Child Kidney Dis.
2023 Dec;27(2):105-110. 10.3339/ckd.23.011.
Hypokalemia as a risk factor for prolonged QT interval and arrhythmia in inherited salt-losing tubulopathy
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Republic of Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Republic of Korea
- KMID: 2549741
- DOI: http://doi.org/10.3339/ckd.23.011
Abstract
- Purpose
To analyze electrocardiograms (ECGs) of patients with a salt-losing tubulopathy (SLT) and to determine the frequency and risk factors for long QT and arrhythmia.
Methods
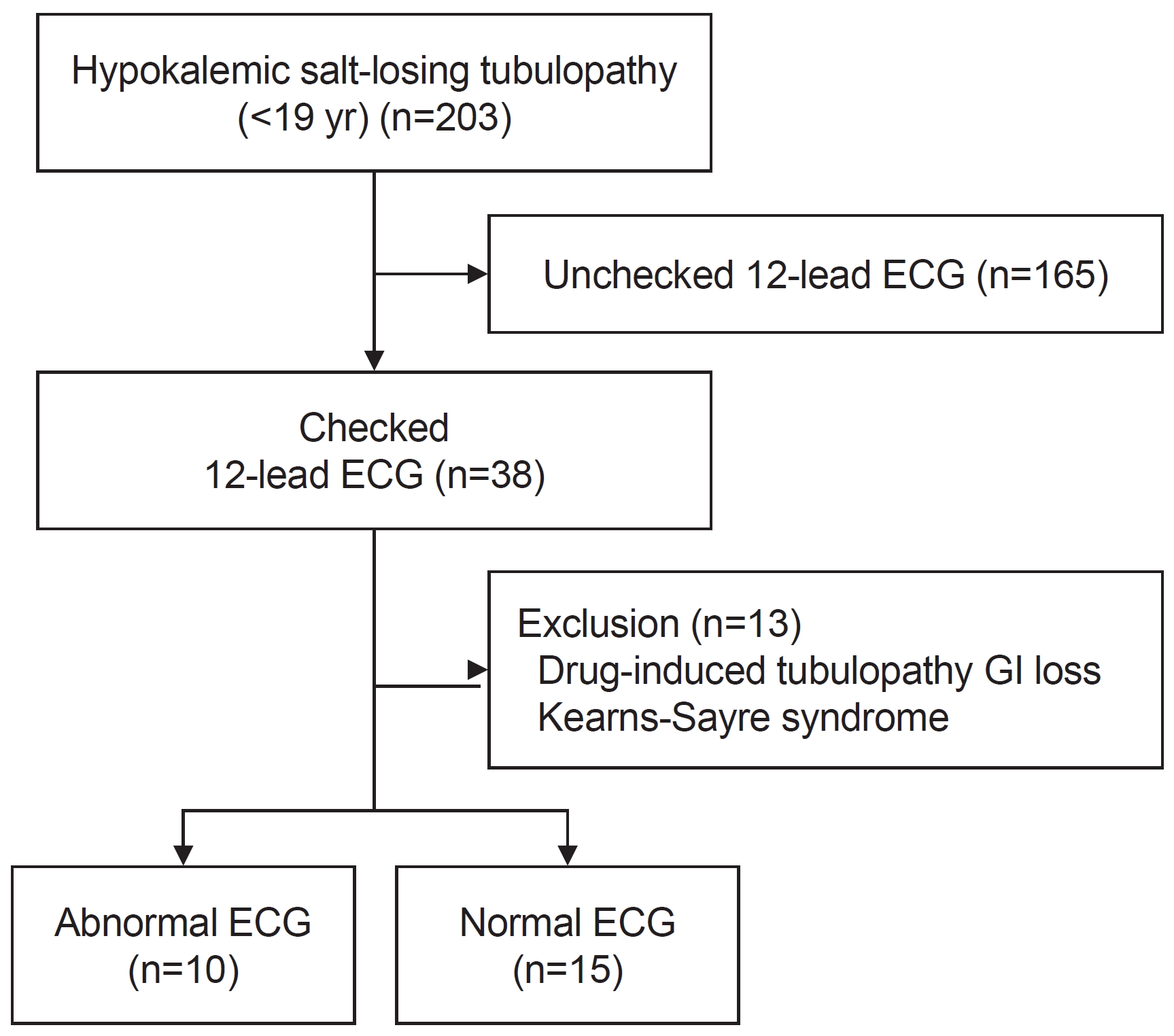
A total of 203 patients aged <19 years with SLT, specifically Bartter syndrome and Gitelman syndrome, who had a 12-lead ECG were included in this retrospective study. We analyzed the presence of an arrhythmia or prolonged corrected QT (QTc) on ECGs obtained for these patients. Demographic and laboratory data were compared between patients with abnormal and normal ECG findings.
Results
Out of the 203 SLT patients, 38 (18.7%) underwent electrocardiography and 10 (40.0%) of 25 patients with inherited SLT had abnormal ECG findings, including prolonged QTc and arrhythmias. The abnormal ECG group had significantly lower serum potassium levels than the normal group (median [interquartile range]: 2.50 mmol/L [2.20–2.83] vs. 2.90 mmol/L [2.70–3.30], p=0.036), whereas other serum chemistry values did not show significant differences. The cutoff level for a significant difference in QTc interval was serum potassium level <2.50 mmol/L. One cardiac event occurred in a 13-year-old boy, who developed paroxysmal supraventricular tachycardia and underwent cardiac ablation. No sudden cardiac deaths occurred in this cohort.
Conclusions
The incidence of ECG abnormalities in patients with inherited SLT was 40.0%, whereas the ECG screening rate was relatively low (18.7%). Therefore, we recommend ECG screening in patients with inherited SLT, especially in those with serum potassium level <2.50 mmol/L.
Figure
Reference
-
References
1. Konrad M, Nijenhuis T, Ariceta G, Bertholet-Thomas A, Calo LA, Capasso G, et al. Diagnosis and management of Bartter syndrome: executive summary of the consensus and recommendations from the European Rare Kidney Disease Reference Network Working Group for Tubular Disorders. Kidney Int. 2021; 99:324–35.
Article2. Gitelman HJ, Graham JB, Welt LG. A new familial disorder characterized by hypokalemia and hypomagnesemia. Trans Assoc Am Physicians. 1966; 79:221–35.3. Blanchard A, Bockenhauer D, Bolignano D, Calo LA, Cosyns E, Devuyst O, et al. Gitelman syndrome: consensus and guidance from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2017; 91:24–33.
Article4. Zelikovic I. Hypokalaemic salt-losing tubulopathies: an evolving story. Nephrol Dial Transplant. 2003; 18:1696–700.
Article5. Podrid PJ. Potassium and ventricular arrhythmias. Am J Cardiol. 1990; 65:33E–44E.
Article6. Bettinelli A, Tosetto C, Colussi G, Tommasini G, Edefonti A, Bianchetti MG. Electrocardiogram with prolonged QT interval in Gitelman disease. Kidney Int. 2002; 62:580–4.
Article7. Cortesi C, Lava SA, Bettinelli A, Tammaro F, Giannini O, Caiata-Zufferey M, et al. Cardiac arrhythmias and rhabdomyolysis in Bartter-Gitelman patients. Pediatr Nephrol. 2010; 25:2005–8.
Article8. Pachulski RT, Lopez F, Sharaf R. Gitelman's not-so-benign syndrome. N Engl J Med. 2005; 353:850–1.
Article9. Malafronte C, Borsa N, Tedeschi S, Syren ML, Stucchi S, Bianchetti MG, et al. Cardiac arrhythmias due to severe hypokalemia in a patient with classic Bartter disease. Pediatr Nephrol. 2004; 19:1413–5.
Article10. Nakane E, Kono T, Sasaki Y, Tokaji Y, Ito T, Sohmiya K, et al. Gitelman's syndrome with exercise-induced ventricular tachycardia. Circ J. 2004; 68:509–11.
Article11. Scognamiglio R, Negut C, Calo LA. Aborted sudden cardiac death in two patients with Bartter's/Gitelman's syndromes. Clin Nephrol. 2007; 67:193–7.
Article12. Hacihamdioglu DO, Fidanci K, Kilic A, Gok F, Topaloglu R. QT and JT dispersion and cardiac performance in children with neonatal Bartter syndrome: a pilot study. Pediatr Nephrol. 2013; 28:1969–74.
Article13. Goldenberg I, Moss AJ. Long QT syndrome. J Am Coll Cardiol. 2008; 51:2291–300.
Article14. Scognamiglio R, Calo LA, Negut C, Coccato M, Mormino P, Pessina AC. Myocardial perfusion defects in Bartter and Gitelman syndromes. Eur J Clin Invest. 2008; 38:888–95.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Attack of Ventricular Arrhythmia Caused by Low Potassium Level in Hemodialysis Patients
- QTc Interval Prolongation with Increasing Body Mass Index
- A Case of Congenital Long QT Syndrome Associated with Deafness and Syncope
- Ventricular arrhythmia in patients with prolonged QT interval during liver transplantation: two cases report
- Analysis of QTc Prolongation Related to Arrhythmia in Patients with Aconitine Intoxication