Ann Rehabil Med.
2023 Dec;47(6):502-510. 10.5535/arm.23060.
A Pulmonary Telerehabilitation Program Improves Exercise Capacity and Quality of Life in Young Females Post-COVID-19 Patients
- Affiliations
-
- 1Department of Physiology, College of Medicine, Qassim University, Buraidah, Kingdom of Saudi Arabia
- 2Department of Physical Therapy, College of Medical Rehabilitation, Qassim University, Buraidah, Kingdom of Saudi Arabia
- 3Department of Physical Therapy for Surgery, Faculty of Physical Therapy, Cairo University, Giza, Egypt
- KMID: 2549731
- DOI: http://doi.org/10.5535/arm.23060
Abstract
Objective
To examine the impact of telerehabilitation training on exercise capacity, lung function, and health-related quality of life (HRQOL) in comparison to no rehabilitation for post-COVID-19 symptoms in adult females.
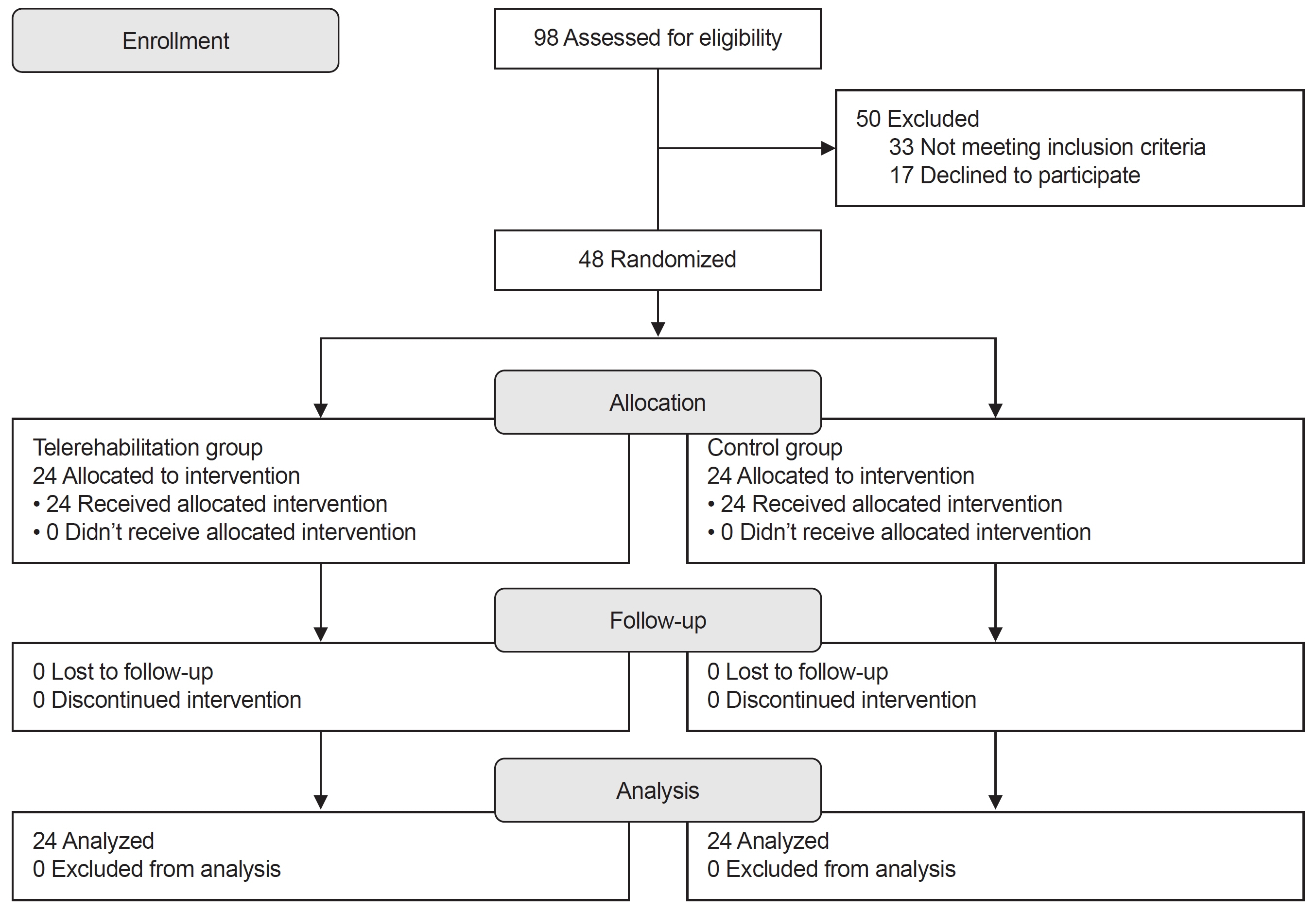
Methods
A randomized controlled trial of 48 females after mild to moderate COVID-19 survival were equally and randomly assigned to one of two groups: intervention group or control group. Three sessions per week for 6 weeks of a telerehabilitation program provided via a smartphone to the intervention group. Spirometry was used to quantify lung function, a 6-minute walk test (6MWT) measured in meters to measure exercise capacity, and the Short Form Health Survey-36 was used to assess HRQOL.
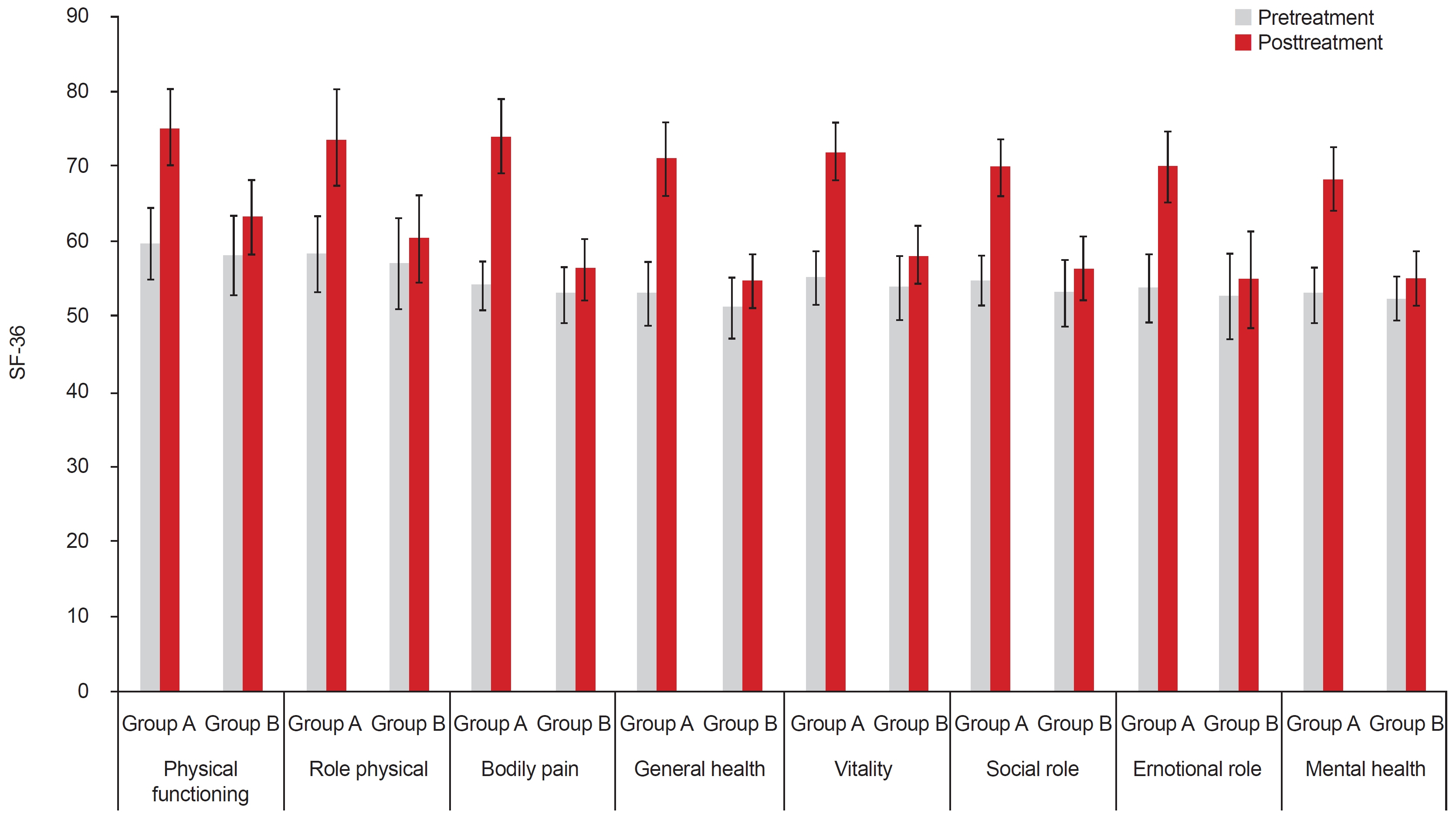
Results
After treatment, there was no statistically significant difference in forced vital capacity (FVC) or forced expiratory volume in 1 second (FEV1) between groups (p>0.05), but the 6MWT of the intervention group increased significantly more than that of the control group (p=0.001). The percent of change in 6MWT for the intervention group and control group was 14.22% and 4.21%, respectively. After therapy, the intervention group’s HRQOL significantly improved when compared to the control group’s (p=0.001).
Conclusion
This study showed that a telerehabilitation programs improved exercise capacity and HRQOL in young females post-COVID-19 compared to no rehabilitation.
Figure
Reference
-
1. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021; 27:601–15.
Article2. Gluckman TJ, Bhave NM, Allen LA, Chung EH, Spatz ES, Ammirati E, et al. 2022 ACC Expert Consensus Decision Pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection, and return to play: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022; 79:1717–56.3. Raman B, Bluemke DA, Lüscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022; 43:1157–72.
Article4. National Institute for Health and Care Excellence (NICE). COVID-19 rapid guideline: managing the long-term effects of COVID-19 [Internet]. NICE;2020 [cited 2022 Aug 25]. Available from: https://www.nice.org.uk/guidance/ng188.5. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV; WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022; 22:e102–7.
Article6. Compagno S, Palermi S, Pescatore V, Brugin E, Sarto M, Marin R, et al. Physical and psychological reconditioning in long COVID syndrome: results of an out-of-hospital exercise and psychological - based rehabilitation program. Int J Cardiol Heart Vasc. 2022; 41:101080.
Article7. Taribagil P, Creer D, Tahir H. ‘Long COVID’ syndrome. BMJ Case Rep. 2021; 14:e241485.
Article8. Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med 2021;9:1275-87. Erratum in: Lancet Respir Med. 2022; 10:e9.9. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021; 397:220–32.
Article10. Holland AE, Hill CJ, Rochford P, Fiore J, Berlowitz DJ, McDonald CF. Telerehabilitation for people with chronic obstructive pulmonary disease: feasibility of a simple, real time model of supervised exercise training. J Telemed Telecare. 2013; 19:222–6.
Article11. Spruit MA, Holland AE, Singh SJ, Tonia T, Wilson KC, Troosters T. COVID-19: interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force. Eur Respir J. 2020; 56:2002197.
Article12. Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020; 54:949–59.
Article13. Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022; 28:611.e9–611.e16.
Article14. Hanson SW, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022; 328:1604–15.
Article15. World Health Organization (WHO). COVID-19 clinical management: living guidance, 25 January 2021. WHO;2021. p. 1–81.16. Sharma BB, Singh V. Pulmonary rehabilitation: an overview. Lung India. 2011; 28:276–84.
Article17. American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 9th ed. Lippincott Williams & Wilkins;2013. p. 1–456.18. Riebe D, Ehrman JK, Liguori G, Magal M. General principles of exercise prescription. In : . ACSM’s guidelines for exercise testing and prescription. 10th ed. Lippincott Williams & Wilkins;2018. p. 143–79.19. Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957; 35:307–15.20. Fish DE, Krabak BJ, Johnson-Greene D, DeLateur BJ. Optimal resistance training: comparison of DeLorme with Oxford techniques. Am J Phys Med Rehabil. 2003; 82:903–9.21. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014; 44:1428–46.
Article22. Rochester CL, Vogiatzis I, Holland AE, Lareau SC, Marciniuk DD, Puhan MA, et al. An Official American Thoracic Society/European Respiratory Society Policy Statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. 2015; 192:1373–86.
Article23. Sheikh KA, Yagoub U, Elsatouhy M, Al Sanosi R, Mohamud SA. Reliability and validity of the Arabic version of the SF-36 health survey questionnaire in population of Khat Chewers—Jazan Region-Kingdom of Saudi Arabia. Appl Res Qual Life. 2015; 10:1–13.
Article24. Colas C, Bayle M, Labeix P, Botelho-Nevers E, Gagneux-Brunon A, Cazorla C, et al. Management of long COVID-The CoviMouv’ pilot study: importance of adapted physical activity for prolonged symptoms following SARS-CoV2 infection. Front Sports Act Living. 2022; 4:877188.
Article25. Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021; 6:e005427.
Article26. Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network - United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:993–8.
Article27. Rinaldo RF, Mondoni M, Parazzini EM, Pitari F, Brambilla E, Luraschi S, et al. Deconditioning as main mechanism of impaired exercise response in COVID-19 survivors. Eur Respir J. 2021; 58:2100870.
Article28. Skjørten I, Ankerstjerne OAW, Trebinjac D, Brønstad E, Rasch-Halvorsen Ø, Einvik G, et al. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur Respir J. 2021; 58:2100996.29. Lerum TV, Aaløkken TM, Brønstad E, Aarli B, Ikdahl E, Lund KMA, et al. Dyspnoea, lung function and CT findings 3 months after hospital admission for COVID-19. Eur Respir J. 2021; 57:2003448.30. Sonnweber T, Sahanic S, Pizzini A, Luger A, Schwabl C, Sonnweber B, et al. Cardiopulmonary recovery after COVID-19: an observational prospective multicentre trial. Eur Respir J. 2021; 57:2003481.31. Clavario P, De Marzo V, Lotti R, Barbara C, Porcile A, Russo C, et al. Cardiopulmonary exercise testing in COVID-19 patients at 3 months follow-up. Int J Cardiol. 2021; 340:113–8.32. Peçanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020; 318:H1441–6.
Article33. Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011; 364:1293–304.
Article34. Li J, Xia W, Zhan C, Liu S, Yin Z, Wang J, et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax. 2022; 77:697–706.
Article35. Nopp S, Moik F, Klok FA, Gattinger D, Petrovic M, Vonbank K, et al. Outpatient pulmonary rehabilitation in patients with Long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration. 2022; 101:593–601.
Article36. Gloeckl R, Leitl D, Jarosch I, Schneeberger T, Nell C, Stenzel N, et al. Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res. 2021; 7:00108–2021.
Article37. Lu Y, Li P, Li N, Wang Z, Li J, Liu X, et al. Effects of home-based breathing exercises in subjects with COPD. Respir Care. 2020; 65:377–87.
Article38. Rooney S, Webster A, Paul L. Systematic review of changes and recovery in physical function and fitness after severe acute respiratory syndrome-related coronavirus infection: implications for COVID-19 rehabilitation. Phys Ther. 2020; 100:1717–29.
Article39. Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020; 99:769–74.
Article40. Besnier F, Bérubé B, Malo J, Gagnon C, Grégoire CA, Juneau M, et al. Cardiopulmonary rehabilitation in long-COVID-19 patients with persistent breathlessness and fatigue: the COVID-rehab study. Int J Environ Res Public Health. 2022; 19:4133.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of an Inpatient Pulmonary Rehabilitation Program on Dyspnea, Exercise Capacity, and Health Related Quality of Life for Patients with Chronic Lung Disease
- Pulmonary Function, Functional Capacity, Respiratory, and Locomotor Muscle Strength after Severe to Critically Ill COVID-19: A Long-Term Study
- Pulmonary Rehabilitation in Chronic Obstructive Pulmonary Disease (COPD)
- The Effects of Self-Efficacy Promoting Pulmonary Rehabilitation Program in Out-Patients with Chronic Obstructive Pulmonary Disease
- Effects of the Respiration Exercise Program through the Pan-flute on the Physiological and Psychological Status of the Elderly