J Yeungnam Med Sci.
2023 Nov;40(Suppl):S65-S72. 10.12701/jyms.2023.00661.
Comparison of serum anti-Müllerian hormone between unilateral and bilateral ovarian endometriomas during follicular, luteal, and random menstrual phases: a retrospective study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- 2Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2548344
- DOI: http://doi.org/10.12701/jyms.2023.00661
Abstract
- Background
Over the last two decades, serum levels of anti-Müllerian hormone (AMH) have been shown to be reliable markers of ovarian reserve. This study aimed to compare baseline serum AMH levels and well-controlled clinical factors between patients with unilateral and bilateral ovarian endometriomas during the menstrual phase.
Methods
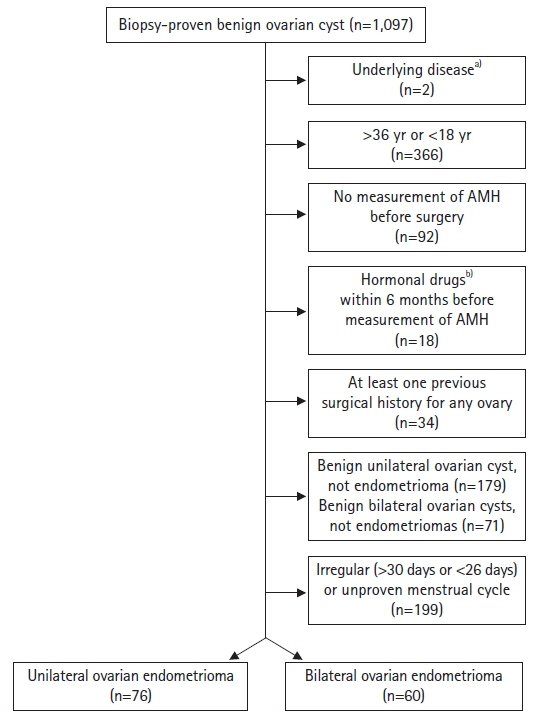
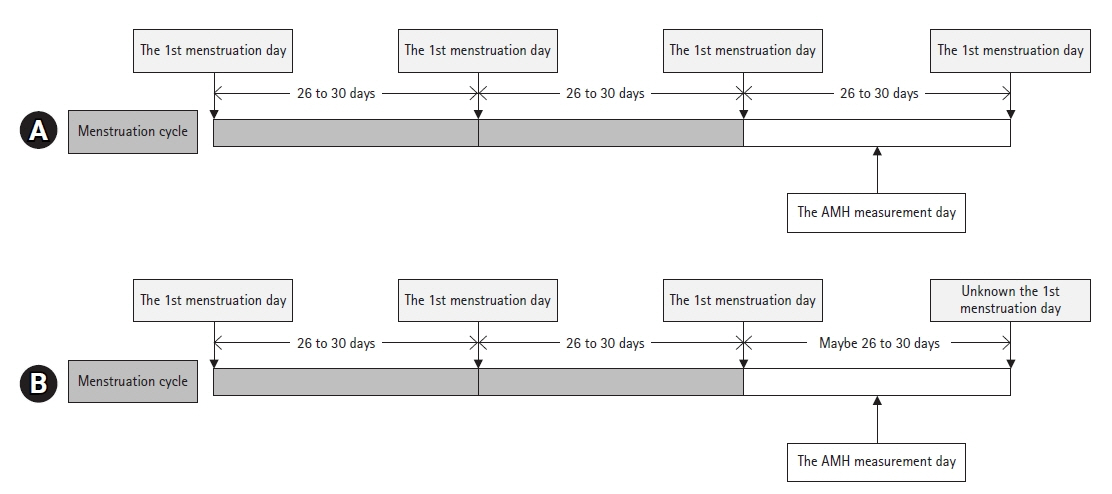
We conducted a retrospective study. We enrolled 136 patients aged 18 to 36 years who were diagnosed with unilateral or bilateral ovarian endometriomas. Serum AMH levels of all patients and their latest two to three menstrual cycles were measured before surgery for ovarian endometriomas. The latest menstrual cycle length ranged from 26 to 30 days. Patients with irregular menstruation, a recent medication history of hormonal drugs other than oral contraceptive pills, a previous history of ovarian surgery, or any medical history influencing ovarian function were excluded.
Results
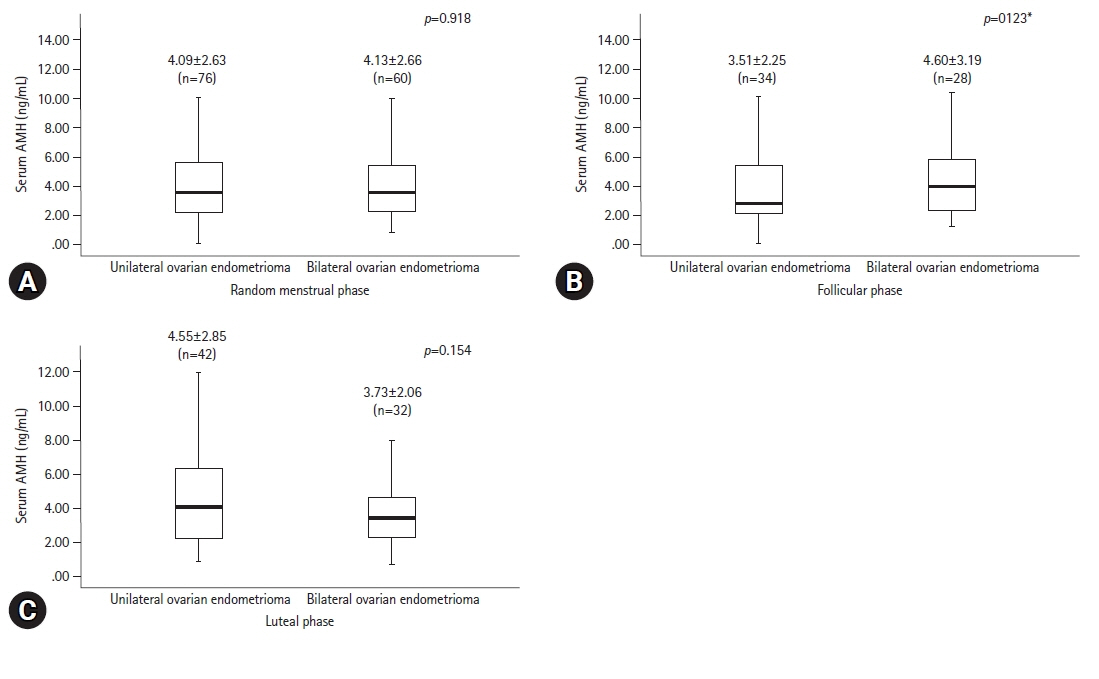
Of the 136 patients, 76 (55.9%) had unilateral ovarian endometriomas and 60 (44.1%) had bilateral ovarian endometriomas. Serum AMH levels were not significantly different between the two groups in the follicular phase, luteal phase, or at any random time point.
Conclusion
Serum AMH levels were not significantly different between unilateral and bilateral ovarian endometriomas in the follicular and luteal phases, or at any random time during the menstrual cycle when various confounding factors were excluded.
Figure
Reference
-
References
1. Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006; 12:685–718.
Article2. Iwase A, Osuka S, Nakamura T, Kato N, Takikawa S, Goto M, et al. Usefulness of the ultrasensitive anti-Müllerian hormone assay for predicting true ovarian reserve. Reprod Sci. 2016; 23:756–60.
Article3. La Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Artenisio AC, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. 2010; 16:113–30.
Article4. Wunder DM, Bersinger NA, Yared M, Kretschmer R, Birkhäuser MH. Statistically significant changes of antimüllerian hormone and inhibin levels during the physiologic menstrual cycle in reproductive age women. Fertil Steril. 2008; 89:927–33.
Article5. Lambert-Messerlian G, Plante B, Eklund EE, Raker C, Moore RG. Levels of antimüllerian hormone in serum during the normal menstrual cycle. Fertil Steril. 2016; 105:208–13.
Article6. Pankhurst MW, Chong YH. Variation in circulating antimüllerian hormone precursor during the periovulatory and acute postovulatory phases of the human ovarian cycle. Fertil Steril. 2016; 106:1238–43.
Article7. Muzii L, Di Tucci C, Di Feliciantonio M, Galati G, Di Donato V, Musella A, et al. Antimüllerian hormone is reduced in the presence of ovarian endometriomas: a systematic review and meta-analysis. Fertil Steril. 2018; 110:932–40.
Article8. Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012; 98:511–9.
Article9. Hwu YM, Wu FS, Li SH, Sun FJ, Lin MH, Lee RK. The impact of endometrioma and laparoscopic cystectomy on serum anti-Müllerian hormone levels. Reprod Biol Endocrinol. 2011; 9:80.
Article10. Yoon H, Lee H, Kim S, Joo J. The relationship of ovarian endometrioma and its size to the preoperative serum anti-Mullerian hormone level. Ginekol Pol. 2020; 91:313–9.
Article11. Karadağ C, Yoldemir T, Demircan Karadağ S, Turgut A. The effects of endometrioma size and bilaterality on ovarian reserve. J Obstet Gynaecol. 2020; 40:531–6.
Article12. McIntosh JE, Matthews CD, Crocker JM, Broom TJ, Cox LW. Predicting the luteinizing hormone surge: relationship between the duration of the follicular and luteal phases and the length of the human menstrual cycle. Fertil Steril. 1980; 34:125–30.13. Revised American Fertility Society classification of endometriosis: 1985. Fertil Steril. 1985; 43:351–2.14. Şenateş E, Çolak Y, Erdem ED, Yeşil A, Coşkunpınar E, Şahin Ö, et al. Serum anti-Müllerian hormone levels are lower in reproductive-age women with Crohn's disease compared to healthy control women. J Crohns Colitis. 2013; 7:e29–34.
Article15. Baek JC, Jo JY, Lee SM, Cho IA, Shin JK, Lee SA, et al. Differences in 25-hydroxy vitamin D and vitamin D-binding protein concentrations according to the severity of endometriosis. Clin Exp Reprod Med. 2019; 46:125–31.
Article16. Wu MH, Hsiao KY, Tsai SJ. Endometriosis and possible inflammation markers. Gynecol Minim Invasive Ther. 2015; 4:61–7.
Article17. Kitajima M, Matsumoto K, Murakami N, Harada A, Kitajima Y, Masuzaki H, et al. Ovarian reserve after three-step laparoscopic surgery for endometriomas utilizing dienogest: a pilot study. Reprod Med Biol. 2020; 19:425–31.18. Steiner AZ, Stanczyk FZ, Patel S, Edelman A. Antimullerian hormone and obesity: insights in oral contraceptive users. Contraception. 2010; 81:245–8.
Article19. La Marca A, Sighinolfi G, Giulini S, Traglia M, Argento C, Sala C, et al. Normal serum concentrations of anti-Müllerian hormone in women with regular menstrual cycles. Reprod Biomed Online. 2010; 21:463–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum Anti-Mullerian Hormone Levels before Surgery in Patients with Ovarian Endometriomas Compared to Other Benign Ovarian Cysts
- Serum levels and expression of Mullerian inhibiting substance in the human ovary during menstrual cycle
- Initial Preoperative Hemoglobin Level Affects the Rate of Decline in Anti-Müllerian Hormone Levels after Laparoscopic Ovarian Cystectomy in Women with Ovarian Endometriosis
- Surgical impact on serum anti-Mullerian hormone in women with benign ovarian cyst: A prospective study
- Serum luteinizing hormone level and luteinizing hormone/follicle-stimulating hormone ratio but not serum anti-Mullerian hormone level is related to ovarian volume in Korean women with polycystic ovary syndrome