J Korean Med Sci.
2023 Nov;38(43):e338. 10.3346/jkms.2023.38.e338.
Mediating Role of Viral Anxiety and Insomnia in Relationship Between Work-Related Stress and Depression Among Cold Chain Workers During COVID-19 Pandemic
- Affiliations
-
- 1College of Health, Yuncheng Vocational and Technical University, Yuncheng, Shanxi, China
- 2Department of Nursing, Taiyuan Central Hospital, Shanxi Medical University, Taiyuan, Shanxi, China
- 3Department of Psychology, University of Chittagong, Chattogram, Bangladesh
- 4National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT, Australia
- 5Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2547963
- DOI: http://doi.org/10.3346/jkms.2023.38.e338
Abstract
- Background
Here we investigated whether cold chain workers’ insomnia, work-related stress, and viral anxiety contributed to their depression. Furthermore, we investigated the role of viral anxiety in mediating the association between work-related stress and depressive symptoms.
Methods
All 200 invited cold chain workers voluntarily responded to an online survey. All were working at a market in Taiyuan, Shanxi Province, China, and responsible for testing nucleic acids in imported cold chain foods and disinfecting outer packaging at government request. We collected their demographic variables and rated their symptoms using the Stress and Anxiety to Viral Epidemics-6 Items (SAVE-6), Patient Health Questionnaire-9, Insomnia Severity Index (ISI), Perceived Stress Scale (PSS), and Maslach Burnout Inventory - General Survey (MBI-GS).
Results
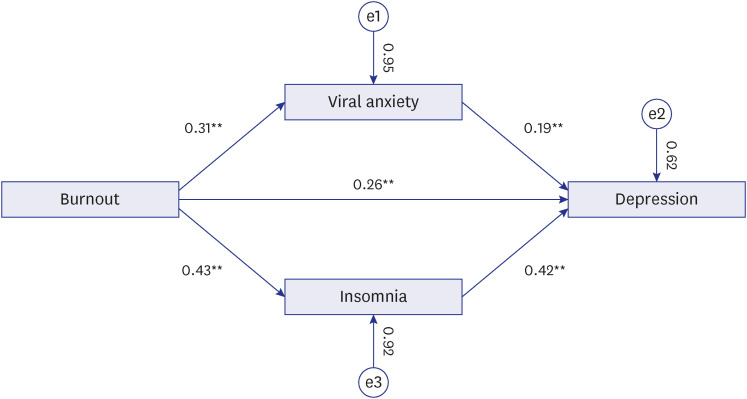
Cold chain workers’ depression was significantly correlated with higher SAVE-6 (r = 0.450, P < 0.01), ISI (r = 0.603, P < 0.01), MBI-GS (r = 0.481, P < 0.01), and PSS (r = 0.390, P < 0.01) scores. SAVE-6 score was significantly correlated with ISI (r = 0.462, P < 0.01), MBI-GS (r = 0.305, P < 0.01), and PSS (r = 0.268, P < 0.01) scores. Linear regression revealed that their depression was predicted by SAVE-6 (β = 0.183, P = 0.003), ISI (β = 0.409, P < 0.001), and MBI-GS (β = 0.236, P = 0.002, adjusted R2 = 0.440, F = 40.04, P < 0.001) scores. Mediation analysis showed that their burnout directly influenced their depression, while viral anxiety or insomnia severity mediated the influence of burnout on depression.
Conclusion
The study showed that burnout was a direct cause of depression and that viral anxiety and insomnia severity mediated the relationship between burnout and depression.
Keyword
Figure
Reference
-
1. World Health Organization. WHO Director-General’s opening remarks at the Public Hearing regarding a new international instrument on pandemic preparedness and response – 12 April 2022. Updated 2022. Accessed September 8, 2022. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-public-hearing-regarding-a-new-international-instrument-on-pandemic-preparedness-and-response---12-april-2022 .2. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2023. Accessed March 11, 2023. https://covid19.who.int/ .3. World Health Organization. WHO-convened Global Study of Origins of SARS-CoV-2: China Part | Joint WHO-China Study, 14 January-10 February 2021. Updated 2021. Accessed March 11, 2023. https://reliefweb.int/report/world/who-convened-global-study-origins-sars-cov-2-china-part-joint-who-china-study-14?gclid=Cj0KCQjwxMmhBhDJARIsANFGOSuZ7NoXqpF9m3PUGKQ4QTeFbu4jbOSDzFkh4MAZerCEANljZzfRz20aAoJIEALw_wcB .4. Wang J, Li F, Liu Z, Li N. COVID-19 outbreaks linked to imported frozen food in China: status and challege. China CDC Wkly. 2022; 4(22):483–487. PMID: 35812776.5. Liu L, Zhang M, Chen H, Xian J, Cao H, Zhou X, et al. COVID-19 vaccine acceptance among cold-chain workers in Shenzhen, China: a cross-sectional survey. Hum Vaccin Immunother. 2022; 18(5):2056400. PMID: 35468306.
Article6. Liu P, Yang M, Zhao X, Guo Y, Wang L, Zhang J, et al. Cold-chain transportation in the frozen food industry may have caused a recurrence of COVID-19 cases in destination: successful isolation of SARS-CoV-2 virus from the imported frozen cod package surface. Biosaf Health. 2020; 2(4):199–201. PMID: 33235990.
Article7. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020; 33(2):e100213. PMID: 32215365.
Article8. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020; 17(5):1729. PMID: 32155789.
Article9. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020; 3(3):e203976. PMID: 32202646.
Article10. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020; 88:901–907. PMID: 32437915.
Article11. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020; 3(9):e2019686. PMID: 32876685.
Article12. Cui R, Fiske A. Relation between depression symptoms and suicide risk in adults and older adults: a brief report. J Appl Gerontol. 2022; 41(1):176–180. PMID: 33174516.
Article13. Dong L, Freedman VA, Mendes de Leon CF. The association of comorbid depression and anxiety symptoms with disability onset in older adults. Psychosom Med. 2020; 82(2):158–164. PMID: 31688675.
Article14. Yip PS, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010; 31(2):86–92. PMID: 20418214.15. Al Omari O, Al Sabei S, Al Rawajfah O, Abu Sharour L, Aljohani K, Alomari K, et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an online cross-sectional multicountry study. Depress Res Treat. 2020; 2020:8887727. PMID: 33062331.
Article16. Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020; 11:1540. PMID: 32655463.
Article17. Çıkrıkçı Ö, Çıkrıkçı N, Griffiths M. Fear of COVID-19, stress and depression: a meta-analytic test of the mediating role of anxiety. Psychol Psychother. 2022; 95(4):853–874. PMID: 35670451.
Article18. Liu Z, Liu R, Zhang Y, Zhang R, Liang L, Wang Y, et al. Association between perceived stress and depression among medical students during the outbreak of COVID-19: The mediating role of insomnia. J Affect Disord. 2021; 292:89–94. PMID: 34107425.
Article19. Cho E, Lee D, Cho IK, Lee J, Ahn J, Bang YR. Insomnia mediate the influence of reassurance-seeking behavior and viral anxiety on preoccupation with COVID-19 among the general population. Sleep Med Rev. 2022; 13(2):68–74.
Article20. Yıldırım M, Solmaz F. COVID-19 burnout, COVID-19 stress and resilience: initial psychometric properties of COVID-19 Burnout Scale. Death Stud. 2022; 46(3):524–532. PMID: 32915702.
Article21. Schaufeli WB, Greenglass ER. Introduction to special issue on burnout and health. Psychol Health. 2001; 16(5):501–510. PMID: 22804495.
Article22. Shah K, Chaudhari G, Kamrai D, Lail A, Patel RS. How essential is to focus on physician’s health and burnout in coronavirus (COVID-19) pandemic? Cureus. 2020; 12(4):e7538. PMID: 32377486.
Article23. Alkhamees AA, Assiri H, Alharbi HY, Nasser A, Alkhamees MA. Burnout and depression among psychiatry residents during COVID-19 pandemic. Hum Resour Health. 2021; 19(1):46. PMID: 33823857.
Article24. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020; 17(11):4065. PMID: 32517294.
Article25. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020; 29(4):e13074. PMID: 32410272.
Article26. Ye B, Wu D, Wang P, Im H, Liu M, Wang X, et al. COVID-19 stressors and poor sleep quality: the mediating role of rumination and the moderating role of emotion regulation strategies. Int J Behav Med. 2022; 29(4):416–425. PMID: 34581977.
Article27. Grandner MA, Malhotra A. Connecting insomnia, sleep apnoea and depression. Respirology. 2017; 22(7):1249–1250. PMID: 28556352.
Article28. Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013; 36(7):1059–1068. PMID: 23814343.
Article29. Golonka K, Mojsa-Kaja J, Blukacz M, Gawłowska M, Marek T. Occupational burnout and its overlapping effect with depression and anxiety. Int J Occup Med Environ Health. 2019; 32(2):229–244. PMID: 30855601.
Article30. Chung S, Ahn MH, Lee S, Kang S, Suh S, Shin YW. The Stress and Anxiety to Viral Epidemics-6 items (SAVE-6) scale: a new instrument for assessing the anxiety response of general population to the viral epidemic during the COVID-19 pandemic. Front Psychol. 2021; 12:669606. PMID: 34149565.
Article31. Chung S, Kim HJ, Ahn MH, Yeo S, Lee J, Kim K, et al. Development of the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) scale for assessing work-related stress and anxiety in healthcare workers in response to viral epidemics. J Korean Med Sci. 2021; 36(47):e319. PMID: 34873885.
Article32. Runlian H, Xinjie D, Ahmed O, Cho E, Chung S. Application of Stress and Anxiety to Viral Epidemics-6 to measure the anxiety response of cold chain practitioners during the COVID-19 post-pandemic era in China. Psychiatry Investig. 2023; 20(2):75–83.
Article33. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.34. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014; 36(5):539–544. PMID: 25023953.
Article35. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011; 34(5):601–608. PMID: 21532953.
Article36. Yu DS. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010; 66(10):2350–2359. PMID: 20722803.
Article37. Cohen S, Kamarck T, Mermelstein R. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Health Soc Behav. 1983; 24(4):385–396. PMID: 6668417.38. Lu W, Bian Q, Wang W, Wu X, Wang Z, Zhao M. Chinese version of the Perceived Stress Scale-10: a psychometric study in Chinese university students. PLoS One. 2017; 12(12):e0189543. PMID: 29252989.
Article39. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001; 52:397–422. PMID: 11148311.
Article40. Khan S, Siddique R, Li H, Ali A, Shereen MA, Bashir N, et al. Impact of coronavirus outbreak on psychological health. J Glob Health. 2020; 10(1):010331. PMID: 32355556.
Article41. North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013; 310(5):507–518. PMID: 23925621.42. Weilenmann S, Ernst J, Petry H, Pfaltz MC, Sazpinar O, Gehrke S, et al. Health care workers’ mental health during the first weeks of the SARS-CoV-2 pandemic in Switzerland-a cross-sectional study. Front Psychiatry. 2021; 12:594340. PMID: 33815162.
Article43. Wurm W, Vogel K, Holl A, Ebner C, Bayer D, Mörkl S, et al. Depression-burnout overlap in physicians. PLoS One. 2016; 11(3):e0149913. PMID: 26930395.
Article44. Ding Y, Qu J, Yu X, Wang S. The mediating effects of burnout on the relationship between anxiety symptoms and occupational stress among community healthcare workers in China: a cross-sectional study. PLoS One. 2014; 9(9):e107130. PMID: 25211025.
Article45. Erbay E, Arslan K, Hatipoğlu E, Yildirim T. The quality of life, depression levels and coping styles of patients on kidney transplant waiting list. Soc Work Public Health. 2021; 36(4):432–447. PMID: 33771077.
Article46. Schrack AP, Joyce-Beaulieu D, MacInnes JW, Kranzler JH, Zaboski BA 2nd, McNamara JP. Intelligence and academic achievement in inpatient adolescents with comorbid anxiety and depression. Bull Menninger Clin. 2021; 85(1):23–41. PMID: 33750201.
Article47. Parent-Lamarche A, Marchand A, Saade S. Does depression mediate the effect of work organization conditions on job performance? J Occup Environ Med. 2020; 62(4):296–302. PMID: 31977926.
Article48. Ghalichi L, Pournik O, Ghaffari M, Vingard E. Sleep quality among health care workers. Arch Iran Med. 2013; 16(2):100–103. PMID: 23360632.49. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016; 16(1):375. PMID: 27816065.
Article50. Bajaj S, Blair KS, Schwartz A, Dobbertin M, Blair RJ. Worry and insomnia as risk factors for depression during initial stages of COVID-19 pandemic in India. PLoS One. 2020; 15(12):e0243527. PMID: 33301508.
Article51. Jacobson NC, Newman MG. Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychol Bull. 2017; 143(11):1155–1200. PMID: 28805400.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mediating Effect of Public Service Motivation and Resilience on the Association Between Work-Related Stress and Work Engagement of Public Workers in the COVID-19 Pandemic
- Effects of Depression and Resilience of Public Workers on Work-related Stress and Anxiety in Response to the COVID-19 Pandemic
- Validation of the Pandemic Grief Risk Factors and Its Relationship With Work-Related Stress and Grief Reaction Among Healthcare Workers Who Witnessed Patient Deaths
- Mediating Effects of ReassuranceSeeking Behavior or Obsession With COVID-19 on the Association Between Intolerance of Uncertainty and Viral Anxiety Among Healthcare Workers in Korea
- Grief Response of Nursing Professionals Is Associated With Their Depression, Loneliness, Insomnia, and Work-Related Stress While Working in COVID-19 Inpatients Wards