J Yeungnam Med Sci.
2023 Nov;40(Suppl):S93-S97. 10.12701/jyms.2023.00199.
Thyroid storm caused by metastatic papillary thyroid carcinoma tissue after total thyroidectomy: a case report
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Nuclear Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2548348
- DOI: http://doi.org/10.12701/jyms.2023.00199
Abstract
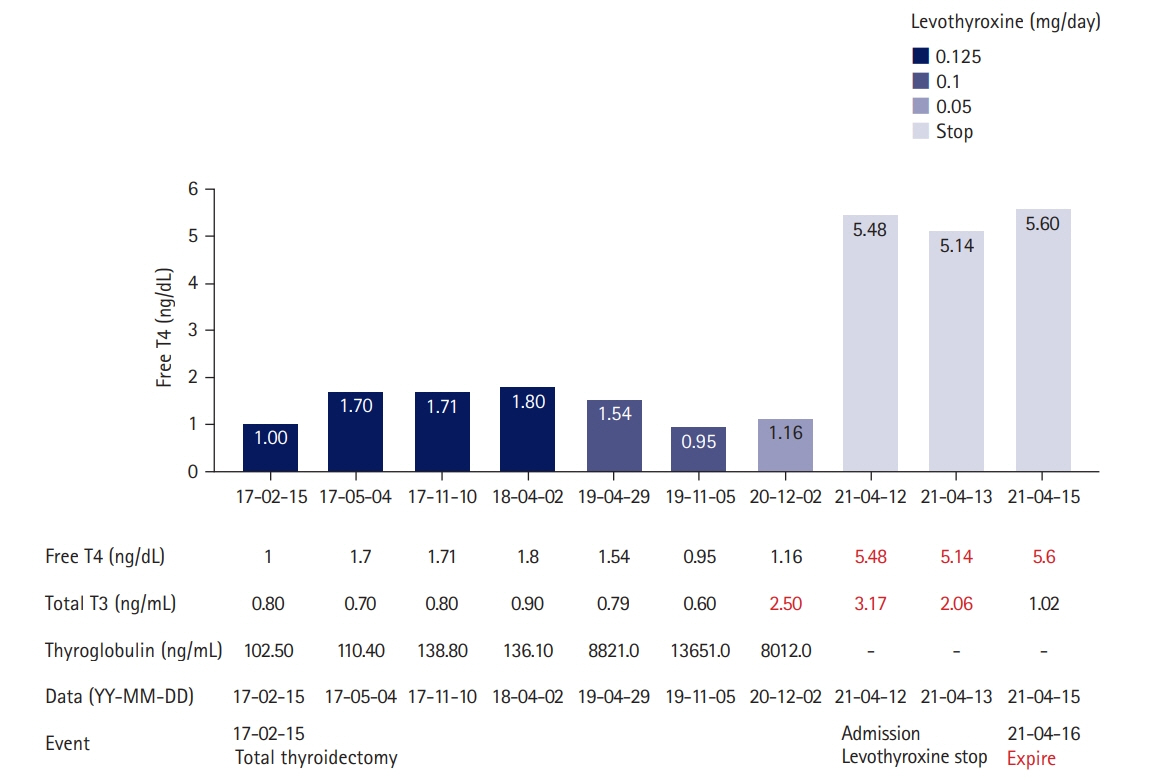
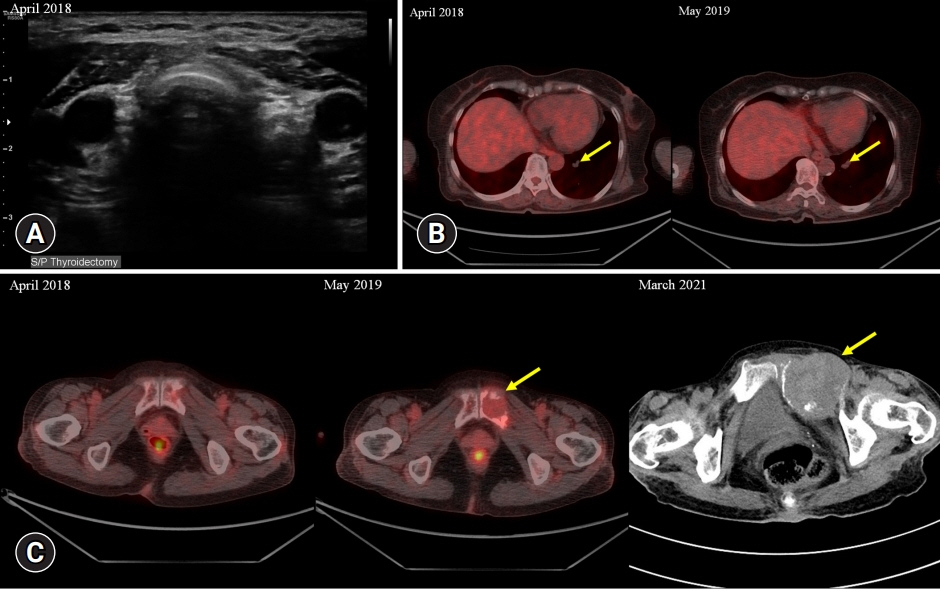
- Thyroid storm is a life-threatening form of thyrotoxicosis and an endocrinological emergency. We present a case of thyroid storm in a patient with metastatic papillary thyroid cancer. A 67-year-old woman with a history of total thyroidectomy 4 years prior to presentation was admitted with deteriorating mental status, fever, and tachycardia. Laboratory tests revealed severe thyrotoxicosis. Although the patient had no residual thyroid tissue after total thyroidectomy, she had a previously diagnosed metastatic thyroid cancer lesion in the pelvic bone. Despite initial treatment with a standard thyroid storm regimen, the patient died 6 days after hospitalization. The patient had no history of Graves disease; however, a thyroxine receptor antibody was detected postmortem. The patient had a history of exposure to an iodine contrast agent, which is a rare cause of thyrotoxicosis. Thyroxine production from a differentiated thyroid carcinoma is rare but can be a source of clinically significant thyrotoxicosis in patients post-thyroidectomy. Overlapping Graves disease is a common stimulus; however, other causes, such as exogenous iodine, cannot be excluded. This case demonstrates that in the setting of metastatic thyroid carcinoma, thyrotoxicosis cannot be completely ruled out as a cause of suspicious symptoms, even in patients with a history of total thyroidectomy.
Figure
Reference
-
References
1. Ishihara T, Ikekubo K, Shimodahira M, Iwakura T, Kobayashi M, Hino M, et al. A case of TSH receptor antibody-positive hyperthyroidism with functioning metastases of thyroid carcinoma. Endocr J. 2002; 49:241–5.
Article2. Folkestad L, Brandt F, Brix T, Vogsen M, Bastholt L, Grupe P, et al. Total thyroidectomy for thyroid cancer followed by thyroid storm due to thyrotropin receptor antibody stimulation of metastatic thyroid tissue. Eur Thyroid J. 2017; 6:276–80.
Article3. Chiha M, Samarasinghe S, Kabaker AS. Thyroid storm: an updated review. J Intensive Care Med. 2015; 30:131–40.4. Burch HB, Wartofsky L. Life-threatening thyrotoxicosis: thyroid storm. Endocrinol Metab Clin North Am. 1993; 22:263–77.
Article5. Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid. 2012; 22:661–79.
Article6. Basida B, Zalavadiya N, Ismail R, Krayem H. Weathering the storm: thyroid storm precipitated by radioiodine contrast in metastatic thyroid carcinoma. Cureus. 2021; 13:e14219.
Article7. Naito Y, Sone T, Kataoka K, Sawada M, Yamazaki K. Thyroid storm due to functioning metastatic thyroid carcinoma in a burn patient. Anesthesiology. 1997; 87:433–5.
Article8. Suwansaksri N, Preechasuk L, Kunavisarut T. Nonthionamide drugs for the treatment of hyperthyroidism: from present to future. Int J Endocrinol. 2018; 2018:5794054.
Article9. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1343–421.
Article10. Solomon BL, Wartofsky L, Burman KD. Adjunctive cholestyramine therapy for thyrotoxicosis. Clin Endocrinol (Oxf). 1993; 38:39–43.
Article11. Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, et al. 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (first edition). Endocr J. 2016; 63:1025–64.
Article12. Liu J, Wang Y, Da D, Zheng M. Hyperfunctioning thyroid carcinoma: a systematic review. Mol Clin Oncol. 2019; 11:535–50.
Article13. Tan J, Zhang G, Xu W, Meng Z, Dong F, Zhang F, et al. Thyrotoxicosis due to functioning metastatic follicular thyroid carcinoma after twelve I-131 therapies. Clin Nucl Med. 2009; 34:615–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subcutaneous Soft Tissue Implantation of Papillary Thyroid Carcinoma after Endoscopic Thyroidectomy
- A Case of a Patient with Medical-Refractory Thyroid Storm Treated Successfully by Surgical Resection
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- A Case of Ectopic Thyroid Papillary Carcinoma with Incidental Papillary Thyroid Microcarcinoma
- Occult Papillary Thyroid Carcinoma Presenting as a Metastatic Pleural Effusion