Arch Hand Microsurg.
2023 Dec;28(4):226-232. 10.12790/ahm.23.0018.
Affordable and reliable three-dimensional printing: a prospective study of seven distal radius fractures
- Affiliations
-
- 1Department of Orthopedics Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Orthopedic Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2548593
- DOI: http://doi.org/10.12790/ahm.23.0018
Abstract
- Purpose
Three-dimensional (3D) printing is now widely available, and its potential applications to surgery are limitless. However, 3D printing is presently performed at only a few large institutions. We developed a 3D printing workflow using an affordable 3D printer and open-source 3D printing software. We tested whether this combination could produce a model that reliably reflects real bone.
Methods
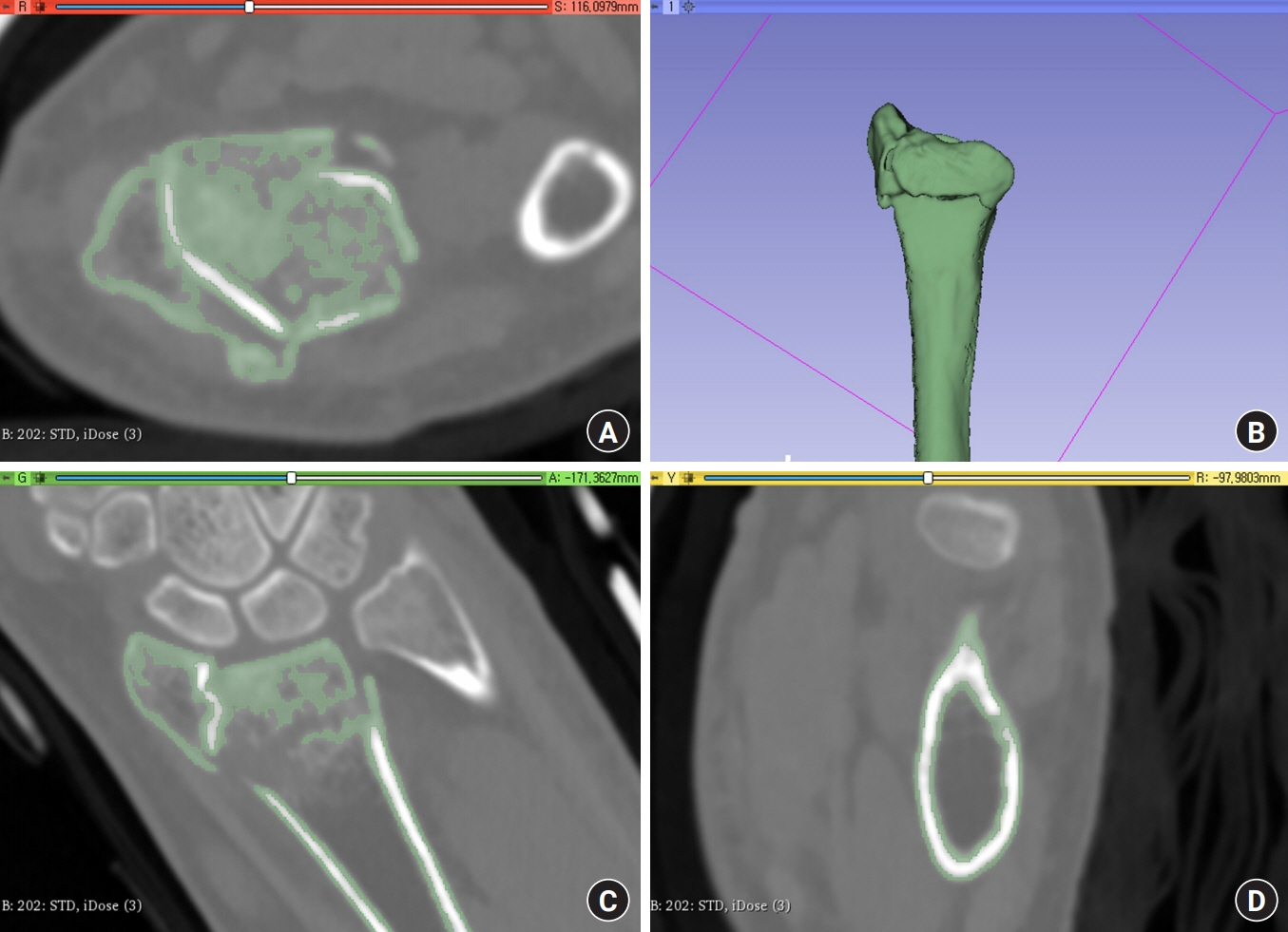
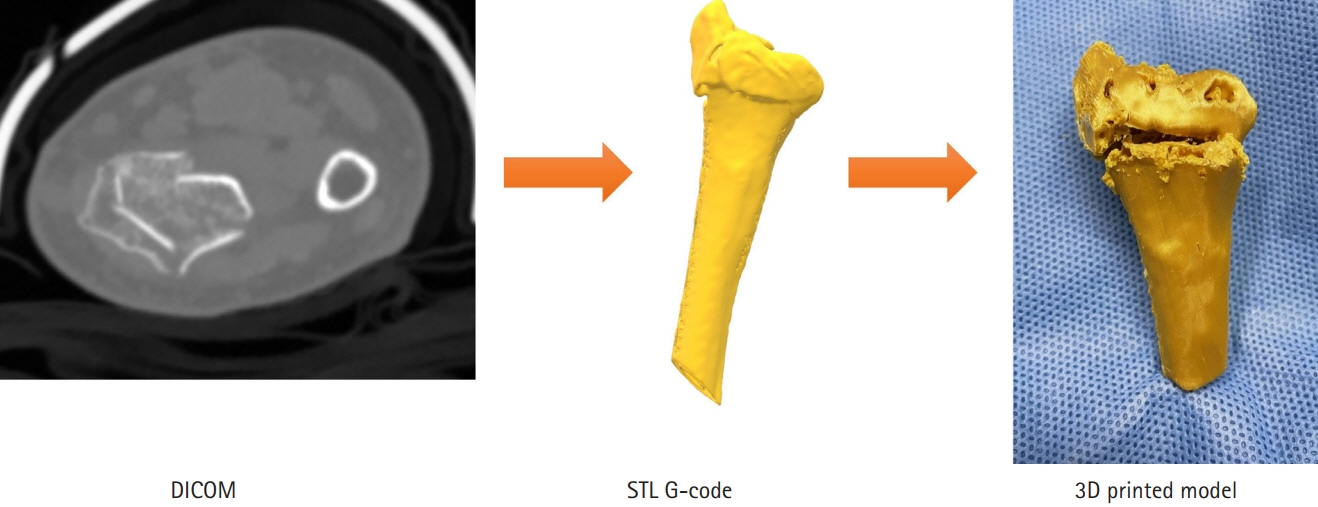
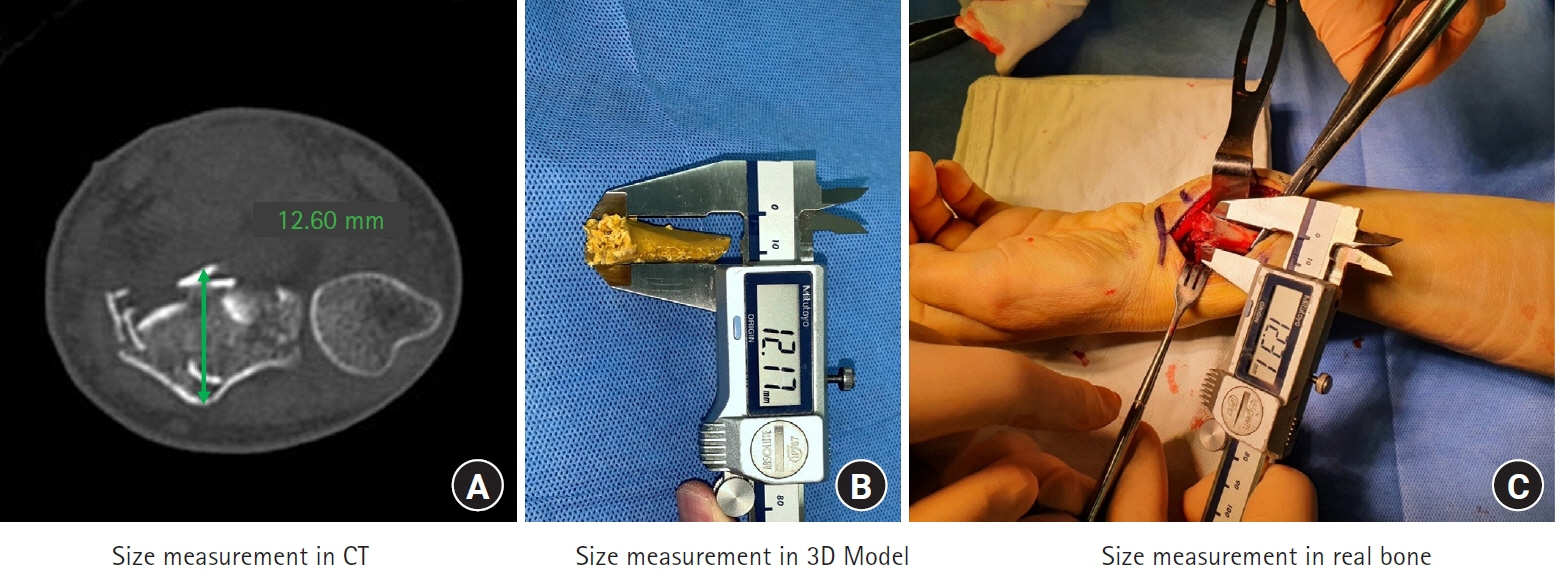
We performed a prospective study with a target sample size of seven. Patients with distal radius fractures were enrolled from October 2021 to February 2022. The 3D-printed models of the fractures were produced using open-source software (3D Slicer [Surgical Planning Laboratory, Harvard Medical School] and Cura [Ultimaker]) and a $600 printer. The anterior-to-posterior (AP) and radial-to-ulnar (RU) widths of the fracture sites were measured on computed tomography (CT) images, in 3D printed models, and in real bones (during surgery). Surgery was simulated using the 3D models; the locations and profiles of implants were compared to those placed during real surgery, which was performed without simulation data.
Results
The fracture AP and RU widths did not differ significantly among the CT, 3D model, and real bone measurements. Interclass correlation coefficients indicated that the measurements were reliable (0.943 [p<0.001] and 0.917 [p<0.001], respectively). When the implant profiles of the simulations and surgical procedures were compared, only the most distal (radial) screws were significantly longer in the simulations (p=0.016). The plate location also differed significantly (p=0.043).
Conclusions
Our 3D printing workflow is affordable yet produces reliable bone models.
Figure
Reference
-
References
1. Skelley NW, Smith MJ, Ma R, Cook JL. Three-dimensional printing technology in orthopaedics. J Am Acad Orthop Surg. 2019; 27:918–25.
Article2. Kim HN, Liu XN, Noh KC. Use of a real-size 3D-printed model as a preoperative and intraoperative tool for minimally invasive plating of comminuted midshaft clavicle fractures. J Orthop Surg Res. 2015; 10:91.
Article3. Kim JW, Lee Y, Seo J, et al. Clinical experience with three-dimensional printing techniques in orthopedic trauma. J Orthop Sci. 2018; 23:383–8.
Article4. Chen C, Cai L, Zhang C, Wang J, Guo X, Zhou Y. Treatment of die-punch fractures with 3D printing technology. J Invest Surg. 2018; 31:385–92.
Article5. You W, Liu LJ, Chen HX, et al. Application of 3D printing technology on the treatment of complex proximal humeral fractures (Neer3-part and 4-part) in old people. Orthop Traumatol Surg Res. 2016; 102:897–903.
Article6. Zheng W, Su J, Cai L, et al. Application of 3D-printing technology in the treatment of humeral intercondylar fractures. Orthop Traumatol Surg Res. 2018; 104:83–8.
Article7. George E, Liacouras P, Rybicki FJ, Mitsouras D. Measuring and establishing the accuracy and reproducibility of 3D printed medical models. Radiographics. 2017; 37:1424–50.
Article8. Ng CY, McQueen MM. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011; 93:145–50.
Article9. Gasse N, Lepage D, Pem R, et al. Anatomical and radiological study applied to distal radius surgery. Surg Radiol Anat. 2011; 33:485–90.
Article10. Centre for Clinical Research and Biostatics (CCRB). Sample size estimation [Internet]. Hong Kong: CCRB;c2021 [cited 2021 May 1]. Available from: https://www2.ccrb.cuhk.edu.hk/stat/Means.htm.11. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41:1149–60.
Article12. Wæver D, Madsen ML, Rölfing JH, et al. Distal radius fractures are difficult to classify. Injury. 2018; 49 Suppl 1:S29–32.
Article13. Fedorov A, Beichel R, Kalpathy-Cramer J, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging. 2012; 30:1323–41.
Article14. Kamio T, Suzuki M, Asaumi R, Kawai T. DICOM segmentation and STL creation for 3D printing: a process and software package comparison for osseous anatomy. 3D Print Med. 2020; 6:17.
Article15. Rathnayaka K, Momot KI, Noser H, et al. Quantification of the accuracy of MRI generated 3D models of long bones compared to CT generated 3D models. Med Eng Phys. 2012; 34:357–63.
Article16. Huotilainen E, Jaanimets R, Valášek J, et al. Inaccuracies in additive manufactured medical skull models caused by the DICOM to STL conversion process. J Craniomaxillofac Surg. 2014; 42:e259–65.17. Bagaria V, Chaudhary K. A paradigm shift in surgical planning and simulation using 3Dgraphy: experience of first 50 surgeries done using 3D-printed biomodels. Injury. 2017; 48:2501–8.
Article18. Horas K, Hoffmann R, Faulenbach M, Heinz SM, Langheinrich A, Schweigkofler U. Advances in the preoperative planning of revision trauma surgery using 3D printing technology. J Orthop Trauma. 2020; 34:e181–6.
Article19. Yoshii Y, Ogawa T, Shigi A, Oka K, Murase T, Ishii T. Three-dimensional evaluations of preoperative planning reproducibility for the osteosynthesis of distal radius fractures. J Orthop Surg Res. 2021; 16:131.
Article20. Lilley BM, Lachance A, Peebles AM, et al. What is the deviation in 3D preoperative planning software?: a systematic review of concordance between plan and actual implant in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2022; 31:1073–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Comminuted Distal Radius Fracutures with External Skeletal Fixation
- Complications of Distal Radius Fracture
- Arthroscopically Assisted Reduction of Distal Radius Fractures
- Failure of Distal Locking Screws in an Intraarticular Distal Radius Fracture Treated with Volar Locking Plate Fixation
- The Availability of Three-Dimensional Computed Tomography Reconstructions on the Classification and Treatment Plan of Distal Radius Fractures