Korean Circ J.
2023 Nov;53(11):727-743. 10.4070/kcj.2023.0242.
Remote Cardiac Rehabilitation With Wearable Devices
- Affiliations
-
- 1Department of Cardiology, Sakakibara Heart Institute, Tokyo, Japan
- 2Department of Cardiovascular Medicine, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
- 3Department of Nursing, Sakakibara Heart Institute, Tokyo, Japan
- 4Department of Nutrition, Sakakibara Heart Institute, Tokyo, Japan
- 5Department of Psychology, Sakakibara Heart Institute, Tokyo, Japan
- 6Department of Psychology and Social Welfare, Seigakuin University, Saitama, Japan
- 7Department of Rehabilitation, Sakakibara Heart Institute, Tokyo, Japan
- 8Department of Cardiology, National Hospital Organization Takasaki General Medical Center, Gunma, Japan
- 9Department of Cardiology, Keio University of Medicine, Tokyo, Japan
- 10Department of Cardiovascular Surgery, Seirei Yokohama Hospital, Kanagawa, Japan
- 11Department of Computational Diagnostic Radiology and Preventive Medicine, The University of Tokyo, Tokyo, Japan
- 12Nagasaki Clinic, Tokyo, Japan
- 13Clinical Research Promotion Center, The University of Tokyo Hospital, Tokyo, Japan
- 14Sakakibara Heart Institute, Tokyo, Japan
- KMID: 2548235
- DOI: http://doi.org/10.4070/kcj.2023.0242
Abstract
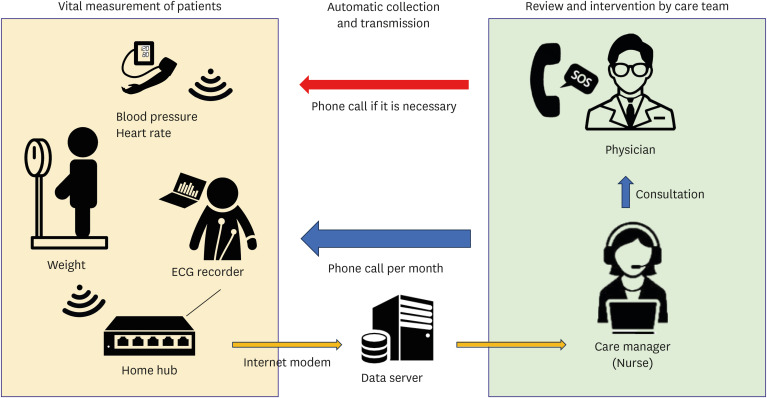
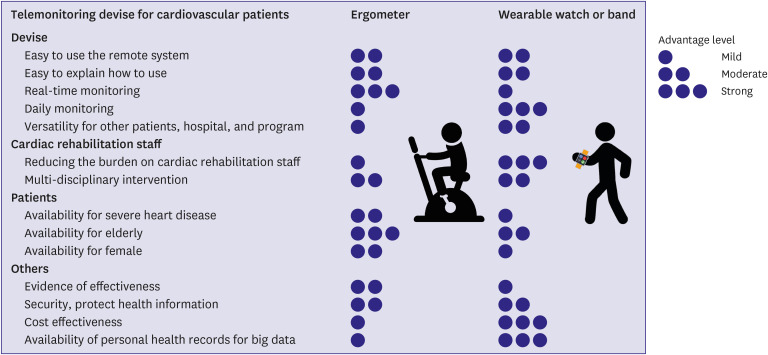
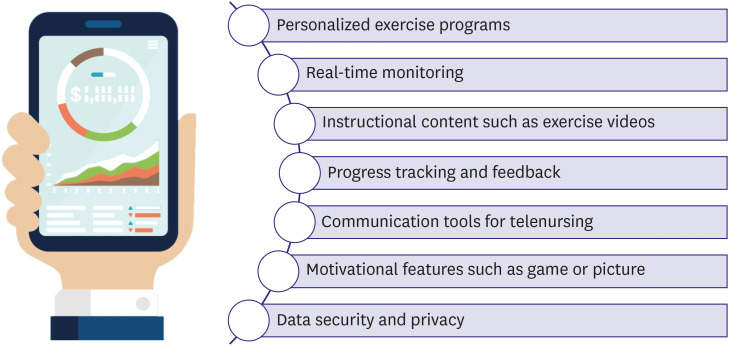
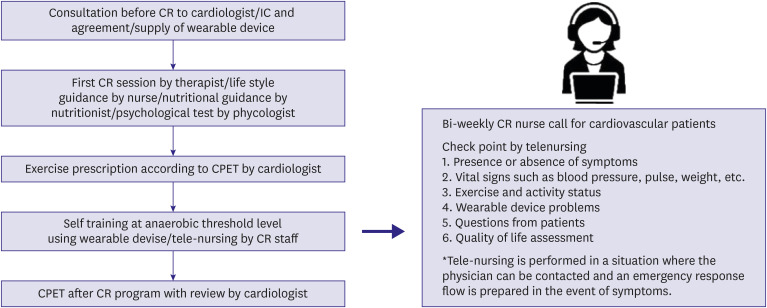
- Although cardiac rehabilitation (CR) has been shown to improve exercise tolerance and prognosis in patients with cardiovascular diseases, there remains low participation in outpatient CR. This may be attributed to the patients’ busy schedules and difficulty in visiting the hospital due to distance, cost, avoidance of exercise, and severity of coronary disease. To overcome these challenges, many countries are exploring the possibility of remote CR. Specifically, there is increasing attention on the development of remote CR devices, which allow transmission of vital information to the hospital via a remote CR application linked to a wearable device for telemonitoring by dedicated hospital staff. In addition, remote CR programs can support return to work after hospitalization. Previous studies have demonstrated the effects of remote CR on exercise tolerance. However, the preventive effects of remote CR on cardiac events and mortality remain controversial. Thus, safe and effective remote CR requires exercise risk stratification for each patient, telenursing by skilled staff, and multidisciplinary interventions. Therefore, quality assurance of telenursing and multi-disciplinary interventions will be essential for remote CR. Remote CR may become an important part of cardiac management in the future. However, issues such as costeffectiveness and insurance coverage still persist.
Figure
Reference
-
1. Goto Y. Current state of CR in Japan. Prog Cardiovasc Dis. 2014; 56:557–562. PMID: 24607022.2. Nakayama A, Nagayama M, Morita H, Kawahara T, Komuro I, Isobe M. The use of geographical analysis in assessing the impact of patients’ home addresses on their participation in outpatient CR: a prospective cohort study. Environ Health Prev Med. 2020; 25:76. PMID: 33248454.3. De Vos C, Li X, Van Vlaenderen I, et al. Participating or not in a CR programme: factors influencing a patient’s decision. Eur J Prev Cardiol. 2013; 20:341–348. PMID: 22345682.
Article4. Ghisi GL, Kin SM, Price J, et al. Women-focused cardiovascular rehabilitation: an International Council of Cardiovascular Prevention and Rehabilitation clinical practice guideline. Can J Cardiol. 2022; 38:1786–1798. PMID: 36085185.
Article5. Ministry of Health, Labour and Welfare (JP). Overview of the 2021 medical facilities (dynamic) survey and hospital report [Internet]. Tokyo: Ministry of Health, Labour and Welfare;2022. cited 2023 October 12. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/21/index.html.6. Japanese Circulation Society. Report by the Japanese Registry Of All cardiac and vascular Diseases (JROAD) in 2021 [Internet]. Tokyo: Japanese Circulation Society;2021. cited 2023 October 12. Available from: https://www.j-circ.or.jp/jittai_chosa/media/jittai_chosa2020web_1.pdf.7. Kida K, Nishitani-Yokoyama M, Oishi S, et al. Japanese Association of CR (JACR) public relations committee. nationwide survey of Japanese CR training facilities during the coronavirus disease 2019 outbreak. Circ Rep. 2021; 3:311–315. PMID: 34136705.
Article8. O’Doherty AF, Humphreys H, Dawkes S, et al. How has technology been used to deliver CR during the COVID-19 pandemic? An international cross-sectional survey of healthcare professionals conducted by the BACPR. BMJ Open. 2021; 11:e046051.9. Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based CR: a systematic review and meta-analysis. Heart. 2016; 102:1183–1192. PMID: 26936337.
Article10. Cleland JG, Louis AA, Rigby AS, Janssens U, Balk AH. TEN-HMS Investigators. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study. J Am Coll Cardiol. 2005; 45:1654–1664. PMID: 15893183.11. Ong MK, Romano PS, Edgington S, et al. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the Better Effectiveness After Transition -- Heart Failure (BEAT-HF) randomized clinical trial. JAMA Intern Med. 2016; 176:310–318. PMID: 26857383.
Article12. Koehler F, Koehler K, Deckwart O, et al. Efficacy of Telemedical Interventional Management in Patients with Heart Failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018; 392:1047–1057. PMID: 30153985.
Article13. Liu H, Wilton SB, Southern DA, et al. Automated referral to CR after coronary artery bypass grafting is associated with modest improvement in program completion. Can J Cardiol. 2019; 35:1491–1498. PMID: 31604671.
Article14. Cavalheiro AH, Silva Cardoso J, Rocha A, Moreira E, Azevedo LF. Effectiveness of tele-rehabilitation programs in heart failure: a systematic review and meta-analysis. Health Serv Insights. 2021; 14:11786329211021668. PMID: 34188484.
Article15. Nakayama A, Takayama N, Kobayashi M, et al. Remote CR is a good alternative of outpatient CR in the COVID-19 era. Environ Health Prev Med. 2020; 25:48. PMID: 32891113.16. Keteyian SJ, Ades PA, Beatty AL, et al. A review of the design and implementation of a hybrid CR program: an expanding opportunity for optimizing cardiovascular care. J Cardiopulm Rehabil Prev. 2022; 42:1–9. PMID: 34433760.17. Kikuchi A, Taniguchi T, Nakamoto K, et al. Feasibility of home-based CR using an integrated telerehabilitation platform in elderly patients with heart failure: a pilot study. J Cardiol. 2021; 78:66–71. PMID: 33579602.
Article18. Nagatomi Y, Ide T, Higuchi T, et al. Home-based CR using information and communication technology for heart failure patients with frailty. ESC Heart Fail. 2022; 9:2407–2418. PMID: 35534907.
Article19. Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens (Greenwich). 2019; 21:853–858. PMID: 30803128.
Article20. Mukkamala R, Yavarimanesh M, Natarajan K, et al. Evaluation of the accuracy of cuffless blood pressure measurement devices: challenges and proposals. Hypertension. 2021; 78:1161–1167. PMID: 34510915.
Article21. Lee YH, Hur SH, Sohn J, et al. Impact of home-based exercise training with wireless monitoring on patients with acute coronary syndrome undergoing percutaneous coronary intervention. J Korean Med Sci. 2013; 28:564–568. PMID: 23580444.
Article22. Chung H, Ko H, Thap T, et al. Smartphone-based CR program: feasibility study. PLoS One. 2016; 11:e0161268. PMID: 27551969.23. Lee H, Chung H, Ko H, et al. Dedicated CR wearable sensor and its clinical potential. PLoS One. 2017; 12:e0187108. PMID: 29088260.24. Sakakibara Heart Institute. Remote CR System, TeleRehab [Internet]. Tokyo: Sakakibara Heart Institute;2022. cited 2023 August 20. Available from: https://heart-rehab.jp/informations/43/.25. Watson A, Chapman R, Shafai G, Maricich YA. FDA regulations and prescription digital therapeutics: evolving with the technologies they regulate. Front Digit Health. 2023; 5:1086219. PMID: 37139487.
Article26. Tzeis S, Asvestas D, Moraitis N, et al. Safety of smartwatches and their chargers in patients with cardiac implantable electronic devices. Europace. 2021; 23:99–103. PMID: 33038213.
Article27. American Heart Association. New telehealth certification available to health care professionals [Internet]. Chicago (IL): American Heart Association;2023. cited 2023 August 20. Available from: https://newsroom.heart.org/news/new-telehealth-certification-available-to-health-care-professionals.28. Centers for Medicare & Medicaid Services. COVID-19 emergency declaration blanket waivers for health care providers [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services;2021. cited 2023 August 20. Available from: https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf.29. Jiang X, Xie H, Tang R, et al. Characteristics of online health care services from China’s largest online medical platform: cross-sectional survey study. J Med Internet Res. 2021; 23:e25817. PMID: 33729985.30. Jones RB, Tredinnick-Rowe J, Baines R, Maramba ID, Chatterjee A. Use and usability of GP online services: a mixed-methods sequential study, before and during the COVID-19 pandemic, based on qualitative interviews, analysis of routine eConsult usage and feedback data, and assessment of GP websites in Devon and Cornwall, England. BMJ Open. 2022; 12:e058247.
Article31. Sadeghi M, Rahiminam H, Amerizadeh A, et al. Prevalence of return to work in cardiovascular patients after CR: a systematic review and meta-analysis. Curr Probl Cardiol. 2022; 47:100876. PMID: 34034921.32. Nakayama A. CR team-led employment support including remote employment support. SHINZO. 2023; 55:554–558.33. Ades PA, Huang D, Weaver SO. CR participation predicts lower rehospitalization costs. Am Heart J. 1992; 123:916–921. PMID: 1550000.34. Ades PA, Pashkow FJ, Nestor JR. Cost-effectiveness of CR after myocardial infarction. J Cardiopulm Rehabil. 1997; 17:222–231. PMID: 9271765.35. Frederix I, Hansen D, Coninx K, et al. Effect of comprehensive cardiac telerehabilitation on one-year cardiovascular rehospitalization rate, medical costs and quality of life: a cost-effectiveness analysis. Eur J Prev Cardiol. 2016; 23:674–682. PMID: 26289723.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perspective on Wearable Devices for Cardiac Arrhythmia Detection
- Introduction of Wearable Device in Cardiovascular Field for Monitoring Arrhythmia
- Can Fitness Trackers Track Sleep?
- Validation of Wearable Digital Devices for Heart Rate Measurement During Exercise Test in Patients With Coronary Artery Disease
- An Update on the Use of Wearable Devices in Men’s Health