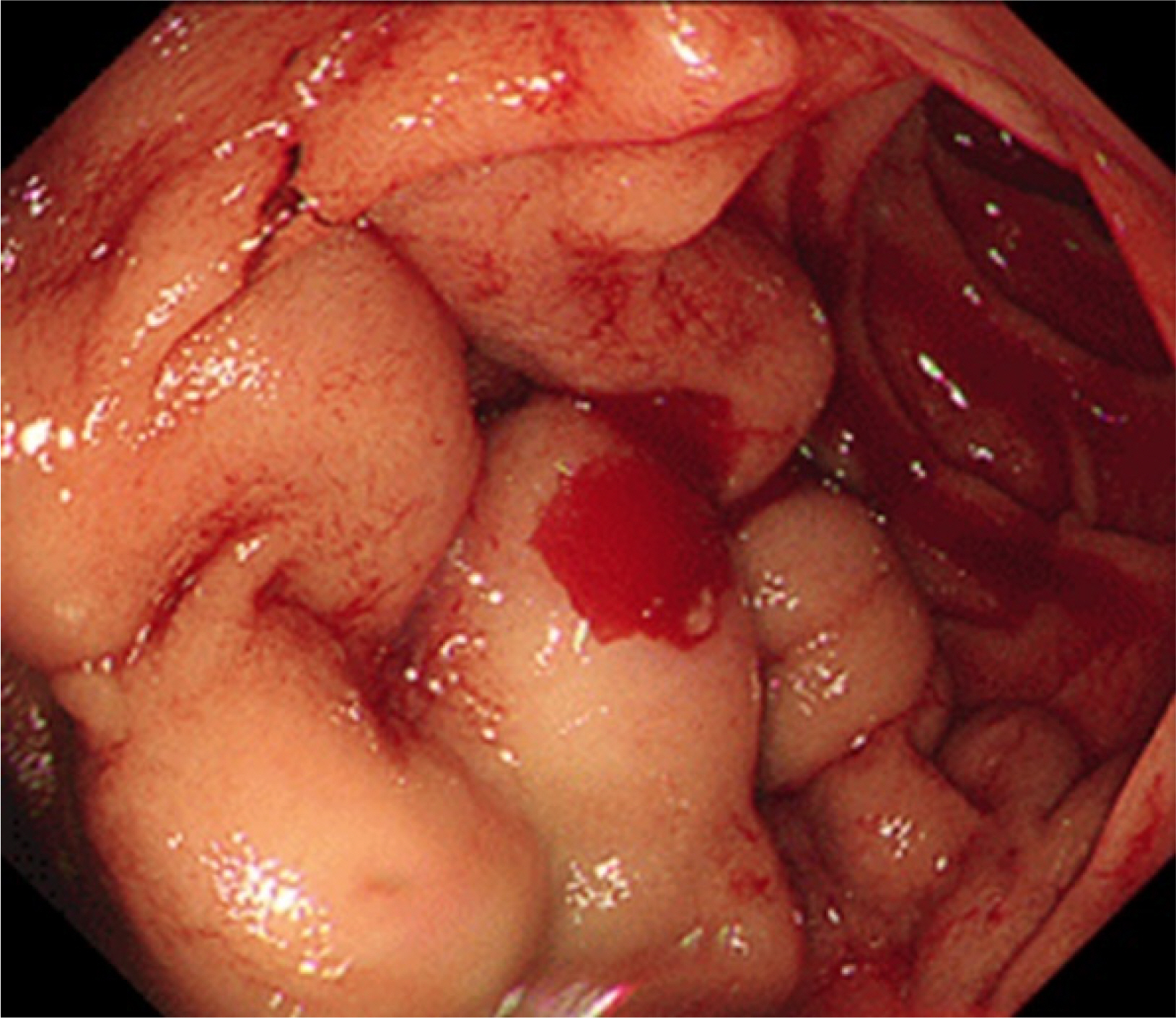
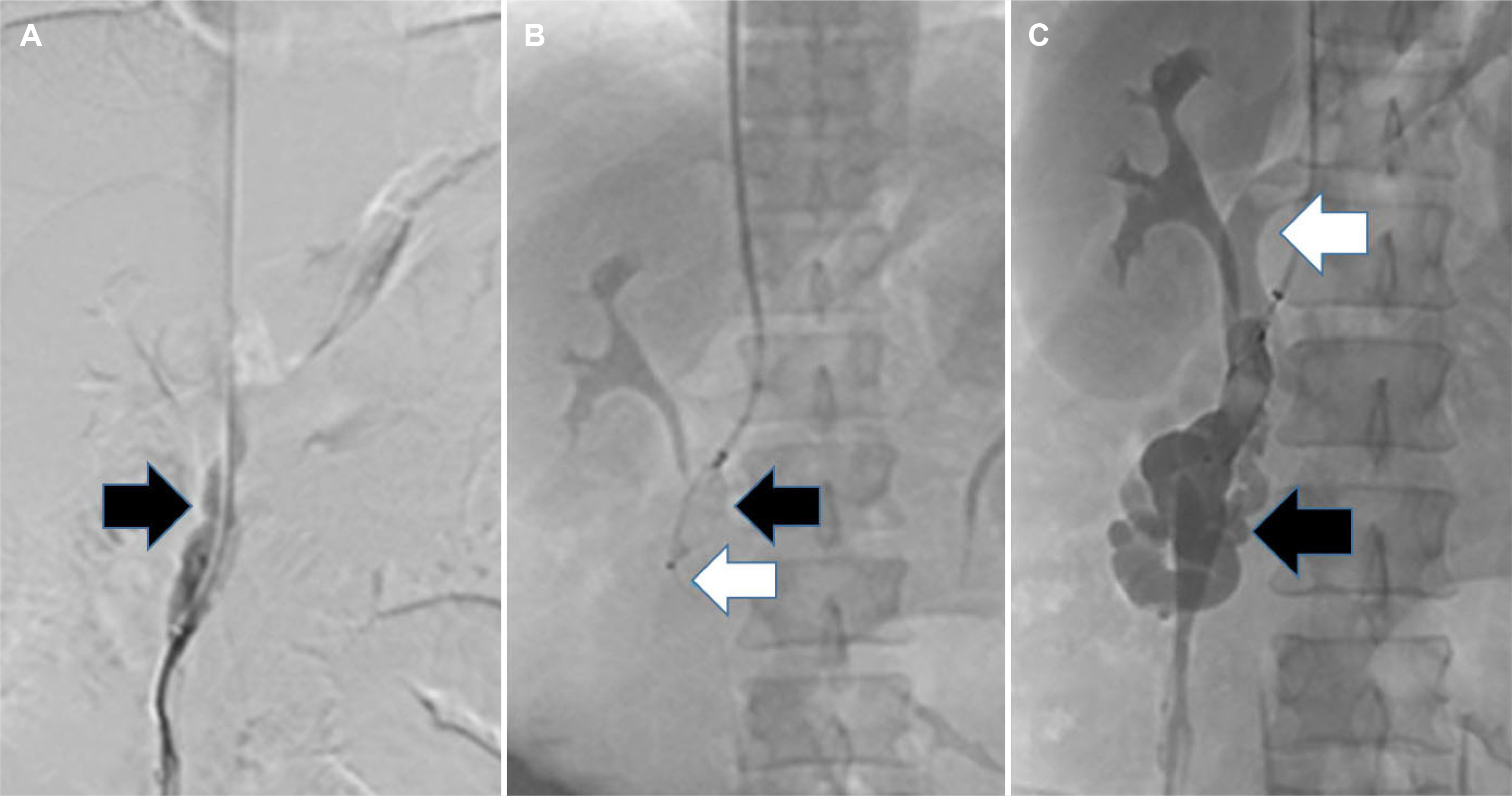
- Duodenal varices are uncommon complications of portal hypertension. Although duodenal variceal bleeding is infrequent, it is a life-threatening condition with a high mortality rate. Non-surgical methods for duodenal variceal bleeding include endoscopic band ligation, endoscopic sclerotherapy, transjugular intrahepatic portosystemic shunt, and retrograde transvenous obliteration. On the other hand, an optimal treatment strategy for this rare condition has not been established. A 38-year-old male with a history of alcoholic liver cirrhosis presented with hematemesis. An emergency esophagogastroduodenoscopy (EGD) revealed large, multiple varices in the second portion of the duodenum, and plug-assisted retrograde transvenous obliteration (PARTO) was performed accordingly. Gastrointestinal bleeding was resolved after the procedure. Follow-up EGD conducted after 11 weeks revealed complete obliteration of the previously observed duodenal varices. PARTO may be considered a viable option for treating duodenal variceal bleeding.
Keyword
Figure
Reference
-
1. D'Imperio N, Piemontese A, Baroncini D, et al. 1996; Evaluation of undiluted N-butyl-2-cyanoacrylate in the endoscopic treatment of upper gastrointestinal tract varices. Endoscopy. 28:239–243. DOI: 10.1055/s-2007-1005435. PMID: 8739740.2. Norton ID, Andrews JC, Kamath PS. 1998; Management of ectopic varices. Hepatology. 28:1154–1158. DOI: 10.1002/hep.510280434. PMID: 9755256.3. Hashimoto R, Sofue K, Takeuchi Y, Shibamoto K, Arai Y. 2013; Successful balloon-occluded retrograde transvenous obliteration for bleeding duodenal varices using cyanoacrylate. World J Gastroenterol. 19:951–954. DOI: 10.3748/wjg.v19.i6.951. PMID: 23429766. PMCID: PMC3574895.4. Jang JY, Jeon UB, Kim JH, et al. 2021; Plug-assisted retrograde transvenous obliteration via gastrocaval shunt for the gastric variceal bleeding: A case report. Medicine (Baltimore). 100:e28107. DOI: 10.1097/MD.0000000000028107. PMID: 34889266. PMCID: PMC8663895.5. Philips CA, Arora A, Shetty R, Kasana V. 2016; A comprehensive review of portosystemic collaterals in cirrhosis: Historical aspects, anatomy, and classifications. Int J Hepatol. 2016:6170243. DOI: 10.1155/2016/6170243. PMID: 28074159. PMCID: PMC5198179.6. Bosch A, Marsano L, Varilek GW. 2003; Successful obliteration of duodenal varices after endoscopic ligation. Dig Dis Sci. 48:1809–1812. DOI: 10.1023/A:1025402411557. PMID: 14561006.7. Yipeng W, Cong L, Sizhe W, Chenkai H, Anjiang W, Xuan Z. 2021; Effectiveness and safety of endoscopic treatment for duodenal variceal bleeding: a systematic review. Eur J Gastroenterol Hepatol. 33:461–469. DOI: 10.1097/MEG.0000000000001819. PMID: 32576766. PMCID: PMC7908861.8. Liu Y, Yang J, Wang J, et al. 2009; Clinical characteristics and endoscopic treatment with cyanoacrylate injection in patients with duodenal varices. Scand J Gastroenterol. 44:1012–1016. DOI: 10.1080/00365520903030787. PMID: 19513934.9. Hwang SW, Sohn JH, Kim TY, et al. 2014; Long-term successful treatment of massive distal duodenal variceal bleeding with balloon-occluded retrograde transvenous obliteration. Korean J Gastroenterol. 63:248–252. DOI: 10.4166/kjg.2014.63.4.248. PMID: 24755751.10. Kim DJ, Darcy MD, Mani NB, et al. 2018; Modified balloon-occluded retrograde transvenous obliteration (BRTO) techniques for the treatment of gastric varices: Vascular plug-assisted retrograde transvenous obliteration (PARTO)/Coil-assisted retrograde transvenous obliteration (CARTO)/Balloon-occluded antegrade transvenous obliteration (BATO). Cardiovasc Intervent Radiol. 41:835–847. DOI: 10.1007/s00270-018-1896-1. PMID: 29417267.11. Korean Association for the Study of the Liver (KASL). 2020; KASL clinical practice guidelines for liver cirrhosis: Varices, hepatic encephalopathy, and related complications. Clin Mol Hepatol. 26:83–127. DOI: 10.3350/cmh.2019.0010n. PMID: 31918536. PMCID: PMC7160350.12. Jonnalagadda SS, Quiason S, Smith OJ. 1998; Successful therapy of bleeding duodenal varices by TIPS after failure of sclerotherapy. Am J Gastroenterol. 93:272–274. DOI: 10.1111/j.1572-0241.1998.270_3.x. PMID: 9468260.13. Hwang GL, Sze DY. 2017; Survival in cirrhotic patients with high MELD scores: The TIPping point. Dig Dis Sci. 62:296–298. DOI: 10.1007/s10620-016-4376-y. PMID: 27830408.14. Angermayr B, Cejna M, Karnel F, et al. 2003; Child-Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosystemic shunt. Gut. 52:879–885. DOI: 10.1136/gut.52.6.879. PMID: 12740346. PMCID: PMC1773665.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plug-Assisted Retrograde Transvenous Obliteration for the Treatment of Gastric Varix with Both Gastrorenal and Gastrocaval Shunts: A Case Report
- Successful Treatment of Duodenal Variceal Bleeding with Coil-Assisted Retrograde Transvenous Obliteration: A Case Report
- Plug-Assisted Retrograde Transvenous Obliteration of Spontaneous Splenorenal Shunt for Refractory Hepatic Encephalopathy: Case Series
- Percutaneous transvenous obliteration for duodenal variceal bleeding using micro-balloon catheter and n-butyl cyanoacrylate: A case report
- Off-label plug-assisted retrograde transvenous obliteration of a giant gastrorenal shunt: A report of two cases