J Neurocrit Care.
2023 Dec;16(2):59-68. 10.18700/jnc.230037.
Management strategies for refractory status epilepticus
- Affiliations
-
- 1Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- KMID: 2549482
- DOI: http://doi.org/10.18700/jnc.230037
Abstract
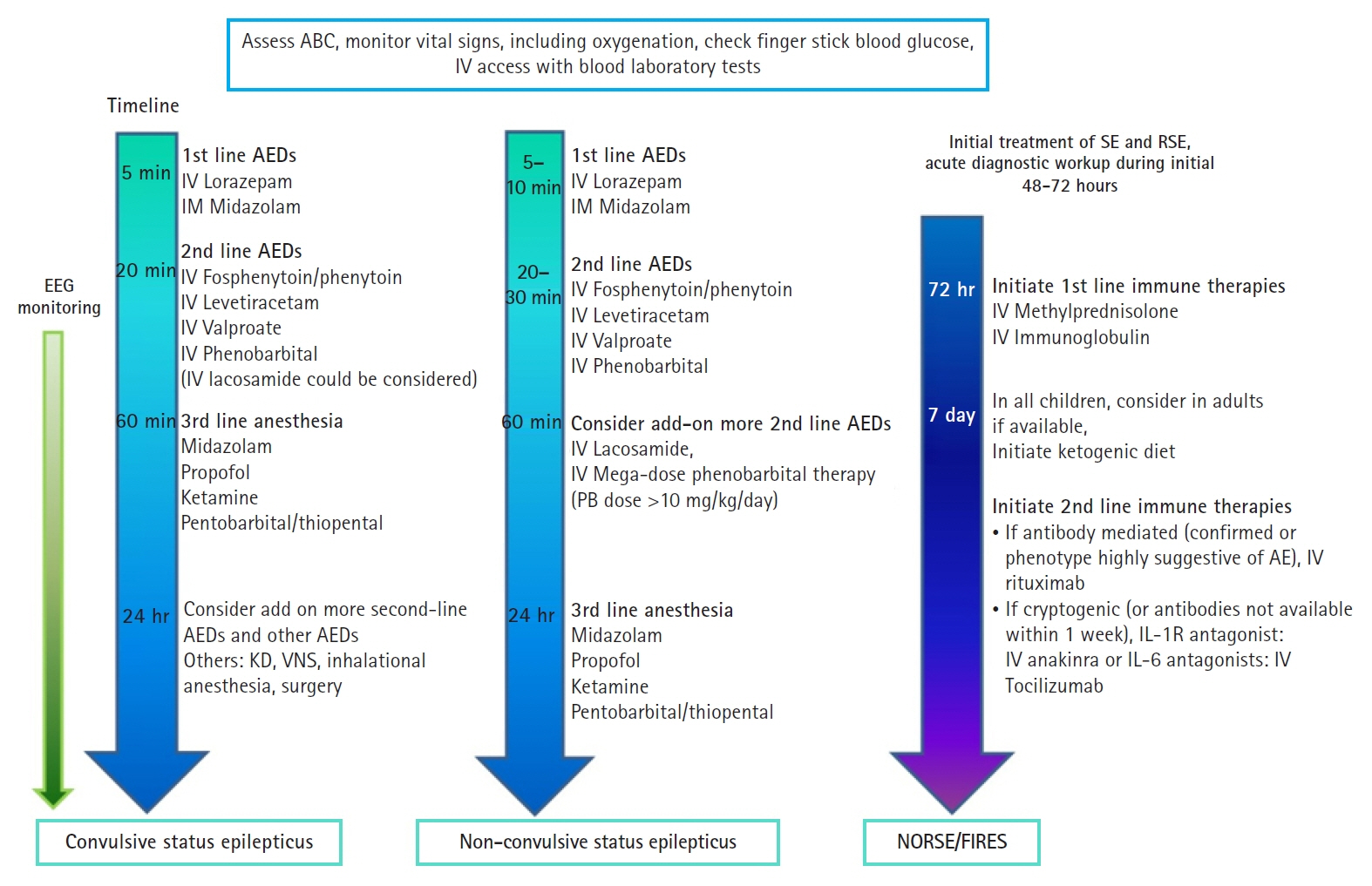
- Refractory status epilepticus (RSE) is defined as the persistence of either clinical or electrographic seizures despite the administration of appropriate doses of an initial benzodiazepine and suitable second-line antiepileptic drugs (AEDs). The Neurocritical Care Society and the American Epilepsy Society have proposed a treatment paradigm for the management of convulsive status epilepticus (CSE). The third-line therapy in refractory CSE may involve general anesthesia using intravenous midazolam, propofol, or other agents, while recent evidence supports the use of ketamine to manage RSE in both adults and children. However, although these treatment strategies are frequently employed in nonconvulsive status epilepticus (NCSE), the efficacy of AEDs and anesthetics in NCSE has not been thoroughly investigated. Recent evidence has demonstrated the safety and efficacy of newer AEDs, including levetiracetam and lacosamide, in the treatment of status epilepticus (SE) and RSE, which also encompasses NCSE. Use of multiple combinations of various intravenous AEDs can also be considered in NCSE before the administration of general anesthesia. In addition, AEDs alone exhibit limited effectiveness in managing SE for new-onset RSE (NORSE) and its subset, febrile infection-related epilepsy syndrome. Therefore, in cases of refractory status, it is imperative to explore treatment options beyond AEDs, including immunotherapy and the incorporation of a ketogenic diet. The present review suggests treatment approaches for RSE based on subgroups, including CSE, NCSE, and NORSE. A discussion of recent clinical studies on AEDs and anesthetics in the management of RSE, as well as proposed treatment methods for NORSE, is also provided.
Keyword
Figure
Reference
-
1. Legriel S, Oddo M, Brophy GM. What's new in refractory status epilepticus? Intensive Care Med. 2017; 43:543–6.2. Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011; 134:2802–18.3. Amengual-Gual M, Sánchez Fernández I, Wainwright MS. Novel drugs and early polypharmacotherapy in status epilepticus. Seizure. 2019; 68:79–88.4. Joshi S, Rajasekaran K, Hawk KM, Chester SJ, Goodkin HP. Status epilepticus: role for etiology in determining response to benzodiazepines. Ann Neurol. 2018; 83:830–41.5. Burman RJ, Rosch RE, Wilmshurst JM, Sen A, Ramantani G, Akerman CJ, et al. Why won't it stop? The dynamics of benzodiazepine resistance in status epilepticus. Nat Rev Neurol. 2022; 18:428–41.6. Fujikawa DG. Starting ketamine for neuroprotection earlier than its current use as an anesthetic/antiepileptic drug late in refractory status epilepticus. Epilepsia. 2019; 60:373–80.7. Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016; 16:48–61.8. Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012; 17:3–23.9. Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, et al. A definition and classification of status epilepticus: report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015; 56:1515–23.10. Trinka E, Leitinger M. Which EEG patterns in coma are nonconvulsive status epilepticus? Epilepsy Behav. 2015; 49:203–22.11. Hirsch LJ, Fong MW, Leitinger M, LaRoche SM, Beniczky S, Abend NS, et al. American Clinical Neurophysiology Society's standardized critical care EEG terminology: 2021 version. J Clin Neurophysiol. 2021; 38:1–29.12. Olney JW, Collins RC, Sloviter RS. Excitotoxic mechanisms of epileptic brain damage. Adv Neurol. 1986; 44:857–77.13. Meldrum BS. Excitotoxicity and selective neuronal loss in epilepsy. Brain Pathol. 1993; 3:405–12.14. Avdic U, Ahl M, Chugh D, Ali I, Chary K, Sierra A, et al. Nonconvulsive status epilepticus in rats leads to brain pathology. Epilepsia. 2018; 59:945–58.15. Cheng JY. Latency to treatment of status epilepticus is associated with mortality and functional status. J Neurol Sci. 2016; 370:290–5.16. Gutiérrez-Viedma Á, Parejo-Carbonell B, Cuadrado ML, Serrano-García I, Abarrategui B, García-Morales I. The relevance of timing in nonconvulsive status epilepticus: a series of 38 cases. Epilepsy Behav. 2018; 82:11–6.17. Power KN, Gramstad A, Gilhus NE, Engelsen BA. Adult nonconvulsive status epilepticus in a clinical setting: semiology, aetiology, treatment and outcome. Seizure. 2015; 24:102–6.18. Hirsch LJ, Gaspard N, van Baalen A, Nabbout R, Demeret S, Loddenkemper T, et al. Proposed consensus definitions for new-onset refractory status epilepticus (NORSE), febrile infection-related epilepsy syndrome (FIRES), and related conditions. Epilepsia. 2018; 59:739–44.19. Gaspard N, Hirsch LJ, Sculier C, Loddenkemper T, van Baalen A, Lancrenon J, et al. New-onset refractory status epilepticus (NORSE) and febrile infection-related epilepsy syndrome (FIRES): state of the art and perspectives. Epilepsia. 2018; 59:745–52.20. Wickstrom R, Taraschenko O, Dilena R, Payne ET, Specchio N, Nabbout R, et al. International consensus recommendations for management of New Onset Refractory Status Epilepticus (NORSE) incl. Febrile Infection-Related Epilepsy Syndrome (FIRES): statements and supporting evidence. Epilepsia. 2022; 63:2840–64.21. Hawkes MA, Hocker SE. Systemic complications following status epilepticus. Curr Neurol Neurosci Rep. 2018; 18:7.22. Busl KM, Bleck TP. Neurogenic pulmonary edema. Crit Care Med. 2015; 43:1710–5.23. Sutter R, Tschudin-Sutter S, Grize L, Fuhr P, Bonten MJ, Widmer AF, et al. Associations between infections and clinical outcome parameters in status epilepticus: a retrospective 5-year cohort study. Epilepsia. 2012; 53:1489–97.24. Sutter R, Marsch S, Fuhr P, Rüegg S. Mortality and recovery from refractory status epilepticus in the intensive care unit: a 7-year observational study. Epilepsia. 2013; 54:502–11.25. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis. An overview for clinicians. Crit Care. 2005; 9:158–69.26. Minicucci F, Ferlisi M, Brigo F, Mecarelli O, Meletti S, Aguglia U, et al. Management of status epilepticus in adults: position paper of the Italian League against Epilepsy. Epilepsy Behav. 2020; 102:106675.27. Chiu WT, Campozano V, Schiefecker A, Rodriguez DR, Ferreira D, Headlee A, et al. Management of refractory status epilepticus: an international cohort study (MORSE CODe) analysis of patients managed in the ICU. Neurology. 2022; 99:e1191–201.28. Gaspard N, Foreman B, Judd LM, Brenton JN, Nathan BR, McCoy BM, et al. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia. 2013; 54:1498–503.29. Espinosa L, Gomez M, Zamora A, Molano-Franco D. Refractory and super-refractory status epilepticus and evidence for the use of ketamine: a scope review. J Neurocrit Care. 2023; 16:1–9.30. Groth CM, Droege CA, Connor KA, Kaukeinen K, Acquisto NM, Chui SH, et al. Multicenter retrospective review of ketamine use in the ICU. Crit Care Explor. 2022; 4:e0633.31. Byun JI. Management of convulsive status epilepticus: recent updates. Encephalitis. 2023; 3:39–43.32. Jacobwitz M, Mulvihill C, Kaufman MC, Gonzalez AK, Resendiz K, MacDonald JM, et al. Ketamine for management of neonatal and pediatric refractory status epilepticus. Neurology. 2022; 99:e1227–38.33. Alkhachroum A, Der-Nigoghossian CA, Mathews E, Massad N, Letchinger R, Doyle K, et al. Ketamine to treat super-refractory status epilepticus. Neurology. 2020; 95:e2286–94.34. Hurth KP, Jaworski A, Thomas KB, Kirsch WB, Rudoni MA, Wohlfarth KM. The reemergence of ketamine for treatment in critically ill adults. Crit Care Med. 2020; 48:899–911.35. Choi JW, Shin JW. Early combination therapy of ketamine and midazolam in patients with refractory status epilepticus in hemodynamic unstable state. J Epilepsy Res. 2021; 11:150–3.36. Sabharwal V, Ramsay E, Martinez R, Shumate R, Khan F, Dave H, et al. Propofol-ketamine combination therapy for effective control of super-refractory status epilepticus. Epilepsy Behav. 2015; 52:264–6.37. Trinka E, Leitinger M. Management of status epilepticus, refractory status epilepticus, and super-refractory status epilepticus. Continuum (Minneap Minn). 2022; 28:559–602.38. Muhlhofer WG, Layfield S, Lowenstein D, Lin CP, Johnson RD, Saini S, et al. Duration of therapeutic coma and outcome of refractory status epilepticus. Epilepsia. 2019; 60:921–34.39. Migdady I, Rosenthal ES, Cock HR. Management of status epilepticus: a narrative review. Anaesthesia. 2022; 77 Suppl 1:78–91.40. Kapur J, Elm J, Chamberlain JM, Barsan W, Cloyd J, Lowenstein D, et al. Randomized trial of three anticonvulsant medications for status epilepticus. N Engl J Med. 2019; 381:2103–13.41. Lyttle MD, Rainford NE, Gamble C, Messahel S, Humphreys A, Hickey H, et al. Levetiracetam versus phenytoin for second-line treatment of paediatric convulsive status epilepticus (EcLiPSE): a multicentre, open-label, randomised trial. Lancet. 2019; 393:2125–34.42. Dalziel SR, Borland ML, Furyk J, Bonisch M, Neutze J, Donath S, et al. Levetiracetam versus phenytoin for second-line treatment of convulsive status epilepticus in children (ConSEPT): an open-label, multicentre, randomised controlled trial. Lancet. 2019; 393:2135–45.43. Husain AM, Lee JW, Kolls BJ, Hirsch LJ, Halford JJ, Gupta PK, et al. Randomized trial of lacosamide versus fosphenytoin for nonconvulsive seizures. Ann Neurol. 2018; 83:1174–85.44. Panda PK, Panda P, Dawman L, Sharawat IK. Efficacy of lacosamide and phenytoin in status epilepticus: a systematic review. Acta Neurol Scand. 2021; 144:366–74.45. Vossler DG, Bainbridge JL, Boggs JG, Novotny EJ, Loddenkemper T, Faught E, et al. Treatment of refractory convulsive status epilepticus: a comprehensive review by the American Epilepsy Society Treatments Committee. Epilepsy Curr. 2020; 20:245–64.46. Trinka E. Phenobarbital in status epilepticus: rediscovery of an effective drug. Epilepsy Behav. 2023; 141:109104.47. Brigo F, Del Giovane C, Nardone R, Trinka E, Lattanzi S. Intravenous antiepileptic drugs in adults with benzodiazepine-resistant convulsive status epilepticus: a systematic review and network meta-analysis. Epilepsy Behav. 2019; 101:106466.48. Byun JI, Chu K, Sunwoo JS, Moon J, Kim TJ, Lim JA, et al. Mega-dose phenobarbital therapy for super-refractory status epilepticus. Epileptic Disord. 2015; 17:444–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Status Epilepticus and Beyond: A Clinical Review of Status Epilepticus and an Update on Current Management Strategies in Super-refractory Status Epilepticus
- Sevoflurane for the Management of Refractory Status Epilepticus : A case report
- Anesthetic experience for performing a cesarean section for a woman with refractory status epilepticus: A case report
- Febrile Infection-Related Epilepsy Syndrome: Refractory Status Epilepticus and Management Strategies
- Garcinia Cambogia-Induced Refractory Status Epilepticus