Clin Exp Otorhinolaryngol.
2023 Nov;16(4):308-316. 10.21053/ceo.2023.00185.
The Olfactory System: Basic Anatomy and Physiology for General Otorhinolaryngologists
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Otolaryngology-Head and Neck Surgery, University of Alabama at Birmingham, Birmingham, AL, USA
- 4Division of Otolaryngology, Department of Surgery, Veterans Affairs, Birmingham, AL, USA
- 5Department of Otolaryngology-Head and Neck Surgery, Stanford University School of Medicine, Stanford, CA, USA
- 6Sensory Organ Research Institute and Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul, Korea
- KMID: 2548359
- DOI: http://doi.org/10.21053/ceo.2023.00185
Abstract
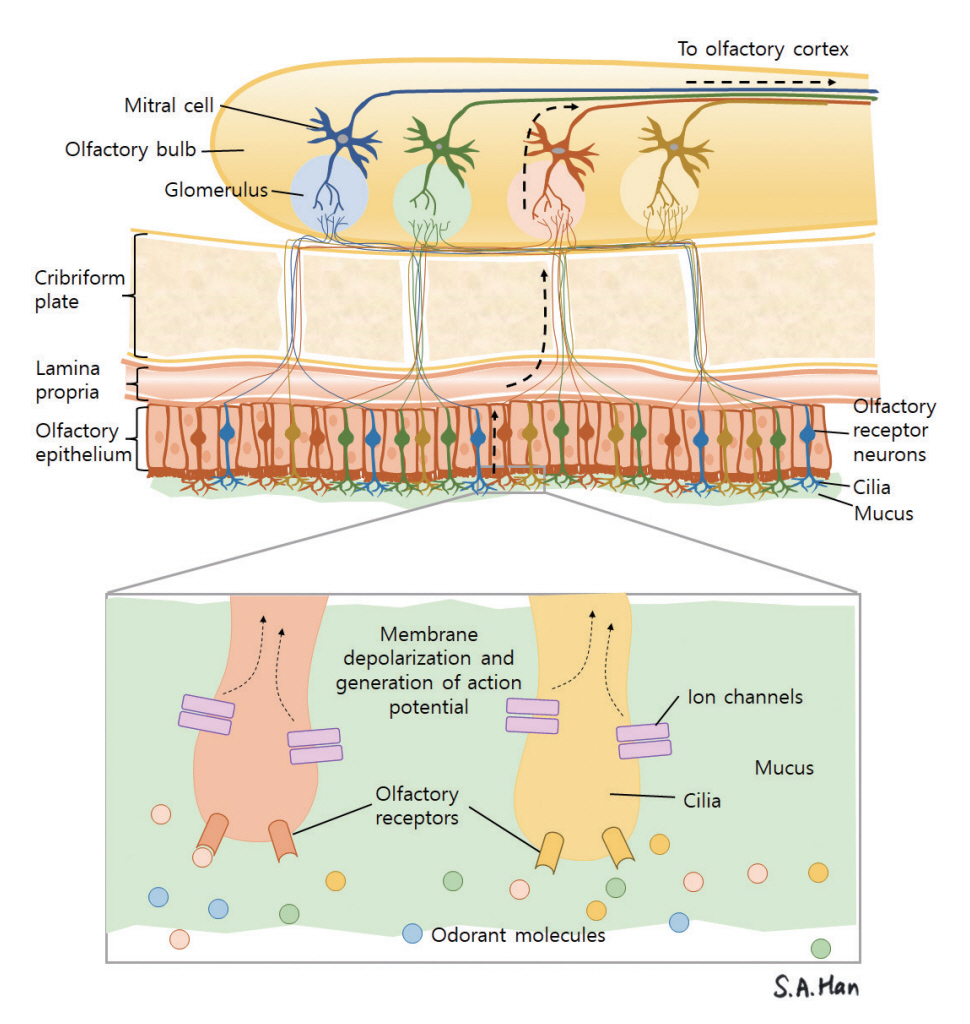
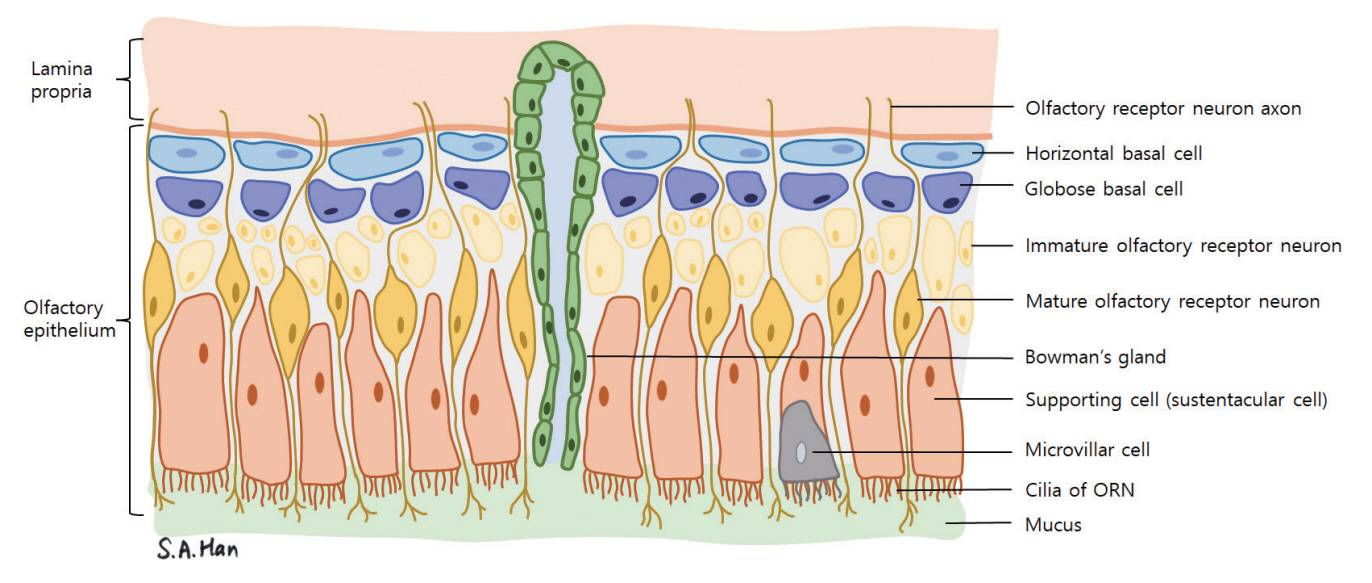
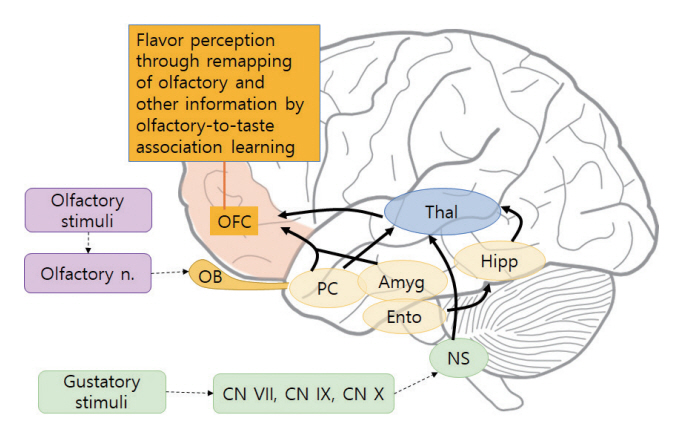
- Olfaction is one of the five basic human senses, and it is known to be one of the most primitive senses. The sense of olfaction may have been critical for human survival in prehistoric society, and although many believe its importance has diminished over time, it continues to have an impact on human interaction, bonding, and propagation of the species. Even if we are unaware of it, the sense of smell greatly affects our lives and is closely related to overall quality of life and health. Nonetheless, olfaction has been neglected from a scientific perspective compared to other senses. However, olfaction has recently received substantial attention since the loss of smell and taste has been noted as a key symptom of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Studies investigating olfaction loss in association with coronavirus disease 2019 (COVID-19) have revealed that olfactory dysfunction can be both conductive and sensorineural, possibly causing structural changes in the brain. Olfactory training is an effective treatment for olfactory dysfunction, suggesting the reorganization of neural associations. A reduced ability to smell may also alert suspicion for neurodegenerative or psychiatric disorders. Here, we summarize the basic knowledge that we, as otorhinolaryngologists, should have about the sense of smell and the peripheral and central olfactory pathways for managing and helping patients with olfactory dysfunction.
Keyword
Figure
Reference
-
1. Malnic B, Godfrey PA, Buck LB. The human olfactory receptor gene family. Proc Natl Acad Sci U S A. 2004; Feb. 101(8):2584–9.2. McGann JP. Poor human olfaction is a 19th-century myth. Science. 2017; May. 356(6338):eaam7263.3. Bushdid C, Magnasco MO, Vosshall LB, Keller A. Humans can discriminate more than 1 trillion olfactory stimuli. Science. 2014; Mar. 343(6177):1370–2.4. Rolls ET, Grabenhorst F. The orbitofrontal cortex and beyond: from affect to decision-making. Prog Neurobiol. 2008; Nov. 86(3):216–44.5. Sarnat HB, Flores-Sarnat L, Wei XC. Olfactory development, part 1: function, from fetal perception to adult wine-tasting. J Child Neurol. 2017; May. 32(6):566–78.6. Clark-Gambelunghe MB, Clark DA. Sensory development. Pediatr Clin North Am. 2015; Apr. 62(2):367–84.7. Genter MB, Doty RL. Toxic exposures and the senses of taste and smell. Handb Clin Neurol. 2019; 164:389–408.8. Pinto JM, Wroblewski KE, Kern DW, Schumm LP, McClintock MK. Olfactory dysfunction predicts 5-year mortality in older adults. PLoS One. 2014; 9(10):e107541.9. Kattar N, Do TM, Unis GD, Migneron MR, Thomas AJ, McCoul ED. Olfactory training for postviral olfactory dysfunction: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2021; Feb. 164(2):244–54.10. Buck L, Axel R. A novel multigene family may encode odorant receptors: a molecular basis for odor recognition. Cell. 1991; Apr. 65(1):175–87.11. Desai M, Oppenheimer J. The importance of considering olfactory dysfunction during the COVID-19 pandemic and in clinical practice. J Allergy Clin Immunol Pract. 2021; Jan. 9(1):7–12.12. Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020; Aug. 277(8):2251–61.13. Desiato VM, Levy DA, Byun YJ, Nguyen SA, Soler ZM, Schlosser RJ. The prevalence of olfactory dysfunction in the general population: a systematic review and meta-analysis. Am J Rhinol Allergy. 2021; Mar. 35(2):195–205.14. Bhattacharyya N, Kepnes LJ. Contemporary assessment of the prevalence of smell and taste problems in adults. Laryngoscope. 2015; May. 125(5):1102–6.15. Hoffman HJ, Rawal S, Li CM, Duffy VB. New chemosensory component in the U.S. National Health and Nutrition Examination Survey (NHANES): first-year results for measured olfactory dysfunction. Rev Endocr Metab Disord. 2016; Jun. 17(2):221–40.16. Lee WH, Wee JH, Kim DK, Rhee CS, Lee CH, Ahn S, et al. Prevalence of subjective olfactory dysfunction and its risk factors: Korean national health and nutrition examination survey. PLoS One. 2013; 8(5):e62725.17. Passali GC, Passali D, Cingi C, Ciprandi G. Smell impairment in patients with chronic rhinosinusitis: a real-life study. Eur Arch Otorhinolaryngol. 2022; Feb. 279(2):773–7.18. Kern RC. Chronic sinusitis and anosmia: pathologic changes in the olfactory mucosa. Laryngoscope. 2000; Jul. 110(7):1071–7.19. Doty RL, Hawkes CH. Chemosensory dysfunction in neurodegenerative diseases. Handb Clin Neurol. 2019; 164:325–60.20. Hura N, Xie DX, Choby GW, Schlosser RJ, Orlov CP, Seal SM, et al. Treatment of post-viral olfactory dysfunction: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2020; Sep. 10(9):1065–86.21. Burdach KJ, Doty RL. The effects of mouth movements, swallowing, and spitting on retronasal odor perception. Physiol Behav. 1987; 41(4):353–6.22. Ronnett GV, Moon C. G proteins and olfactory signal transduction. Annu Rev Physiol. 2002; 64:189–222.23. Cleland TA, Linster C. Central olfactory structures. Handb Clin Neurol. 2019; 164:79–96.24. Smith TD, Bhatnagar KP. Anatomy of the olfactory system. Handb Clin Neurol. 2019; 164:17–28.25. Morrison EE, Costanzo RM. Morphology of the human olfactory epithelium. J Comp Neurol. 1990; Jul. 297(1):1–13.26. Chess A, Simon I, Cedar H, Axel R. Allelic inactivation regulates olfactory receptor gene expression. Cell. 1994; Sep. 78(5):823–34.27. Wang F, Nemes A, Mendelsohn M, Axel R. Odorant receptors govern the formation of a precise topographic map. Cell. 1998; Apr. 93(1):47–60.28. Shepherd GM. Synaptic organization of the mammalian olfactory bulb. Physiol Rev. 1972; Oct. 52(4):864–917.29. Feldmesser E, Bercovich D, Avidan N, Halbertal S, Haim L, Gross-Isseroff R, et al. Mutations in olfactory signal transduction genes are not a major cause of human congenital general anosmia. Chem Senses. 2007; Jan. 32(1):21–30.30. Kulaga HM, Leitch CC, Eichers ER, Badano JL, Lesemann A, Hoskins BE, et al. Loss of BBS proteins causes anosmia in humans and defects in olfactory cilia structure and function in the mouse. Nat Genet. 2004; Sep. 36(9):994–8.31. Murrell W, Bushell GR, Livesey J, McGrath J, MacDonald KP, Bates PR, et al. Neurogenesis in adult human. Neuroreport. 1996; Apr. 7(6):1189–94.32. Holbrook EH, Szumowski KE, Schwob JE. An immunochemical, ultrastructural, and developmental characterization of the horizontal basal cells of rat olfactory epithelium. J Comp Neurol. 1995; Dec. 363(1):129–46.33. Mackay-Sim A. Stem cells and their niche in the adult olfactory mucosa. Arch Ital Biol. 2010; Jun. 148(2):47–58.34. London B, Nabet B, Fisher AR, White B, Sammel MD, Doty RL. Predictors of prognosis in patients with olfactory disturbance. Ann Neurol. 2008; Feb. 63(2):159–66.35. Wilson DA, Xu W, Sadrian B, Courtiol E, Cohen Y, Barnes DC. Cortical odor processing in health and disease. Prog Brain Res. 2014; 208:275–305.36. Rolls ET, Critchley HD, Mason R, Wakeman EA. Orbitofrontal cortex neurons: role in olfactory and visual association learning. J Neurophysiol. 1996; May. 75(5):1970–81.37. de Araujo IE, Rolls ET, Kringelbach ML, McGlone F, Phillips N. Tasteolfactory convergence, and the representation of the pleasantness of flavour, in the human brain. Eur J Neurosci. 2003; Oct. 18(7):2059–68.38. Doty RL. Olfactory dysfunction in Parkinson disease. Nat Rev Neurol. 2012; May. 8(6):329–39.39. Johnson ME, Bergkvist L, Mercado G, Stetzik L, Meyerdirk L, Wolfrum E, et al. Deficits in olfactory sensitivity in a mouse model of Parkinson’s disease revealed by plethysmography of odor-evoked sniffing. Sci Rep. 2020; Jun. 10(1):9242.40. Niu H, Wang Q, Zhao W, Liu J, Wang D, Muhammad B, et al. IL-1β/IL-1R1 signaling induced by intranasal lipopolysaccharide infusion regulates alpha-Synuclein pathology in the olfactory bulb, substantia nigra and striatum. Brain Pathol. 2020; Nov. 30(6):1102–18.41. Dan X, Wechter N, Gray S, Mohanty JG, Croteau DL, Bohr VA. Olfactory dysfunction in aging and neurodegenerative diseases. Ageing Res Rev. 2021; Sep. 70:101416.42. Quarmley M, Moberg PJ, Mechanic-Hamilton D, Kabadi S, Arnold SE, Wolk DA, et al. Odor identification screening improves diagnostic classification in incipient Alzheimer’s disease. J Alzheimers Dis. 2017; 55(4):1497–507.43. Kovacs T, Cairns NJ, Lantos PL. Beta-amyloid deposition and neurofibrillary tangle formation in the olfactory bulb in ageing and Alzheimer’s disease. Neuropathol Appl Neurobiol. 1999; Dec. 25(6):481–91.44. Pacyna RR, Han SD, Wroblewski KE, McClintock MK, Pinto JM. Rapid olfactory decline during aging predicts dementia and GMV loss in AD brain regions. Alzheimers Dement. 2023; Apr. 19(4):1479–90.45. Joseph A, DeLuca GC. Back on the scent: the olfactory system in CNS demyelinating diseases. J Neurol Neurosurg Psychiatry. 2016; Oct. 87(10):1146–54.46. Khurshid K, Crow AJ, Rupert PE, Minniti NL, Carswell MA, Mechanic-Hamilton DJ, et al. A quantitative meta-analysis of olfactory dysfunction in epilepsy. Neuropsychol Rev. 2019; Sep. 29(3):328–37.47. Cothren TO, Evonko CJ, MacQueen DA. Olfactory dysfunction in schizophrenia: evaluating olfactory abilities across species. Curr Top Behav Neurosci. 2023; 63:363–92.48. Sabiniewicz A, Hoffmann L, Haehner A, Hummel T. Symptoms of depression change with olfactory function. Sci Rep. 2022; Apr. 12(1):5656.49. Schofield PW, Moore TM, Gardner A. Traumatic brain injury and olfaction: a systematic review. Front Neurol. 2014; 5:5.50. Marin C, Langdon C, Alobid I, Mullol J. Olfactory dysfunction in traumatic brain injury: the role of neurogenesis. Curr Allergy Asthma Rep. 2020; Jul. 20(10):55.51. Patel ZM, Holbrook EH, Turner JH, Adappa ND, Albers MW, Altundag A, et al. International consensus statement on allergy and rhinology: olfaction. Int Forum Allergy Rhinol. 2022; Apr. 12(4):327–680.52. Yan CH, Rathor A, Krook K, Ma Y, Rotella MR, Dodd RL, et al. Effect of omega-3 supplementation in patients with smell dysfunction following endoscopic sellar and parasellar tumor resection: a multicenter prospective randomized controlled trial. Neurosurgery. 2020; Aug. 87(2):E91–8.53. Yan CH, Jang SS, Lin HC, Ma Y, Khanwalkar AR, Thai A, et al. Use of platelet-rich plasma for COVID-19-related olfactory loss: a randomized controlled trial. Int Forum Allergy Rhinol. 2023; Jun. 13(6):989–97.54. Hernandez AK, Woosch D, Haehner A, Hummel T. Omega-3 supplementation in postviral olfactory dysfunction: a pilot study. Rhinology. 2022; Apr. 60(2):139–44.55. Nguyen TP, Patel ZM. Budesonide irrigation with olfactory training improves outcomes compared with olfactory training alone in patients with olfactory loss. Int Forum Allergy Rhinol. 2018; Sep. 8(9):977–81.56. Hummel T, Rissom K, Reden J, Hahner A, Weidenbecher M, Huttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; Mar. 119(3):496–9.57. Patel ZM, Wise SK, DelGaudio JM. Randomized controlled trial demonstrating cost-effective method of olfactory training in clinical practice: essential oils at uncontrolled concentration. Laryngoscope Investig Otolaryngol. 2017; Apr. 2(2):53–6.58. Choi BY, Jeong H, Noh H, Park JY, Cho JH, Kim JK. Effects of olfactory training in patients with postinfectious olfactory dysfunction. Clin Exp Otorhinolaryngol. 2021; Feb. 14(1):88–92.59. Huang T, Wei Y, Wu D. Effects of olfactory training on posttraumatic olfactory dysfunction: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2021; Jul. 11(7):1102–12.60. Al Ain S, Poupon D, Hetu S, Mercier N, Steffener J, Frasnelli J. Smell training improves olfactory function and alters brain structure. Neuroimage. 2019; Apr. 189:45–54.61. Jiramongkolchai P, Jones MS, Peterson A, Lee JJ, Liebendorfer A, Klatt-Cromwell CN, et al. Association of olfactory training with neural connectivity in adults with postviral olfactory dysfunction. JAMA Otolaryngol Head Neck Surg. 2021; Jun. 147(6):502–9.62. Kollndorfer K, Kowalczyk K, Hoche E, Mueller CA, Pollak M, Trattnig S, et al. Recovery of olfactory function induces neuroplasticity effects in patients with smell loss. Neural Plast. 2014; 2014:140419.63. Negoias S, Pietsch K, Hummel T. Changes in olfactory bulb volume following lateralized olfactory training. Brain Imaging Behav. 2017; Aug. 11(4):998–1005.64. Adler E, Hoon MA, Mueller KL, Chandrashekar J, Ryba NJ, Zuker CS. A novel family of mammalian taste receptors. Cell. 2000; Mar. 100(6):693–702.65. Reyna RA, Kishimoto-Urata M, Urata S, Makishima T, Paessler S, Maruyama J. Recovery of anosmia in hamsters infected with SARS-CoV-2 is correlated with repair of the olfactory epithelium. Sci Rep. 2022; Jan. 12(1):628.66. Urata S, Maruyama J, Kishimoto-Urata M, Sattler RA, Cook R, Lin N, et al. Regeneration profiles of olfactory epithelium after SARSCoV-2 infection in golden Syrian hamsters. ACS Chem Neurosci. 2021; Feb. 12(4):589–95.67. Zazhytska M, Kodra A, Hoagland DA, Frere J, Fullard JF, Shayya H, et al. Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia. Cell. 2022; Mar. 185(6):1052–64.68. Chiu A, Fischbein N, Wintermark M, Zaharchuk G, Yun PT, Zeineh M. COVID-19-induced anosmia associated with olfactory bulb atrophy. Neuroradiology. 2021; Jan. 63(1):147–8.69. Liang YC, Tsai YS, Syue LS, Lee NY, Li CW. Olfactory bulb atrophy in a case of COVID-19 with hyposmia. Acad Radiol. 2020; Nov. 27(11):1649–50.70. Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022; Apr. 604(7907):697–707.71. Liu YH, Chen Y, Wang QH, Wang LR, Jiang L, Yang Y, et al. One-year trajectory of cognitive changes in older survivors of COVID-19 in Wuhan, China: a longitudinal cohort study. JAMA Neurol. 2022; May. 79(5):509–17.72. Lee MH, Perl DP, Nair G, Li W, Maric D, Murray H, et al. Microvascular injury in the brains of patients with COVID-19. N Engl J Med. 2021; Feb. 384(5):481–3.73. Khan M, Yoo SJ, Clijsters M, Backaert W, Vanstapel A, Speleman K, et al. Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb. Cell. 2021; Nov. 184(24):5932–49.74. Addison AB, Wong B, Ahmed T, Macchi A, Konstantinidis I, Huart C, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021; May. 147(5):1704–19.75. Yildirim D, Kandemirli SG, Tekcan Sanli DE, Akinci O, Altundag A. A comparative olfactory MRI, DTI and fMRI study of COVID-19 related anosmia and post viral olfactory dysfunction. Acad Radiol. 2022; Jan. 29(1):31–41.76. Stankevice D, Fjaeldstad AW, Agergaard J, Ovesen T. Long-term COVID-19 smell and taste disorders differ significantly from other postinfectious cases. Laryngoscope. 2023; Jan. 133(1):169–74.77. Damm M, Pikart LK, Reimann H, Burkert S, Goktas O, Haxel B, et al. Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study. Laryngoscope. 2014; Apr. 124(4):826–31.78. Tan BK, Han R, Zhao JJ, Tan NK, Quah ES, Tan CJ, et al. Prognosis and persistence of smell and taste dysfunction in patients with COVID-19: meta-analysis with parametric cure modelling of recovery curves. BMJ. 2022; Jul. 378:e069503.