J Dent Rehabil Appl Sci.
2023 Jun;39(2):61-68. 10.14368/jdras.2023.39.2.61.
Influence of tongue pressure on the obturator prosthesis for soft palate defects: a 3D-FEA study
- Affiliations
-
- 1Dental Research Institute and Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea
- 2Dental Research Institute and Department of Oral Anatomy, School of Dentistry, Seoul National University, Seoul, Republic of Korea
- KMID: 2549273
- DOI: http://doi.org/10.14368/jdras.2023.39.2.61
Abstract
- Purpose
The purpose of the study was to analyze how swallowing tongue pressure affects the biomechanics of a velopharyngeal obturator prosthesis and compare its displacement across different occlusal rest positions.
Materials and Methods
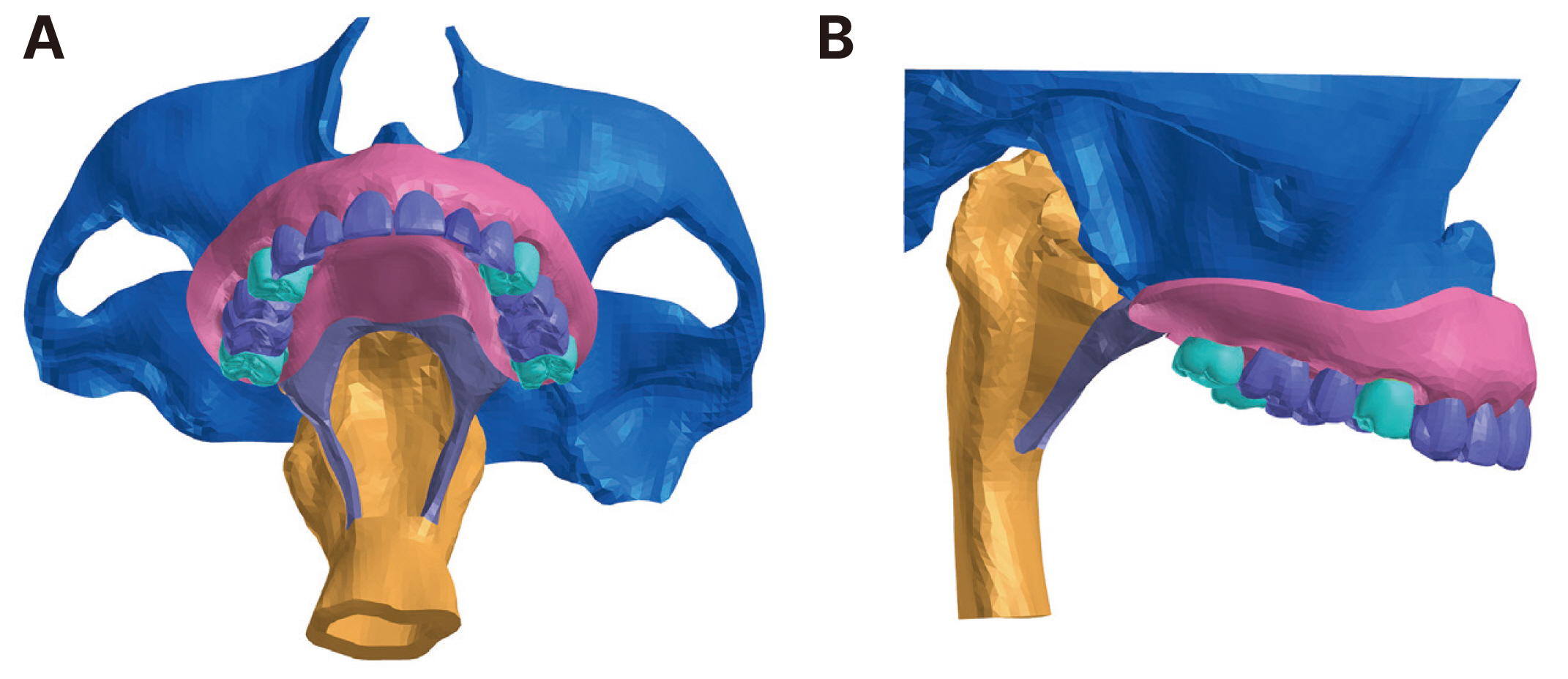
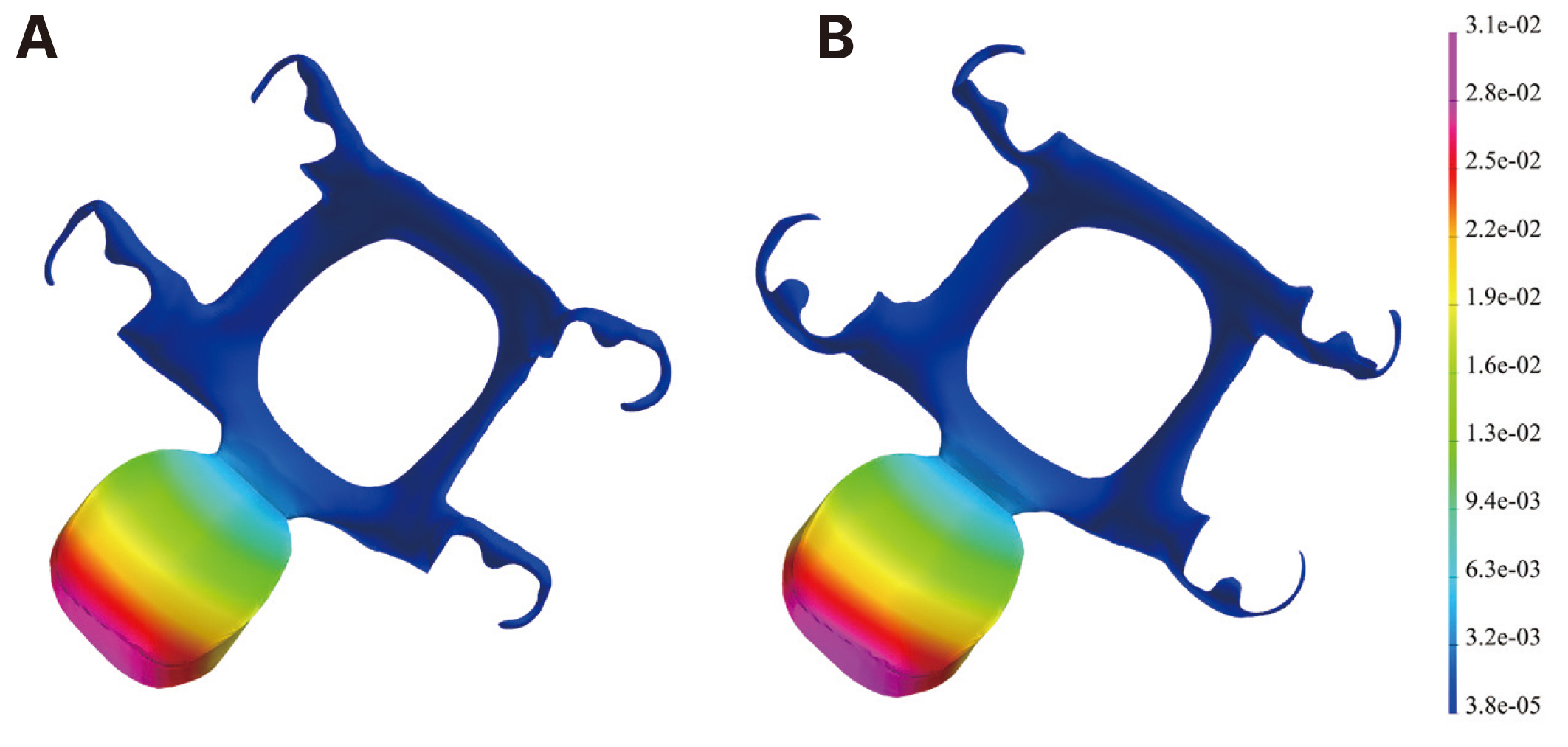
A 3D geometric model consisting of the maxilla, teeth, soft palate, and a portion of the pharynx was developed based on the CBCT and MRI data. A defect was created by the resection of soft palate portion. Two experimental models were generated based on two different velopharyngeal obturator designs: one “with mesial occlusal rests” (Model 1) and the other with “distal occlusal rests” (Model 2). A pressure of 25 kPa was applied at the surface of the bulb of the obturator prosthesis opposite the base of the tongue to simulate tongue pressure during swallowing. The maximum von-Mises stress and displacement values of two types of obturator prostheses were analyzed and compared.
Results
The maximum von-Mises stress in the metal framework, located at the posterior palatal strap, was slightly higher in model 1 (64.9 MPa) than in model 2 (54.2 MPa). In both models, the acrylic resin obturator bulb exhibited a maximum stress value of 4.3 MPa. There was no significant difference in prosthesis displacement between the two models, with 31.3 µm for model 1 and 33.6 µm for model 2.
Conclusion
Swallowing tongue pressure had a minor impact on the biomechanics of a velopharyngeal obturator prosthesis, and distal occlusal rests showed a slightly better biomechanical response compared to mesial occlusal rests.
Figure
Reference
-
References
1. Gaziano JE. 2002; Evaluation and management of oropharyngeal dysphagia in head and neck cancer. Cancer Control. 9:400–9. DOI: 10.1177/107327480200900505. PMID: 12410179.
Article2. Boseley ME, Hartnick CJ. 2004; Assessing the outcome of surgery to correct velopharyngeal insufficiency with the pediatric voice outcomes survey. Int J Pediatr Otorhinolaryngol. 68:1429–33. DOI: 10.1016/j.ijporl.2004.06.002. PMID: 15488976.
Article3. Thomas L, Jones TM, Tandon S, Katre C, Lowe D, Rogers SN. 2008; An evaluation of the University of Washington quality of life swallowing domain following oropharyngeal cancer. Eur Arch Otorhinolaryngol. 265 Suppl 1:S29–37. DOI: 10.1007/s00405-007-0470-2. PMID: 17952450.
Article4. Barata LF, de Carvalho GB, Carrara-de Angelis E, de Faria JCM, Kowalski LP. 2013; Swallowing, speech and quality of life in patients undergoing resection of soft palate. Eur Arch Otorhinolaryngol. 270:305–12. DOI: 10.1007/s00405-012-2006-7. PMID: 22526573.
Article5. Aramany MA, Myers EN. 1978; Prosthetic reconstruction following resection of the hard and soft palate. J Prosthet Dent. 40:174–8. DOI: 10.1016/0022-3913(78)90013-6. PMID: 278835.
Article6. Shetty NB, Shetty S, Nagraj E, D'Souza R, Shetty O. 2014; Management of velopharyngeal defects: A review. J Clin Diagn Res. 8:283–7. DOI: 10.7860/JCDR/2014/6220.4188. PMID: 24783161. PMCID: PMC4003670. PMID: 29b86e91cedb4dc9938604da638d2d39.
Article7. Saunders TR, Oliver NA. 1993; A speech-aid prosthesis for anterior maxillary implant-supported prostheses. J Prosthet Dent. 70:546–7. DOI: 10.1016/0022-3913(93)90271-O. PMID: 8277446.
Article8. Abreu A, Levy D, Rodriguez E, Rivera I. 2007; Oral rehabilitation of a patient with complete unilateral cleft lip and palate using an implant-retained speech-aid prosthesis: Clinical report. Cleft Palate Craniofac J. 44:673–7. DOI: 10.1597/06-169.1. PMID: 18177197.
Article9. Raol N, Hartnick CJ. 2015; Anatomy and physiology of velopharyngeal closure and insufficiency. Adv Otorhinolaryngol. 76:1–6. DOI: 10.1159/000368003. PMID: 25733226.
Article10. McConnel FM. 1988; Analysis of pressure generation and bolus transit during pharyngeal swallowing. Laryngoscope. 98:71–8. DOI: 10.1288/00005537-198801000-00015. PMID: 3336265.
Article11. Jacob RF, King G. 1990; Indirect retainers in soft palate obturator design. J Prosthet Dent. 63:311–5. DOI: 10.1016/0022-3913(90)90203-O. PMID: 2407829.
Article12. Tuna SH, Pekkan G, Gumus HO, Aktas A. 2010; Prosthetic rehabilitation of velopharyngeal insufficiency: pharyngeal obturator prostheses with different retention mechanisms. Eur J Dent. 4:81–7. DOI: 10.1055/s-0039-1697813. PMID: 20046485. PMCID: PMC2798795.
Article13. Collin JD, Main BGJ, Barber AJ, Thomas SJ. 2014; Airway compromise by dislodged obturator in a patient with severe trismus. J Prosthet Dent. 112:83–5. DOI: 10.1016/j.prosdent.2013.08.021. PMID: 24423458.
Article14. Hohmann A, Kober C, Young P, Dorow C, Geiger M, Boryor A, Sander FM, Sander C, Sander FG. 2011; Influence of different modeling strategies for the periodontal ligament on finite element simulation results. Am J Orthod Dentofacial Orthop. 139:775–83. DOI: 10.1016/j.ajodo.2009.11.014. PMID: 21640884.
Article15. Tachimura T, Nohara K, Wada T. 2000; Effect of placement of a speech appliance on levator veli palatini muscle activity during speech. Cleft Palate Craniofac J. 37:478–82. DOI: 10.1597/1545-1569_2000_037_0478_eopoas_2.0.co_2. PMID: 11034030.
Article16. de Sousa AA, Mattos BSC. 2014; Finite element analysis of stability and functional stress with implant-supported maxillary obturator prostheses. J Prosthet Dent. 112:1578–84. DOI: 10.1016/j.prosdent.2014.06.020. PMID: 25277029.
Article17. Rubin C, Krishnamurthy N, Capilouto E, Yi H. 1983; Stress analysis of the human tooth using a three-dimensional finite element model. J Dent Res. 62:82–6. DOI: 10.1177/00220345830620021701. PMID: 6571871.18. Reinhardt RA, Pao YC, Krejci RF. 1984; Periodontal ligament stresses in the initiation of occlusal traumatism. J Periodontal Res. 19:238–46. DOI: 10.1111/j.1600-0765.1984.tb00815.x. PMID: 6235340.
Article19. Rees JS, Jacobsen PH. 1997; Elastic modulus of the periodontal ligament. Biomaterials. 18:995–9. DOI: 10.1016/S0142-9612(97)00021-5. PMID: 9212195.
Article20. Miyashita ER, Mattos BSC, Noritomi PY, Navarro H. 2012; Finite element analysis of maxillary bone stress caused by Aramany class IV obturator prostheses. J Prosthet Dent. 107:336–42. DOI: 10.1016/S0022-3913(12)60086-9. PMID: 22546312.
Article21. Haddad SMH, Dhaliwal SS, Rotenberg BW, Samani A, Ladak HM. 2018; Estimation of the Young's moduli of fresh human oropharyngeal soft tissues using indentation testing. J Mech Behav Biomed Mater. 86:352–8. DOI: 10.1016/j.jmbbm.2018.07.004. PMID: 30007184.
Article22. Birch MJ, odon PD Sr. 2009; Biomechanical properties of the human soft palate. Cleft Palate Craniofac J. 46:268–74. DOI: 10.1597/08-012.1. PMID: 19642755.
Article23. Carrigy NB, Carey JP, Martin AR, Remmers JE, Zareian A, Topor Z, Grosse J, Noga M, Finlay WH. 2016; Simulation of muscle and adipose tissue deformation in the passive human pharynx. Comput Methods Biomech Biomed Engin. 19:780–8. DOI: 10.1080/10255842.2015.1062477. PMID: 26213804.
Article24. Kim SM, Kim SJ, Bae HS, Choi BC, Mun JH. 2004; A nondestructive diagnostic modeling for muscular dysfunction of human pharynx using finite element method. Key Eng Mater. 270-273:2061–6. DOI: 10.4028/www.scientific.net/KEM.270-273.2061.
Article25. Ha SR, Kim SH, Lee JB, Han JS, Yeo IS, Yoo SH, Kim HK. 2016; Biomechanical three-dimensional finite element analysis of monolithic zirconia crown with different cement thickness. Ceram Int. 42:14928–36. DOI: 10.1016/j.ceramint.2016.06.133.
Article26. Heo KH, Lim YJ, Kim MJ, Kwon HB. 2018; Three-dimensional finite element analysis of the splinted implant prosthesis in a reconstructed mandible. J Adv Prosthodont. 10:138–46. DOI: 10.4047/jap.2018.10.2.138. PMID: 29713435. PMCID: PMC5917106.
Article27. Eom JW, Lim YJ, Kim MJ, Kwon HB. 2017; Three-dimensional finite element analysis of implant-assisted removable partial dentures. J Prosthet Dent. 117:735–42. DOI: 10.1016/j.prosdent.2016.09.021. PMID: 27914668.
Article28. Wang M, Qu X, Cao M, Wang D, Zhang C. 2013; Biomechanical three-dimensional finite element analysis of prostheses retained with/without zygoma implants in maxillectomy patients. J Biomech. 46:1155–61. DOI: 10.1016/j.jbiomech.2013.01.004. PMID: 23395509.
Article29. Shahmiri R, Das R, Aarts JM, Bennani V. 2014; Finite element analysis of an implant-assisted removable partial denture during bilateral loading: Occlusal rests position. J Prosthet Dent. 112:1126–33. DOI: 10.1016/j.prosdent.2014.04.023. PMID: 24951387.30. Qazi WM, Ekberg O, Wiklund J, Kotze R, Stading M. 2019; Assessment of the food-swallowing process using bolus visualisation and manometry simultaneously in a device that models human swallowing. Dysphagia. 34:821–33. DOI: 10.1007/s00455-019-09995-8. PMID: 30840137. PMCID: PMC6825639.
Article31. Al-Toubi AK, Doeltgen SH, Daniels SK, Corey DM, Huckabee ML. 2015; Pharyngeal pressure differences between four types of swallowing in healthy participants. Physiol Behav. 140:132–8. DOI: 10.1016/j.physbeh.2014.12.029. PMID: 25527200.
Article32. Zarrati S, Bahrami M, Heidari F, Kashani J. 2015; Three dimensional finite element analysis of distal abutment stresses of removable partial dentures with different retainer designs. J Dent (Tehran). 12:389–97. PMID: 26884772. PMCID: PMC4754564.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prosthetic rehabilitation by double-processing technique for edentulous patient with soft palate defect after maxillectomy: A case report
- Obturator Prosthesis for Velopharyngeal Insufficiency after Treatment of Soft Palate Cancer: A Case Report
- Palatal obturator restoration of a cleft palate patient with velopharyngeal insufficiency: a clinical report
- Fabrication of closed hollow obturator for hard palate defect patient undergone maxillectomy
- Application of 3D printing technology for rehabilitating maxillary defects