J Korean Med Sci.
2023 Nov;38(45):e322. 10.3346/jkms.2023.38.e322.
Hyperkalemia Detection in Emergency Departments Using Initial ECGs: A Smartphone AI ECG Analyzer vs. Board-Certified Physicians
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Division of Cardiology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Emergency Medicine, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
- 4Division of Data Science, Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea
- 5ARPI Inc., Seongnam, Korea
- KMID: 2547979
- DOI: http://doi.org/10.3346/jkms.2023.38.e322
Abstract
- Background
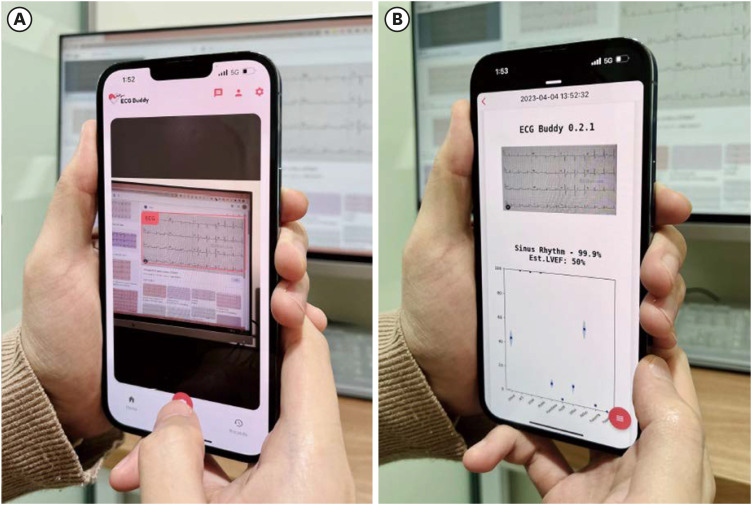
Hyperkalemia is a potentially fatal condition that mandates rapid identification in emergency departments (EDs). Although a 12-lead electrocardiogram (ECG) can indicate hyperkalemia, subtle changes in the ECG often pose detection challenges. An artificial intelligence application that accurately assesses hyperkalemia risk from ECGs could revolutionize patient screening and treatment. We aimed to evaluate the efficacy and reliability of a smartphone application, which utilizes camera-captured ECG images, in quantifying hyperkalemia risk compared to human experts.
Methods
We performed a retrospective analysis of ED hyperkalemic patients (serum potassium ≥ 6 mmol/L) and their age- and sex-matched non-hyperkalemic controls. The application was tested by five users and its performance was compared to five board-certified emergency physicians (EPs).
Results
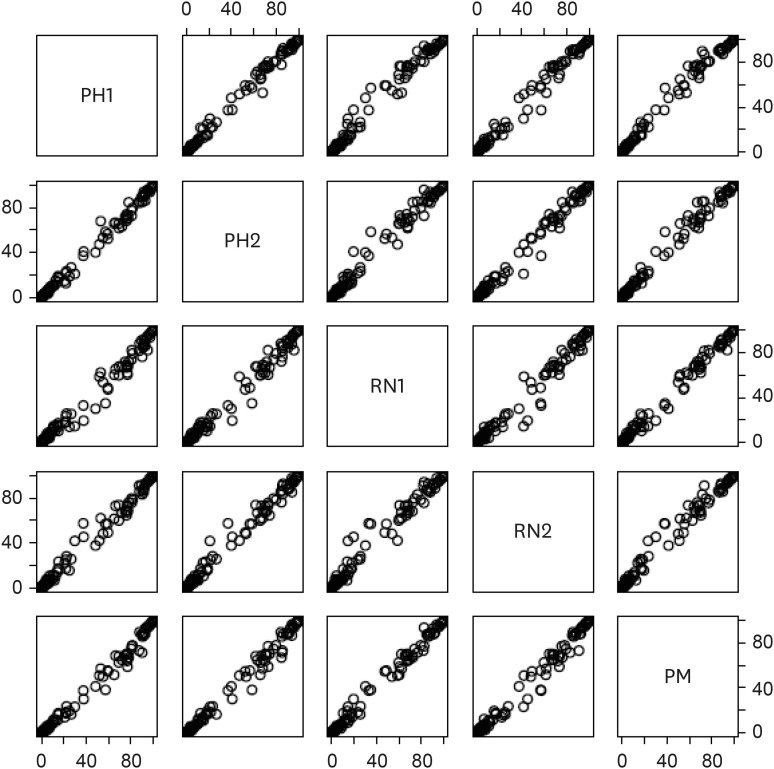
Our study included 125 patients. The area under the curve (AUC)-receiver operating characteristic of the application’s output was nearly identical among the users, ranging from 0.898 to 0.904 (median: 0.902), indicating almost perfect interrater agreement (Fleiss’ kappa 0.948). The application demonstrated high sensitivity (0.797), specificity (0.934), negative predictive value (NPV) (0.815), and positive predictive value (PPV) (0.927). In contrast, the EPs showed moderate interrater agreement (Fleiss’ kappa 0.551), and their consensus score had a significantly lower AUC of 0.662. The physicians’ consensus demonstrated a sensitivity of 0.203, specificity of 0.934, NPV of 0.527, and PPV of 0.765. Notably, this performance difference remained significant regardless of patients’ sex and age (P < 0.001 for both).
Conclusion
Our findings suggest that a smartphone application can accurately and reliably quantify hyperkalemia risk using initial ECGs in the ED.
Keyword
Figure
Reference
-
1. Diercks DB, Shumaik GM, Harrigan RA, Brady WJ, Chan TC. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med. 2004; 27(2):153–160. PMID: 15261358.
Article2. Dillon JJ, DeSimone CV, Sapir Y, Somers VK, Dugan JL, Bruce CJ, et al. Noninvasive potassium determination using a mathematically processed ECG: proof of concept for a novel “blood-less, blood test”. J Electrocardiol. 2015; 48(1):12–18. PMID: 25453193.
Article3. Attia ZI, DeSimone CV, Dillon JJ, Sapir Y, Somers VK, Dugan JL, et al. Novel bloodless potassium determination using a signal-processed single-lead ECG. J Am Heart Assoc. 2016; 5(1):e002746. PMID: 26811164.
Article4. Velagapudi V, O’Horo JC, Vellanki A, Baker SP, Pidikiti R, Stoff JS, et al. Computer-assisted image processing 12 lead ECG model to diagnose hyperkalemia. J Electrocardiol. 2017; 50(1):131–138. PMID: 27662777.
Article5. Laks MM, Elek SR. The effect of potassium on the electrocardiogram: clinical and transmembrane correlations. Dis Chest. 1967; 51(6):573–586. PMID: 6027025.6. Wrenn KD, Slovis CM, Slovis BS. The ability of physicians to predict hyperkalemia from the ECG. Ann Emerg Med. 1991; 20(11):1229–1232. PMID: 1952310.
Article7. Montague BT, Ouellette JR, Buller GK. Retrospective review of the frequency of ECG changes in hyperkalemia. Clin J Am Soc Nephrol. 2008; 3(2):324–330. PMID: 18235147.
Article8. Lin CS, Lin C, Fang WH, Hsu CJ, Chen SJ, Huang KH, et al. A deep-learning algorithm (ECG12Net) for detecting hypokalemia and hyperkalemia by electrocardiography: algorithm development. JMIR Med Inform. 2020; 8(3):e15931. PMID: 32134388.
Article9. Galloway CD, Valys AV, Shreibati JB, Treiman DL, Petterson FL, Gundotra VP, et al. Development and validation of a deep-learning model to screen for hyperkalemia from the electrocardiogram. JAMA Cardiol. 2019; 4(5):428–436. PMID: 30942845.
Article10. Chiu IM, Cheng JY, Chen TY, Wang YM, Cheng CY, Kung CT, et al. Using deep transfer learning to detect hyperkalemia from ambulatory electrocardiogram monitors in intensive care units: personalized medicine approach. J Med Internet Res. 2022; 24(12):e41163. PMID: 36469396.
Article11. Corsi C, Cortesi M, Callisesi G, De Bie J, Napolitano C, Santoro A, et al. Noninvasive quantification of blood potassium concentration from ECG in hemodialysis patients. Sci Rep. 2017; 7(1):42492. PMID: 28198403.
Article12. Choi YJ, Park MJ, Ko Y, Soh MS, Kim HM, Kim CH, et al. Artificial intelligence versus physicians on interpretation of printed ECG images: diagnostic performance of ST-elevation myocardial infarction on electrocardiography. Int J Cardiol. 2022; 363:6–10. PMID: 35691440.
Article13. Kim D, Hwang JE, Cho Y, Cho HW, Lee W, Lee JH, et al. A retrospective clinical evaluation of an artificial intelligence screening method for early detection of STEMI in the emergency department. J Korean Med Sci. 2022; 37(10):e81. PMID: 35289140.
Article14. Conger AJ. Integration and generalization of kappas for multiple raters. Psychol Bull. 1980; 88(2):322–328.
Article15. Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971; 76(5):378–382.
Article16. Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. 3rd ed. New York, NY, USA: John Wiley & Sons;2003.17. Chan KS, Chan YM, Tan AH, Liang S, Cho YT, Hong Q, et al. Clinical validation of an artificial intelligence-enabled wound imaging mobile application in diabetic foot ulcers. Int Wound J. 2022; 19(1):114–124. PMID: 33942998.
Article18. Kwon JM, Jung MS, Kim KH, Jo YY, Shin JH, Cho YH, et al. Artificial intelligence for detecting electrolyte imbalance using electrocardiography. Ann Noninvasive Electrocardiol. 2021; 26(3):e12839. PMID: 33719135.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preliminary comparison of length of stay of patients treated by 3 board-certified physicians and 1 pediatric resident in the emergency department during night shifts
- Smartphone AI vs. Medical Experts: A Comparative Study in Prehospital STEMI Diagnosis
- Diagnostic Value of an Electrocardiogram for Hyperkalemia
- ROMIAE (Rule-Out Acute Myocardial Infarction Using Artificial Intelligence Electrocardiogram Analysis) trial study protocol: a prospective multicenter observational study for validation of a deep learning–based 12-lead electrocardiogram analysis model for detecting acute myocardial infarction in patients visiting the emergency department
- Getting to the heart of the issue: senior emergency resident electrocardiogram interpretation and its impact on quality assurance events