J Korean Med Sci.
2023 Nov;38(43):e337. 10.3346/jkms.2023.38.e337.
Comprehensive Measurement of the Burden of Disease due to Adverse Events: A New Analysis of the CrossSectional Patient Safety Incident Inquiry
- Affiliations
-
- 1Department of Nursing, Chung-Ang University, Seoul, Korea
- 2Department of Preventive Medicine, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Nursing, College of Nursing, Inje University, Gimhae, Korea
- 4Department of Preventive Medicine, Asan Medical Institute of Convergence Science and Technology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 5Department of Preventive Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2547962
- DOI: http://doi.org/10.3346/jkms.2023.38.e337
Abstract
- Background
A methodology for comprehensively and reasonably measuring the burden of disease due to adverse events has yet to be clearly established. In this study, a new and systematic method for measuring the burden of disease due to adverse events was tested by utilizing the results of a medical record review, which is commonly used as a gold standard.
Methods
Using the characteristics of preventable adverse events identified in the 2019 Patient Safety Incidents Inquiry (PSII), conducted to monitor the level of patient safety in Korea accurately, the resulting disability-adjusted life years (DALYs) and economic costs were estimated. DALYs were calculated as the sum of the years lived with a disability for patients who suffered permanent disability, or more, due to preventable adverse events, and the years of life lost due to premature mortality was calculated for patients who died due to preventable adverse events. The economic cost was calculated using the main diagnostic codes of patients who suffered preventable adverse events, identified as prolonged hospitalization in PSII, and the average medical cost by disease category and age group.
Results
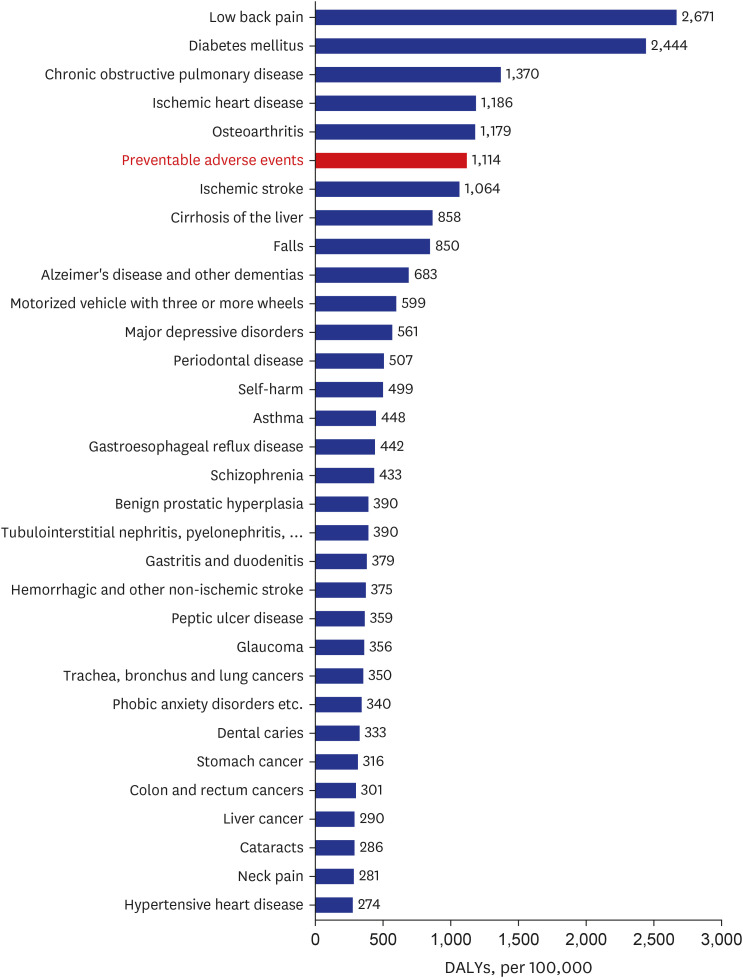
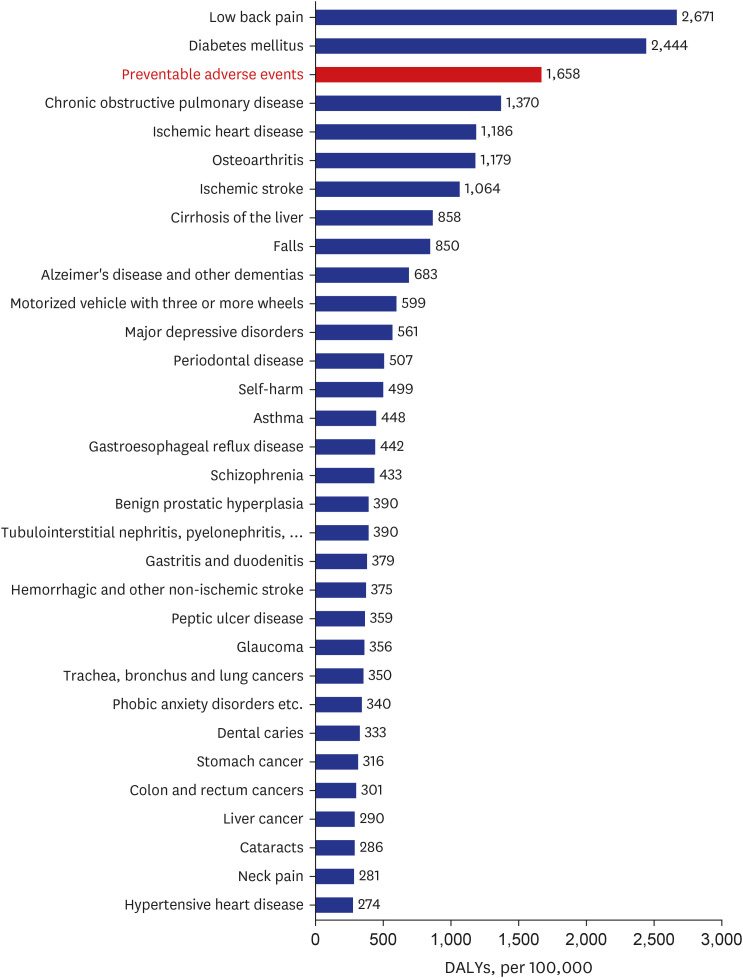
Estimates of DALYs due to preventable adverse events were 1,114.4 DALYs per 100,000 population for the minimum standard and 1,658.5 DALYs per 100,000 population for the maximum standard. Compared to the 2015 Korea Burden of Disease results, the ranking of DALYs due to preventable adverse events was sixth for the minimum standard and third for the maximum standard. The annual medical cost of adverse events in 2016 was estimated to be approximately Korean Republic Won (KRW) 870 billion (700 million US dollars). Medical expenses due to preventable adverse events were calculated to be approximately KRW 150 billion (120 million US dollars) as a minimum standard and approximately KRW 300 billion (240 million US dollars) as a maximum standard.
Conclusion
If this more standard method of systematically calculating the disease burden due to adverse events is used, it will be possible to compare the size of the patient safety problem with that of other diseases. The results of this study indicate that we still need to pay more attention to the issue of patient safety.
Figure
Reference
-
1. Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, D.C., USA: National Academies Press;1999.2. Pronovost PJ, Goeschel CA, Marsteller JA, Sexton JB, Pham JC, Berenholtz SM. Framework for patient safety research and improvement. Circulation. 2009; 119(2):330–337. PMID: 19153284.
Article3. World Health Organization. Regional Office for Africa. Guide for developing national patient safety policy and strategic plan. Updated 2014. Accessed March 1, 2023. https://apps.who.int/iris/handle/10665/206546 .4. World Health Organization. Global patient safety action plan 2021–2030: towards eliminating avoidable harm in health care. Updated 2021. Accessed March 1, 2023. https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan .5. Liang C, Miao Q, Kang H, Vogelsmeier A, Hilmas T, Wang J, et al. Leveraging patient safety research: efforts made fifteen years since to err is human. Stud Health Technol Inform. 2019; 264:983–987. PMID: 31438071.6. Borzecki AM, Rosen AK. Is there a ‘best measure’ of patient safety? BMJ Qual Saf. 2020; 29(3):185–188.
Article7. Nauman J, Soteriades ES, Hashim MJ, Govender R, Al Darmaki RS, Al Falasi RJ, et al. Global incidence and mortality trends due to adverse effects of medical treatment, 1990–2017: a systematic analysis from the global burden of diseases, injuries and risk factors study. Cureus. 2020; 12(3):e7265. PMID: 32195071.
Article8. McDonald SA, Nijsten D, Bollaerts K, Bauwens J, Praet N, van der Sande M, et al. Methodology for computing the burden of disease of adverse events following immunization. Pharmacoepidemiol Drug Saf. 2018; 27(7):724–730. PMID: 29575242.
Article9. Kim YE, Jung YS, Ock M, Yoon SJ. DALY estimation approaches: understanding and using the incidence-based approach and the prevalence-based approach. J Prev Med Public Health. 2022; 55(1):10–18. PMID: 35135044.
Article10. Kim YE, Jung YS, Ock M, Yoon SJ. A review of the types and characteristics of healthy life expectancy and methodological issues. J Prev Med Public Health. 2022; 55(1):1–9. PMID: 35135043.
Article11. Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014; 20(4):327–337. PMID: 25548737.
Article12. Brown P, McArthur C, Newby L, Lay-Yee R, Davis P, Briant R. Cost of medical injury in New Zealand: a retrospective cohort study. J Health Serv Res Policy. 2002; 7(Suppl 1):S29–S34. PMID: 12175432.
Article13. Hoogervorst-Schilp J, Langelaan M, Spreeuwenberg P, de Bruijne MC, Wagner C. Excess length of stay and economic consequences of adverse events in Dutch hospital patients. BMC Health Serv Res. 2015; 15(1):531. PMID: 26626729.
Article14. Kjellberg J, Wolf RT, Kruse M, Rasmussen SR, Vestergaard J, Nielsen KJ, et al. Costs associated with adverse events among acute patients. BMC Health Serv Res. 2017; 17(1):651. PMID: 28903748.
Article15. Adler L, Yi D, Li M, McBroom B, Hauck L, Sammer C, et al. Impact of inpatient harms on hospital finances and patient clinical outcomes. J Patient Saf. 2018; 14(2):67–73. PMID: 25803176.
Article16. Khan MA, Soteriades ES, King J, Govender R, Hashim MJ, Masood-Husain S, et al. Global trends and forecast of the burden of adverse effects of medical treatment: epidemiological analysis based on the global burden of disease study. Cureus. 2020; 12(3):e7250. PMID: 32195068.
Article17. Kim MJ, Seo HJ, Koo HM, Ock M, Hwang JI, Lee SI. The Korea National Patient Safety incidents inquiry survey: characteristics of adverse events identified through medical records review in regional public hospitals. J Patient Saf. 2022; 18(5):382–388. PMID: 35948288.
Article18. Kim MJ, Seo HJ, Koo HM, Ock M, Hwang JI, Lee SI. The Korea National Patient Safety incidents inquiry survey: feasibility of medical record review for detecting adverse events in regional public hospitals. J Patient Saf. 2022; 18(5):389–395. PMID: 35067623.
Article19. Ock M, Lee JY, Oh IH, Park H, Yoon SJ, Jo MW. Disability weights measurement for 228 causes of disease in the Korean Burden of Disease Study 2012. J Korean Med Sci. 2016; 31(Suppl 2):Suppl 2. S129–S138. PMID: 27775250.
Article20. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019; 34(Suppl 1):e75. PMID: 30923488.
Article21. Statistics Korea. Life table. Updated 2022. Accessed March 1, 2023. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42&conn_path=I3 .22. Health Insurance Review and Assessment Services, National Health Insurance Service. 2016 Statistical yearbook of healthcare insurance. Updated 2017. Accessed March 1, 2023. https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045020000&brdScnBltNo=4&brdBltNo=2309&pageIndex=1 .23. Kim GH, Park GC, Chae S, Lee DH, Sun JY. Status of medical service use as of 2016. Updated 2019. Accessed March 1, 2023. https://www.mohw.go.kr/react/gm/sgm0704vw.jsp?PAR_MENU_ID=13&MENU_ID=13040801&CONT_SEQ=356232&PAR_CONT_SEQ=355637 .24. Klein DO, Rennenberg RJ, Koopmans RP, Prins MH. A systematic review of methods for medical record analysis to detect adverse events in hospitalized patients. J Patient Saf. 2021; 17(8):e1234–e1240. PMID: 32168280.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Nurses' Incident Reporting Attitude, Perception of Importance on Patient Safety Management, and Patient Safety Culture on the Reporting of Patient Safety Events
- Analysis of Patient Safety Incident in Korea
- Factors Associated with Patient Safety Incidents in Long-Term Care Hospitals: A Secondary Data Analysis
- Factors Affecting the Degree of Harm from Fall Incidents in Hospitals
- Comparative Analysis of Terminology and Classification Related to Risk Management of Radiotherapy