J Korean Med Sci.
2023 Dec;38(48):e404. 10.3346/jkms.2023.38.e404.
Aortic Valve Replacement in the Era of Transcatheter Aortic Valve Implantation: Current Status in Korea
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 5Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2549167
- DOI: http://doi.org/10.3346/jkms.2023.38.e404
Abstract
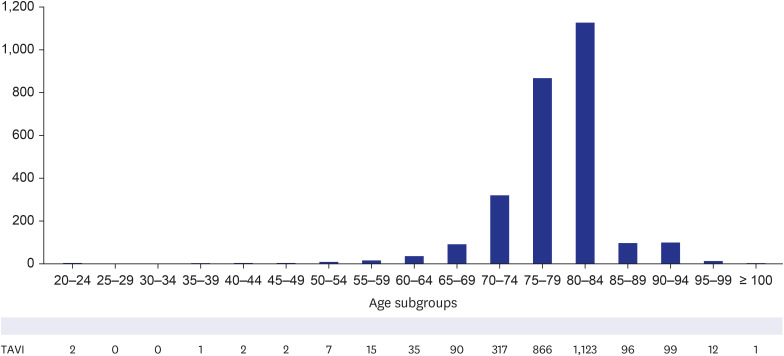
- Background
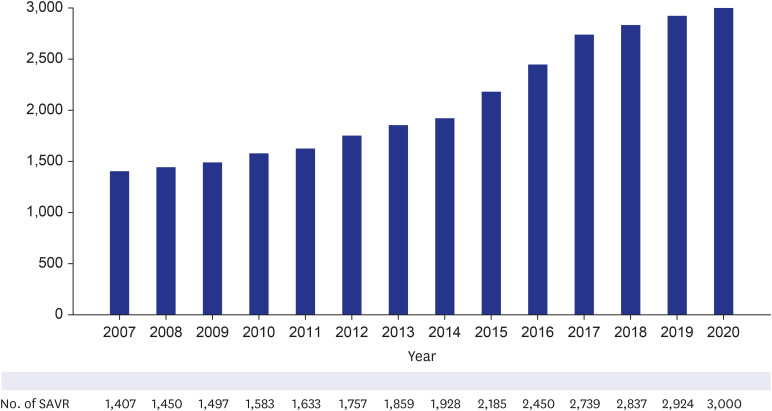
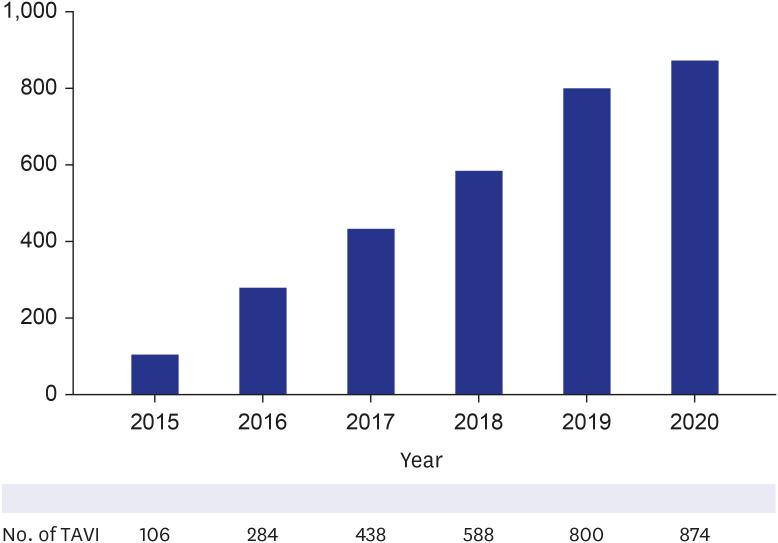
In the era of transcatheter aortic valve implantation, this study was conducted to investigate the current trend of aortic valve procedures in Korea and to evaluate the early and mid-term outcomes of isolated surgical aortic valve replacement (SAVR) using bioprosthetic valves in contemporary Korea.
Methods
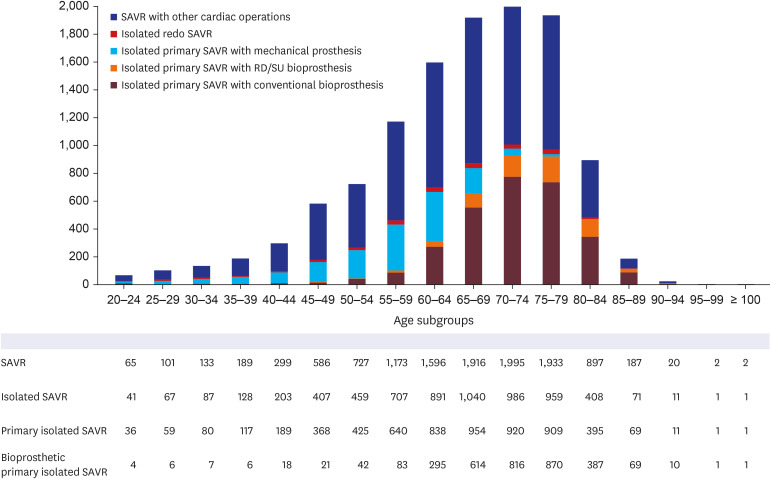
Contemporary outcomes of isolated bioprosthetic SAVR in Korea were analyzed using the datasets on a multicenter basis. Patients who underwent isolated SAVR using bioprostheses from June 2015 to May 2019 were included, and those with concomitant cardiac procedures, SAVR with mechanical valve, or SAVR for infective endocarditis were excluded. A total of 456 patients from 4 large-volume centers were enrolled in this study. Median follow-up duration was 43.4 months. Early postoperative outcomes, mid-term clinical outcomes, and echocardiographic outcomes were evaluated.
Results
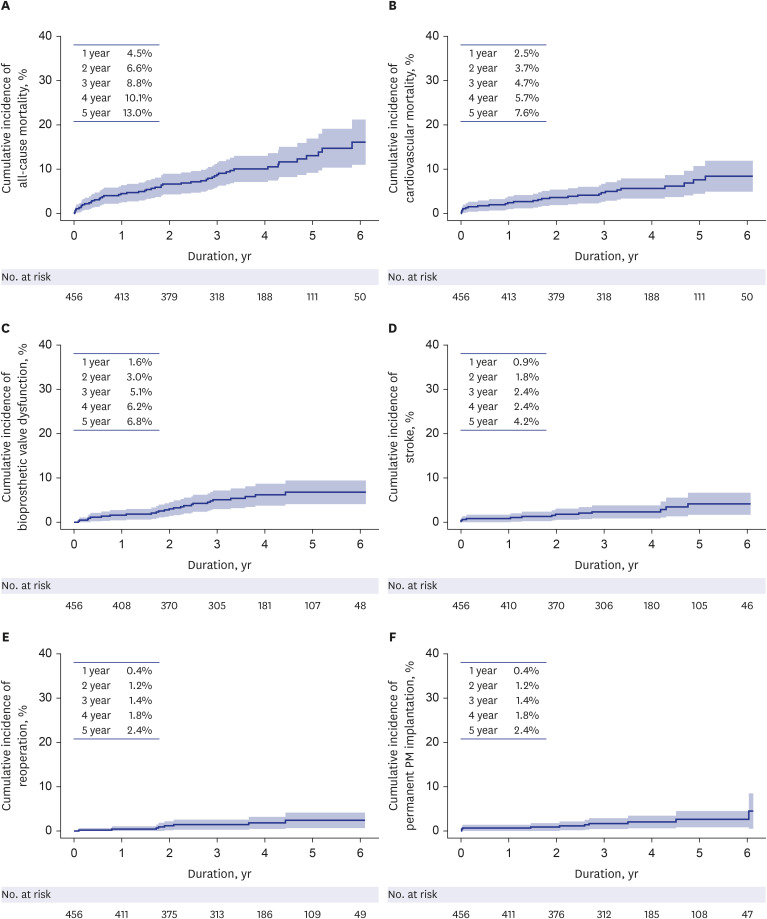
Mean age of the patients was 73.1 ± 7.3 years, and EuroSCORE II was 2.23 ± 2.09. The cardiopulmonary bypass time and aortic cross-clamp times were median 106 and 76 minutes, respectively. SAVR was performed with full median sternotomy (81.8%), right thoracotomy (14.7%), or partial sternotomy (3.5%). Operative mortality was 1.8%. The incidences of stroke and permanent pacemaker implantation were 1.1% and 1.1%, respectively. Paravalvular regurgitation ≥ mild was detected in 2.6% of the patients. Cumulative incidence of all-cause mortality at 5 years was 13.0%. Cumulative incidences of cardiovascular mortality and bioprosthetic valve dysfunction at 5 years were 7.6% and 6.8%, respectively.
Conclusion
The most recent data for isolated SAVR using bioprostheses in Korea resulted in excellent early and mid-term outcomes in a multicenter study.
Keyword
Figure
Reference
-
1. Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM, et al. 5-Year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015; 385(9986):2477–2484. PMID: 25788234.2. Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016; 374(17):1609–1620. PMID: 27040324.
Article3. Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019; 380(18):1695–1705. PMID: 30883058.
Article4. Writing Committee Members. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2021; 77(4):e25–197. PMID: 33342586.
Article5. Sharma T, Krishnan AM, Lahoud R, Polomsky M, Dauerman HL. National trends in TAVR and SAVR for patients with severe isolated aortic stenosis. J Am Coll Cardiol. 2022; 80(21):2054–2056. PMID: 36122626.
Article6. Sedrakyan A, Dhruva SS, Sun T, Mao J, Gaudino MF, Redberg RF. Trends in use of transcatheter aortic valve replacement by age. JAMA. 2018; 320(6):598–600. PMID: 30039166.
Article7. Nguyen V, Michel M, Eltchaninoff H, Gilard M, Dindorf C, Iung B, et al. Implementation of transcatheter aortic valve replacement in France. J Am Coll Cardiol. 2018; 71(15):1614–1627. PMID: 29650117.
Article8. Reinöhl J, Kaier K, Reinecke H, Schmoor C, Frankenstein L, Vach W, et al. Effect of availability of transcatheter aortic-valve replacement on clinical practice. N Engl J Med. 2015; 373(25):2438–2447. PMID: 26672846.
Article9. Ludman PF, Moat N, de Belder MA, Blackman DJ, Duncan A, Banya W, et al. Transcatheter aortic valve implantation in the United Kingdom: temporal trends, predictors of outcome, and 6-year follow-up: a report from the UK Transcatheter Aortic Valve Implantation (TAVI) Registry, 2007 to 2012. Circulation. 2015; 131(13):1181–1190. PMID: 25637628.
Article10. Carroll JD, Mack MJ, Vemulapalli S, Herrmann HC, Gleason TG, Hanzel G, et al. STS-ACC TVT registry of transcatheter aortic valve replacement. J Am Coll Cardiol. 2020; 76(21):2492–2516. PMID: 33213729.
Article11. Kim WJ, Kim YH, Lee JY, Park DW, Kang SJ, Lee SW, et al. Transcatheter aortic valve implantation: early experience in Korea. Korean Circ J. 2012; 42(10):684–691. PMID: 23170096.
Article12. Martinsson A, Nielsen SJ, Milojevic M, Redfors B, Omerovic E, Tønnessen T, et al. Life expectancy after surgical aortic valve replacement. J Am Coll Cardiol. 2021; 78(22):2147–2157. PMID: 34823657.
Article13. VARC-3 Writing Committee. Généreux P, Piazza N, Alu MC, Nazif T, Hahn RT, et al. Valve academic research consortium 3: updated endpoint definitions for aortic valve clinical research. J Am Coll Cardiol. 2021; 77(21):2717–2746. PMID: 33888385.
Article14. Yu CW, Kim WJ, Ahn JM, Kook H, Kang SH, Han JK, et al. Trends and outcomes of transcatheter aortic valve implantation (TAVI) in Korea: the results of the first cohort of Korean TAVI registry. Korean Circ J. 2018; 48(5):382–394. PMID: 29671283.
Article15. Nguyen V, Willner N, Eltchaninoff H, Burwash IG, Michel M, Durand E, et al. Trends in aortic valve replacement for aortic stenosis: a French nationwide study. Eur Heart J. 2022; 43(7):666–679.
Article16. Onorati F, Quintana E, El-Dean Z, Perrotti A, Sponga S, Ruggieri VG, et al. Aortic valve replacement for aortic stenosis in low-, intermediate-, and high-risk patients: preliminary results from a prospective multicenter registry. J Cardiothorac Vasc Anesth. 2020; 34(8):2091–2099. PMID: 32362544.
Article17. Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019; 380(18):1706–1715. PMID: 30883053.
Article18. Barili F, Freemantle N, Folliguet T, Muneretto C, De Bonis M, Czerny M, et al. The flaws in the detail of an observational study on transcatheter aortic valve implantation versus surgical aortic valve replacement in intermediate-risks patients. Eur J Cardiothorac Surg. 2017; 51(6):1031–1035. PMID: 28531333.
Article19. Benedetto U, Sousa-Uva M. Apples, orange, and pears. Transcatheter aortic valve implantation in intermediate risk patients has borne fruit. J Thorac Cardiovasc Surg. 2017; 153(4):821–822. PMID: 28359371.
Article20. Dewey TM, Herbert MA, Prince SL, Bowers BS. Influence of surgical volume on outcomes in low-risk patients undergoing isolated surgical aortic valve replacement. J Thorac Cardiovasc Surg. 2022; 163(6):2046–2052.e2. PMID: 33985812.
Article21. Johnston DR, Mahboubi R, Soltesz EG, Artis AS, Roselli EE, Blackstone EH, et al. Redefining “low risk”: outcomes of surgical aortic valve replacement in low-risk patients in the transcatheter aortic valve replacement era. J Thorac Cardiovasc Surg. 2023; 165(2):591–604.e3. PMID: 36635021.
Article22. Thourani VH, Brennan JM, Edelman JJ, Thibault D, Jawitz OK, Bavaria JE, et al. Association of volume and outcomes in 234 556 patients undergoing surgical aortic valve replacement. Ann Thorac Surg. 2022; 114(4):1299–1306. PMID: 34785247.
Article23. Tokuda Y, Yamamoto H, Miyata H, Usui A, Motomura N. Japan Cardiovascular Surgery Database Organization. Contemporary outcomes of surgical aortic valve replacement in Japan. Circ J. 2020; 84(2):277–282. PMID: 31932559.
Article24. Hiltner E, Erinne I, Singh A, Chen C, Kassotis J, Russo M, et al. In-hospital outcomes of surgical aortic valve replacement at transcatheter valve implantation centers. Am J Cardiol. 2022; 183:78–84. PMID: 36114022.
Article25. Vogt F, Santarpino G, Fujita B, Frerker C, Bauer T, Beckmann A, et al. Surgical aortic valve replacement in patients aged 50-69 years-insights from the German Aortic Valve Registry (GARY). Eur J Cardiothorac Surg. 2022; 62(1):ezac286. PMID: 35567484.
Article26. Ler A, Ying YJ, Sazzad F, Choong AM, Kofidis T. Structural durability of early-generation transcatheter aortic valve replacement valves compared with surgical aortic valve replacement valves in heart valve surgery: a systematic review and meta-analysis. J Cardiothorac Surg. 2020; 15(1):127. PMID: 32513222.
Article27. Kataruka A, Otto CM. Valve durability after transcatheter aortic valve implantation. J Thorac Dis. 2018; 10(Suppl 30):S3629–S3636. PMID: 30505545.
Article28. Santarpino G, Pfeiffer S, Jessl J, Dell’Aquila A, Vogt F, von Wardenburg C, et al. Clinical outcome and cost analysis of sutureless versus transcatheter aortic valve implantation with propensity score matching analysis. Am J Cardiol. 2015; 116(11):1737–1743. PMID: 26433277.
Article29. Schnittman SR, Adams DH, Itagaki S, Toyoda N, Egorova NN, Chikwe J. Bioprosthetic aortic valve replacement: revisiting prosthesis choice in patients younger than 50 years old. J Thorac Cardiovasc Surg. 2018; 155(2):539–547.e9. PMID: 29110948.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expanding transcatheter aortic valve replacement into uncharted indications
- Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
- Recent updates in transcatheter aortic valve implantation
- Echocardiography in Transcatheter Aortic Valve Implantation and Mitral Valve Clip
- Transcatheter Mitral Valve Implantation in Open Heart Surgery: An Off-Label Technique