J Korean Med Sci.
2023 Nov;38(43):e356. 10.3346/jkms.2023.38.e356.
Brain Tumor Classification by Methylation Profile
- Affiliations
-
- 1Department of Pathology, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea
- 3Institute of Neuroscience, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2547966
- DOI: http://doi.org/10.3346/jkms.2023.38.e356
Abstract
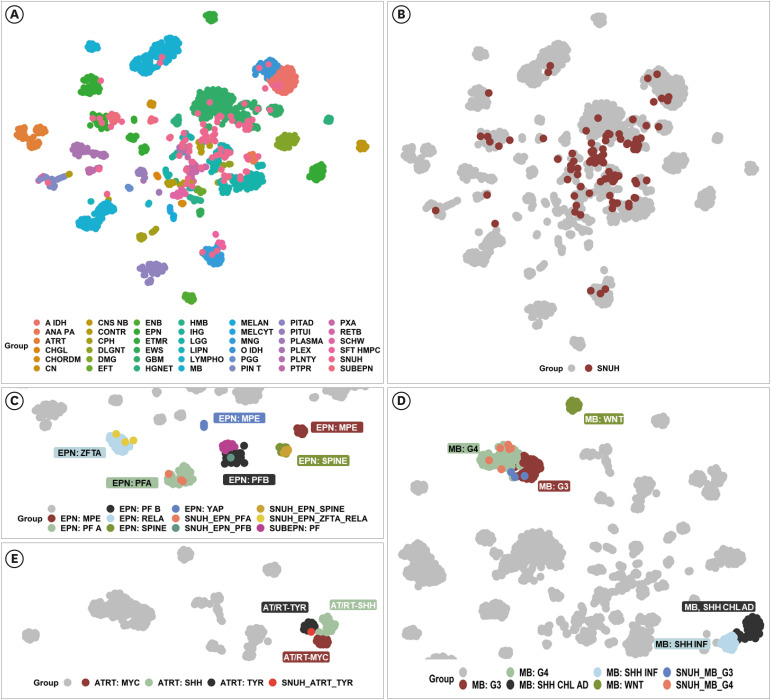
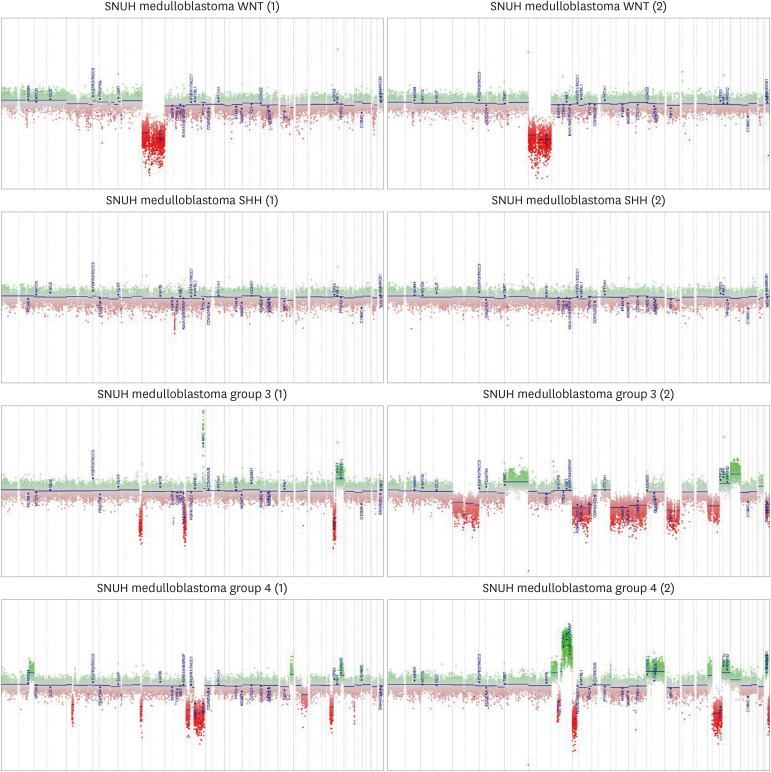
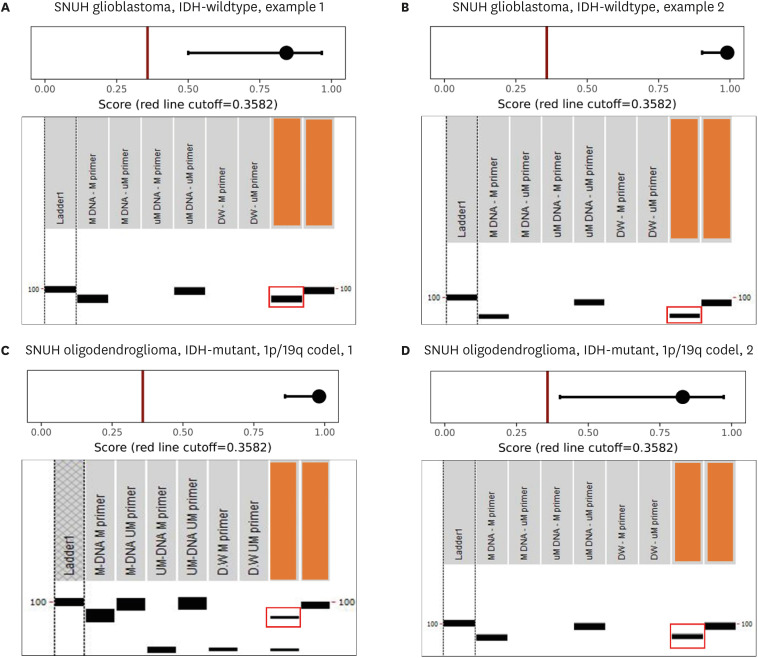
- The goal of the methylation classifier in brain tumor classification is to accurately classify tumors based on their methylation profiles. Accurate brain tumor diagnosis is the first step for healthcare professionals to predict tumor prognosis and establish personalized treatment plans for patients. The methylation classifier can be used to perform classification on tumor samples with diagnostic difficulties due to ambiguous histology or mismatch between histopathology and molecular signatures, i.e., not otherwise specified (NOS) cases or not elsewhere classified (NEC) cases, aiding in pathological decision-making. Here, the authors elucidate upon the application of a methylation classifier as a tool to mitigate the inherent complexities associated with the pathological evaluation of brain tumors, even when pathologists are experts in histopathological diagnosis and have access to enough molecular genetic information. Also, it should be emphasized that methylome cannot classify all types of brain tumors, and it often produces erroneous matches even with high matching scores, so, excessive trust is prohibited. The primary issue is the considerable difficulty in obtaining reference data regarding the methylation profile of each type of brain tumor. This challenge is further amplified when dealing with recently identified novel types or subtypes of brain tumors, as such data are not readily accessible through open databases or authors of publications. An additional obstacle arises from the fact that methylation classifiers are primarily research-based, leading to the unavailability of charging patients. It is important to note that the application of methylation classifiers may require specialized laboratory techniques and expertise in DNA methylation analysis.
Keyword
Figure
Reference
-
1. Moore LD, Le T, Fan G. DNA methylation and its basic function. Neuropsychopharmacology. 2013; 38(1):23–38. PMID: 22781841.
Article2. Delpu Y, Cordelier P, Cho WC, Torrisani J. DNA methylation and cancer diagnosis. Int J Mol Sci. 2013; 14(7):15029–15058. PMID: 23873296.
Article3. Pratt D, Sahm F, Aldape K. DNA methylation profiling as a model for discovery and precision diagnostics in neuro-oncology. Neuro Oncol. 2021; 23(23):Suppl 5. S16–S29. PMID: 34725697.
Article4. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 2021; 23(8):1231–1251. PMID: 34185076.
Article5. Gerges N, Fontebasso AM, Albrecht S, Faury D, Jabado N. Pediatric high-grade astrocytomas: a distinct neuro-oncological paradigm. Genome Med. 2013; 5(7):66. PMID: 23906214.
Article6. Capper D, Jones DT, Sill M, Hovestadt V, Schrimpf D, Sturm D, et al. DNA methylation-based classification of central nervous system tumours. Nature. 2018; 555(7697):469–474. PMID: 29539639.7. Chen Y, Yan Y, Xu M, Chen W, Lin J, Zhao Y, et al. Development of a machine learning classifier for brain tumors diagnosis based on DNA methylation profile. Front Bioinform. 2021; 1:744345. PMID: 36303797.
Article8. Petruzzellis G, Alessi I, Colafati GS, Diomedi-Camassei F, Ciolfi A, Pedace L, et al. Role of DNA methylation profile in diagnosing astroblastoma: a case report and literature review. Front Genet. 2019; 10:391. PMID: 31114608.
Article9. Perez E, Capper D. Invited review: DNA methylation-based classification of paediatric brain tumours. Neuropathol Appl Neurobiol. 2020; 46(1):28–47. PMID: 31955441.
Article10. Huse JT, Snuderl M, Jones DT, Brathwaite CD, Altman N, Lavi E, et al. Polymorphous low-grade neuroepithelial tumor of the young (PLNTY): an epileptogenic neoplasm with oligodendroglioma-like components, aberrant CD34 expression, and genetic alterations involving the MAP kinase pathway. Acta Neuropathol. 2017; 133(3):417–429. PMID: 27812792.
Article11. Reinhardt A, Stichel D, Schrimpf D, Sahm F, Korshunov A, Reuss DE, et al. Anaplastic astrocytoma with piloid features, a novel molecular class of IDH wildtype glioma with recurrent MAPK pathway, CDKN2A/B and ATRX alterations. Acta Neuropathol. 2018; 136(2):273–291. PMID: 29564591.
Article12. Korshunov A, Schrimpf D, Ryzhova M, Sturm D, Chavez L, Hovestadt V, et al. H3-/IDH-wild type pediatric glioblastoma is comprised of molecularly and prognostically distinct subtypes with associated oncogenic drivers. Acta Neuropathol. 2017; 134(3):507–516. PMID: 28401334.
Article13. Guerreiro Stucklin AS, Ryall S, Fukuoka K, Zapotocky M, Lassaletta A, Li C, et al. Alterations in ALK/ROS1/NTRK/MET drive a group of infantile hemispheric gliomas. Nat Commun. 2019; 10(1):4343. PMID: 31554817.
Article14. Deng MY, Sill M, Sturm D, Stichel D, Witt H, Ecker J, et al. Diffuse glioneuronal tumour with oligodendroglioma-like features and nuclear clusters (DGONC) - a molecularly defined glioneuronal CNS tumour class displaying recurrent monosomy 14. Neuropathol Appl Neurobiol. 2020; 46(5):422–430. PMID: 31867747.
Article15. Sturm D, Orr BA, Toprak UH, Hovestadt V, Jones DT, Capper D, et al. New brain tumor entities emerge from molecular classification of CNS-PNETs. Cell. 2016; 164(5):1060–1072. PMID: 26919435.16. Roohani S, Ehret F, Perez E, Capper D, Jarosch A, Flörcken A, et al. Sarcoma classification by DNA methylation profiling in clinical everyday life: the Charité experience. Clin Epigenetics. 2022; 14(1):149. PMID: 36380356.
Article17. Papanicolau-Sengos A, Aldape K. DNA methylation profiling: an emerging paradigm for cancer diagnosis. Annu Rev Pathol. 2022; 17(1):295–321. PMID: 34736341.
Article18. Adeoye J, Wan CC, Zheng LW, Thomson P, Choi SW, Su YX. Machine learning-based genome-wide salivary DNA methylation analysis for identification of noninvasive biomarkers in oral cancer diagnosis. Cancers (Basel). 2022; 14(19):4935. PMID: 36230858.
Article19. Xiao Y, Ju L, Qian K, Jin W, Wang G, Zhao Y, et al. Non-invasive diagnosis and surveillance of bladder cancer with driver and passenger DNA methylation in a prospective cohort study. Clin Transl Med. 2022; 12(8):e1008. PMID: 35968916.
Article20. Terp SK, Stoico MP, Dybkær K, Pedersen IS. Early diagnosis of ovarian cancer based on methylation profiles in peripheral blood cell-free DNA: a systematic review. Clin Epigenetics. 2023; 15(1):24. PMID: 36788585.
Article21. Frontiers Production Office. Erratum: A DNA methylation-based panel for the prognosis and diagnosis of patients with breast cancer and its mechanisms. Front Mol Biosci. 2020; 7:596445. PMID: 33282913.22. Pan Y, Liu G, Zhou F, Su B, Li Y. DNA methylation profiles in cancer diagnosis and therapeutics. Clin Exp Med. 2018; 18(1):1–14. PMID: 28752221.
Article23. Marzese DM, Hoon DS. Emerging technologies for studying DNA methylation for the molecular diagnosis of cancer. Expert Rev Mol Diagn. 2015; 15(5):647–664. PMID: 25797072.
Article24. Li S, Wang L, Zhao Q, Wang Z, Lu S, Kang Y, et al. Genome-wide analysis of cell-free DNA methylation profiling for the early diagnosis of pancreatic cancer. Front Genet. 2020; 11:596078. PMID: 33424927.
Article25. Kang S, Li Q, Chen Q, Zhou Y, Park S, Lee G, et al. CancerLocator: non-invasive cancer diagnosis and tissue-of-origin prediction using methylation profiles of cell-free DNA. Genome Biol. 2017; 18(1):53. PMID: 28335812.
Article26. Li J, Zhao S, Lee M, Yin Y, Li J, Zhou Y, et al. Reliable tumor detection by whole-genome methylation sequencing of cell-free DNA in cerebrospinal fluid of pediatric medulloblastoma. Sci Adv. 2020; 6(42):eabb5427. PMID: 33067228.
Article27. Wu Z, Abdullaev Z, Pratt D, Chung HJ, Skarshaug S, Zgonc V, et al. Impact of the methylation classifier and ancillary methods on CNS tumor diagnostics. Neuro Oncol. 2022; 24(4):571–581. PMID: 34555175.
Article28. Pelizzola M, Ecker JR. The DNA methylome. FEBS Lett. 2011; 585(13):1994–2000. PMID: 21056564.
Article29. Li E, Zhang Y. DNA methylation in mammals. Cold Spring Harb Perspect Biol. 2014; 6(5):a019133. PMID: 24789823.
Article30. Law PP, Holland ML. DNA methylation at the crossroads of gene and environment interactions. Essays Biochem. 2019; 63(6):717–726. PMID: 31782496.
Article31. Pasha HA, Rezk NA, Riad MA. Circulating cell free nuclear DNA, mitochondrial DNA and global DNA methylation: potential noninvasive biomarkers for breast cancer diagnosis. Cancer Invest. 2019; 37(9):432–439. PMID: 31516038.
Article32. Younesian S, Yousefi AM, Momeny M, Ghaffari SH, Bashash D. The DNA methylation in neurological diseases. Cells. 2022; 11(21):3439. PMID: 36359835.
Article33. Mazzone R, Zwergel C, Artico M, Taurone S, Ralli M, Greco A, et al. The emerging role of epigenetics in human autoimmune disorders. Clin Epigenetics. 2019; 11(1):34. PMID: 30808407.
Article34. Reuss DE, Kratz A, Sahm F, Capper D, Schrimpf D, Koelsche C, et al. Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. Acta Neuropathol. 2015; 130(3):407–417. PMID: 26087904.
Article35. Lewandowska J, Bartoszek A. DNA methylation in cancer development, diagnosis and therapy--multiple opportunities for genotoxic agents to act as methylome disruptors or remediators. Mutagenesis. 2011; 26(4):475–487. PMID: 21551264.
Article36. Zhang Z, Li D, Wu M, Xiang B, Wang L, Zhou M, et al. Promoter hypermethylation-mediated inactivation of LRRC4 in gliomas. BMC Mol Biol. 2008; 9(1):99. PMID: 18976507.
Article37. Tao F, Zhang Z. Editorial: Epigenetic drugs and therapeutic resistance for epithelial malignancies. Front Pharmacol. 2023; 14:1208518. PMID: 37229257.
Article38. Levenson VV. DNA methylation as a universal biomarker. Expert Rev Mol Diagn. 2010; 10(4):481–488. PMID: 20465502.
Article39. Sharma T, Schwalbe EC, Williamson D, Sill M, Hovestadt V, Mynarek M, et al. Second-generation molecular subgrouping of medulloblastoma: an international meta-analysis of Group 3 and Group 4 subtypes. Acta Neuropathol. 2019; 138(2):309–326. PMID: 31076851.
Article40. Schwalbe EC, Lindsey JC, Nakjang S, Crosier S, Smith AJ, Hicks D, et al. Novel molecular subgroups for clinical classification and outcome prediction in childhood medulloblastoma: a cohort study. Lancet Oncol. 2017; 18(7):958–971. PMID: 28545823.
Article41. Northcott PA, Buchhalter I, Morrissy AS, Hovestadt V, Weischenfeldt J, Ehrenberger T, et al. The whole-genome landscape of medulloblastoma subtypes. Nature. 2017; 547(7663):311–317. PMID: 28726821.
Article42. Coltin H, Sundaresan L, Smith KS, Skowron P, Massimi L, Eberhart CG, et al. Subgroup and subtype-specific outcomes in adult medulloblastoma. Acta Neuropathol. 2021; 142(5):859–871. PMID: 34409497.
Article43. Miranda Kuzan-Fischer C, Juraschka K, Taylor MD. Medulloblastoma in the molecular era. J Korean Neurosurg Soc. 2018; 61(3):292–301. PMID: 29742881.
Article44. Bleeker L, Kouwenhoven MC, de Heer I, Lissenberg-Witte BI, Gijsbers AH, Dubbink HJ, et al. Medulloblastoma in adults: evaluation of the Dutch society for neuro-oncology treatment protocol. J Neurooncol. 2023; 162(1):225–235. PMID: 36920679.
Article45. Pajtler KW, Wen J, Sill M, Lin T, Orisme W, Tang B, et al. Molecular heterogeneity and CXorf67 alterations in posterior fossa group A (PFA) ependymomas. Acta Neuropathol. 2018; 136(2):211–226. PMID: 29909548.
Article46. Rathi KS, Arif S, Koptyra M, Naqvi AS, Taylor DM, Storm PB, et al. A transcriptome-based classifier to determine molecular subtypes in medulloblastoma. PLOS Comput Biol. 2020; 16(10):e1008263. PMID: 33119584.
Article47. Kumar R, Smith KS, Deng M, Terhune C, Robinson GW, Orr BA, et al. Clinical outcomes and patient-matched molecular composition of relapsed medulloblastoma. J Clin Oncol. 2021; 39(7):807–821. PMID: 33502920.
Article48. Pajtler KW, Witt H, Sill M, Jones DT, Hovestadt V, Kratochwil F, et al. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell. 2015; 27(5):728–743. PMID: 25965575.
Article49. Lim KY, Lee K, Shim Y, Park JW, Kim H, Kang J, et al. Molecular subtyping of ependymoma and prognostic impact of Ki-67. Brain Tumor Pathol. 2022; 39(1):1–13. PMID: 34812989.
Article50. Panwalkar P, Tamrazi B, Dang D, Chung C, Sweha S, Natarajan SK, et al. Targeting integrated epigenetic and metabolic pathways in lethal childhood PFA ependymomas. Sci Transl Med. 2021; 13(614):eabc0497. PMID: 34613815.
Article51. Baroni LV, Sundaresan L, Heled A, Coltin H, Pajtler KW, Lin T, et al. Ultra high-risk PFA ependymoma is characterized by loss of chromosome 6q. Neuro Oncol. 2021; 23(8):1360–1370. PMID: 33580238.
Article52. Kresbach C, Dorostkar MM, Suwala AK, Wefers AK, Schweizer L, Engertsberger L, et al. Neurofibromatosis type 2 predisposes to ependymomas of various localization, histology, and molecular subtype. Acta Neuropathol. 2021; 141(6):971–974. PMID: 33844070.
Article53. Lim KY, Lee KH, Phi JH, Yun H, Won JK, Choi SH, et al. ZFTA-YAP1 fusion-positive ependymoma can occur in the spinal cord: Letter to the editor. Brain Pathol. 2022; 32(1):e13020. PMID: 34506076.
Article54. Raffeld M, Abdullaev Z, Pack SD, Xi L, Nagaraj S, Briceno N, et al. High level MYCN amplification and distinct methylation signature define an aggressive subtype of spinal cord ependymoma. Acta Neuropathol Commun. 2020; 8(1):101. PMID: 32641156.
Article55. Kristensen BW, Priesterbach-Ackley LP, Petersen JK, Wesseling P. Molecular pathology of tumors of the central nervous system. Ann Oncol. 2019; 30(8):1265–1278. PMID: 31124566.
Article56. Ho B, Johann PD, Grabovska Y, De Dieu Andrianteranagna MJ, Yao F, Frühwald M, et al. Molecular subgrouping of atypical teratoid/rhabdoid tumors-a reinvestigation and current consensus. Neuro Oncol. 2020; 22(5):613–624. PMID: 31889194.
Article57. Holdhof D, Johann PD, Spohn M, Bockmayr M, Safaei S, Joshi P, et al. Atypical teratoid/rhabdoid tumors (ATRTs) with SMARCA4 mutation are molecularly distinct from SMARCB1-deficient cases. Acta Neuropathol. 2021; 141(2):291–301. PMID: 33331994.
Article58. Johann PD, Erkek S, Zapatka M, Kerl K, Buchhalter I, Hovestadt V, et al. Atypical teratoid/rhabdoid tumors are comprised of three epigenetic subgroups with distinct enhancer landscapes. Cancer Cell. 2016; 29(3):379–393. PMID: 26923874.
Article59. Duan Z, Yao K, Yang S, Qu Y, Ren M, Zhang Y, et al. Primary adult sellar SMARCB1/INI1-deficient tumor represents a subtype of atypical teratoid/rhabdoid tumor. Mod Pathol. 2022; 35(12):1910–1920. PMID: 35804041.
Article60. Reinhardt A, Stichel D, Schrimpf D, Koelsche C, Wefers AK, Ebrahimi A, et al. Tumors diagnosed as cerebellar glioblastoma comprise distinct molecular entities. Acta Neuropathol Commun. 2019; 7(1):163. PMID: 31661039.
Article61. Lucas CG, Sloan EA, Gupta R, Wu J, Pratt D, Vasudevan HN, et al. Multiplatform molecular analyses refine classification of gliomas arising in patients with neurofibromatosis type 1. Acta Neuropathol. 2022; 144(4):747–765. PMID: 35945463.
Article62. Thomas DL. 2021 updates to the World Health Organization classification of adult-type and pediatric-type diffuse gliomas: a clinical practice review. Chin Clin Oncol. 2023; 12(1):7. PMID: 36922356.
Article63. Lim SD, Kim SI, Park JW, Won JK, Kim SK, Phi JH, et al. Emerging glioneuronal and neuronal tumors: case-based review. Brain Tumor Pathol. 2022; 39(2):65–78. PMID: 35048219.
Article64. Rao S, Sugur H, Konar S, Arivazhagan A, Santosh V. MYCN amplification in spinal ependymoma: a five-year retrospective study. Neuropathology. 2023; neup.12912.
Article65. Poh B, Koso H, Momota H, Komori T, Suzuki Y, Yoshida N, et al. Foxr2 promotes formation of CNS-embryonal tumors in a Trp53-deficient background. Neuro Oncol. 2019; 21(8):993–1004. PMID: 30976792.
Article66. Verburg N, Barthel FP, Anderson KJ, Johnson KC, Koopman T, Yaqub MM, et al. Spatial concordance of DNA methylation classification in diffuse glioma. Neuro Oncol. 2021; 23(12):2054–2065. PMID: 34049406.
Article67. Bure IV, Nemtsova MV, Kuznetsova EB. Histone modifications and non-coding RNAs: mutual epigenetic regulation and role in pathogenesis. Int J Mol Sci. 2022; 23(10):5801. PMID: 35628612.
Article68. Beyes S, Bediaga NG, Zippo A. An epigenetic perspective on intra-tumour heterogeneity: novel insights and new challenges from multiple fields. Cancers (Basel). 2021; 13(19):4969. PMID: 34638453.
Article69. Roy S, Coldren C, Karunamurthy A, Kip NS, Klee EW, Lincoln SE, et al. Standards and guidelines for validating next-generation sequencing bioinformatics pipelines: a joint recommendation of the Association for Molecular Pathology and the College of American Pathologists. J Mol Diagn. 2018; 20(1):4–27. PMID: 29154853.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- DNA methylation: an epigenetic mark of cellular memory
- DNA Methylation in Brain and Liver Tissues of Mice Infected with Scrapie Agent
- Relationship between Methylation Status of p16 Tumor Suppressor Gene and Clinicopathologic Behavior of Stomach Cancer
- Aberrant CpG Islands Hypermethylation Profiles in Malignant Gliomas
- Analysis of Epigenetic Marker of Bladder Cancer