Ewha Med J.
2023 Oct;46(4):e15. 10.12771/emj.2023.e15.
The Recent Surgical Treatment of Elbow Pain
- Affiliations
-
- 1Department of Orthopedic Surgery, St. Carolus Hospital, Faculty of Medicine, Universitas Trisakti, Jakarta, Indonesia
- 2Department of Orthopedic Surgery, Asan Medical Center, College of Medicine, Ulsan University, Seoul, Korea
- 3Department of Orthopedic Surgery, Uijeongbu Eulji Medical Center, College of Medicine, Eulji University, Uijeongbu, Korea
- KMID: 2547919
- DOI: http://doi.org/10.12771/emj.2023.e15
Abstract
- The review article explores recent advances in the surgical treatment of elbow pain, a common ailment that can significantly impair daily functioning. With a surge in elbow-related conditions such as tennis elbow, osteoarthritis, and nerve compression disorders, the necessity for surgical approaches has become paramount. This article provides an overview of the cutting-edge procedures now available, including minimally invasive arthroscopic surgery. These modern methods have been shown to significantly reduce recovery times and improve overall patient outcomes. The combination of surgical management and targeted rehabilitation ensures a comprehensive and personalized treatment plan for patients with various elbow pathologies. This article aims to shed light on these recent surgical interventions and their potential for advancing the management of elbow pain, emphasizing the ongoing trend toward precision, efficiency, and patient-centered care.
Keyword
Figure
Reference
-
References
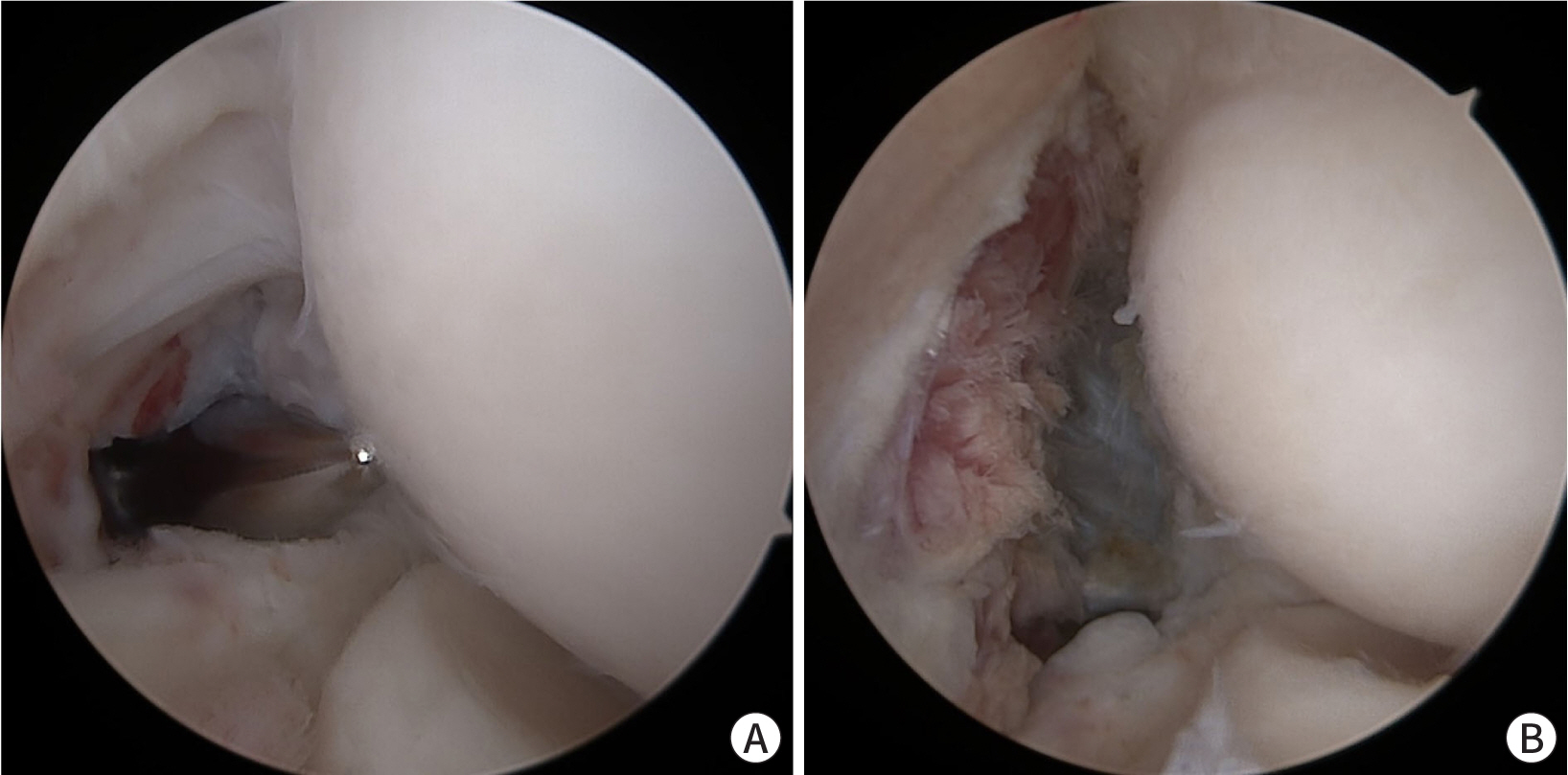
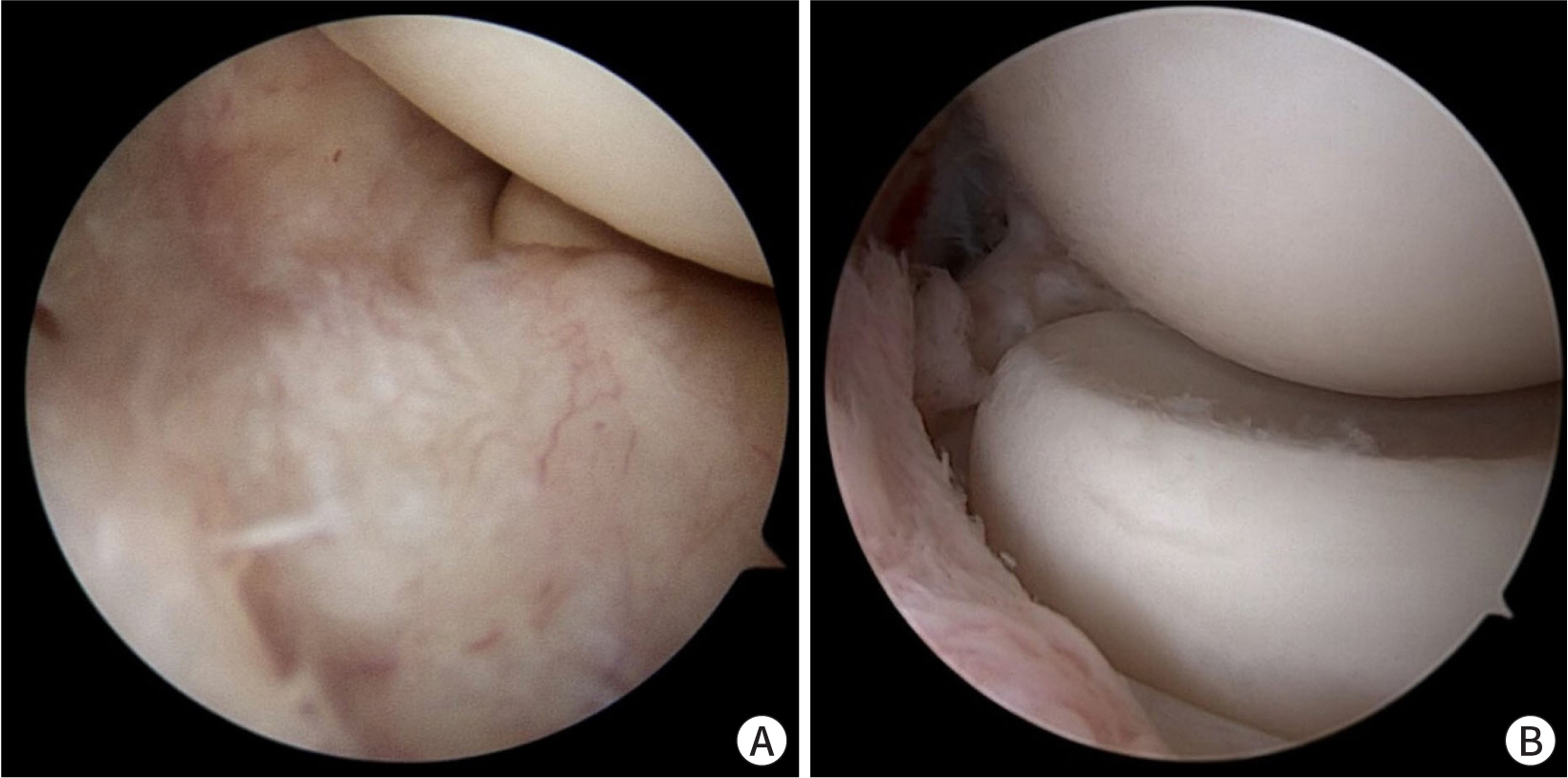
1. Kang B, Jung GH, Kholinne E, Jeon IH, Kwak JM. The elbow is the load-bearing joint during arm swing. Clin Shoulder Elb. 2023; 26((2)):126–130. DOI: 10.5397/cise.2023.00101. PMID: 37316173. PMCID: PMC10277704.2. Kwak JM, Lee KW, Jung GH, Kholinne E, Hwang SJ, Koh KH, et al. Biomechanical impact of elbow motion in elbow stiffness. Int Orthop. 2023; 47((7)):1779–1786. DOI: 10.1007/s00264-023-05781-2. PMID: 37010561.3. Concina C, Crucil M, Theodorakis E, Saggin G, Perin S, Gherlinzoni F. Complex open elbow fracture-dislocation with severe proximal ulna bone loss: a case report of massive osteochondral allograft surgical treatment. Clin Shoulder Elb. 2021; 24((3)):183–188. DOI: 10.5397/cise.2021.00220. PMID: 34488300. PMCID: PMC8423533.4. Breda G, De Marco G, Cesaraccio P, Pillastrini P. Diagnostic accuracy of clinical tests to rule out elbow fracture: a systematic review. Clin Shoulder Elb. 2023; 26((2)):182–190. DOI: 10.5397/cise.2022.00948. PMID: 35971600. PMCID: PMC10277706.5. Rouhani A, Chavoshi M, Sadeghpour A, Aslani H, Mardani-Kivi M. Outcome of open reduction and Kirschner wire fixation in pediatric radial neck fracture. Clin Shoulder Elb. 2021; 24((4)):239–244. DOI: 10.5397/cise.2021.00402. PMID: 34875730. PMCID: PMC8651599.6. Spierings KE, Schoolmeesters BJ, Doornberg JN, Eygendaal D, van den Bekerom MP. Complications of olecranon osteotomy in the treatment of distal humerus fracture. Clin Shoulder Elb. 2022; 25((2)):163–169. DOI: 10.5397/cise.2021.00591. PMID: 35545245. PMCID: PMC9185118.7. Rajani AM, Mittal ARS, Kulkarni V, Rajani K, Rajani K. Role of concomitant percutaneous pie crusting and local corticosteroid injection in lateral epicondylitis: a prospective, case control study. Clin Shoulder Elb. 2023; 26((1)):49–54. DOI: 10.5397/cise.2022.01375. PMID: 36919507. PMCID: PMC10030988.8. Kwak JM, Rotman D, Lievano JR, Fitzsimmons JS, O'Driscoll SW. The role of the lateral collateral ligament-capsule complex of the elbow under gravity varus. J Shoulder Elbow Surg. 2023; 32((1)):150–158. DOI: 10.1016/j.jse.2022.08.004. PMID: 36167291.9. Kwak JM, Rotman D, Lievano JR, Xue M, O'Driscoll SW. The role of the lateral part of the distal triceps and the anconeus in varus stability of the elbow: a biomechanical study. J Shoulder Elbow Surg. 2023; 32((1)):159–167. DOI: 10.1016/j.jse.2022.08.005. PMID: 36167289.10. Kholinne E, Liu H, Kim H, Kwak JM, Koh KH, Jeon IH. Systematic review of elbow instability in association with refractory lateral epicondylitis: myth or fact? Am J Sports Med. 2021; 49((9)):2542–2550. DOI: 10.1177/0363546520980133. PMID: 33433240.11. Kwak JM, Rotman D, Lievano JR, Fitzsimmons JS, O'Driscoll SW. Ultrasonographic measurement of elbow varus laxity with a sequential injury model of the lateral collateral ligament-capsular complex. Orthop J Sports Med. 2021; 9((11)):23259671211048941. DOI: 10.1177/23259671211048941. PMID: 34778473. PMCID: PMC8586189.12. Kwak JM, Kholinne E, Sun Y, Park JY, Koh KH, Jeon IH. Arthroscopic visualization of the medial collateral ligament of the elbow. J Shoulder Elbow Surg. 2019; 28((11)):2232–2237. DOI: 10.1016/j.jse.2019.04.040. PMID: 31300370.13. Yu JS, Manzi JE, Apostolakos JM, Carr JB, Dines JS. YouTube as a source of patient education information for elbow ulnar collateral ligament injuries: a quality control content analysis. Clin Shoulder Elb. 2022; 25((2)):145–153. DOI: 10.5397/cise.2021.00717. PMID: 35698784. PMCID: PMC9185119.14. Kholinne E, Nanda A, Liu H, Kwak JM, Kim H, Koh KH, et al. The elbow plica: a systematic review of terminology and characteristics. J Shoulder Elbow Surg. 2021; 30((5)):E185–E198. DOI: 10.1016/j.jse.2020.09.011. PMID: 33038495.15. Bonczar M, Ostrowski P, Bednarz W, Wojciechowski W, Walocha J, Koziej M. Synovial plica of the elbow: detailed measurements and how to implicate its relevance in clinical practice. Int Orthop. 2023; 47((4)):1031–1039. DOI: 10.1007/s00264-023-05726-9. PMID: 36809417. PMCID: PMC10014655.16. Bonczar M, Ostrowski P, Dziedzic M, Kasprzyk M, Obuchowicz R, Zacharias T, et al. Evaluation of lateral epicondylopathy, posterior interosseous nerve compression, and plica syndrome as co-existing causes of chronic tennis elbow. Int Orthop. 2023; 47((7)):1787–1795. DOI: 10.1007/s00264-023-05805-x. PMID: 37071147. PMCID: PMC10267267.17. Jeon IH, Liu H, Nanda A, Kim H, Kim DM, Park D, et al. Systematic review of the surgical outcomes of elbow plicae. Orthop J Sports Med. 2020; 8((10)):2325967120955162. DOI: 10.1177/2325967120955162. PMID: 33195708. PMCID: PMC7607772.18. Lubiatowski P, Wałecka J, Dzianach M, Stefaniak J, Romanowski L. Synovial plica of the elbow and its clinical relevance. EFORT Open Rev. 2020; 5((9)):549–557. DOI: 10.1302/2058-5241.5.200027. PMID: 33072407. PMCID: PMC7528666.19. Kwak JM, Sun Y, Kholinne E, Koh KH, Jeon IH. Surgical outcomes for post-traumatic stiffness after elbow fracture: comparison between open and arthroscopic procedures for intra- and extra-articular elbow fractures. J Shoulder Elbow Surg. 2019; 28((10)):1998–2006. DOI: 10.1016/j.jse.2019.06.008. PMID: 31540725.20. Kwak JM, Kholinne E, Sun Y, Alhazmi AM, Koh KH, Jeon IH. Intraobserver and interobserver reliability of the computed tomography-based radiographic classification of primary elbow osteoarthritis: comparison with plain radiograph-based classification and clinical assessment. Osteoarthritis Cartilage. 2019; 27((7)):1057–1063. DOI: 10.1016/j.joca.2019.03.004. PMID: 30922981.21. Kwak JM, Jeon IH. Surgical management for primary osteoarthritis of the elbow. J Orthop Surg. 2021; 29((1)):2309499020988174. DOI: 10.1177/2309499020988174. PMID: 33570019.22. Kwak JM, Kholinne E, Sun Y, Lim S, Koh KH, Jeon IH. Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: comparison of arthroscopic and open procedure. Arthroscopy. 2019; 35((4)):1083–1089. DOI: 10.1016/j.arthro.2018.11.057. PMID: 30871900.23. Kwak JM, Kim H, Sun Y, Kholinne E, Koh KH, Jeon IH. Arthroscopic osteocapsular arthroplasty for advanced-stage primary osteoarthritis of the elbow using a computed tomography-based classification. J Shoulder Elbow Surg. 2020; 29((5)):989–995. DOI: 10.1016/j.jse.2019.09.036. PMID: 31831280.24. Kim H, Kholinne E, Kwak JM. Ulnar nerve decompression with osteocapsular arthroplasty for primary elbow osteoarthritis. J Orthop Surg. 2022; 30((2)):10225536221109914. DOI: 10.1177/10225536221109914. PMID: 35749109.25. Colasanti CA, Boin M, Hacquebord J, Virk MS. Anterior interosseous nerve palsy in the early postoperative period after open capsular release for elbow stiffness. Clin Shoulder Elb. 2022; Nov. 21. [Epub]. DOI: 10.5397/cise.2022.00899. PMID: 37088884.26. Kwak JM, Kholinne E, Sun Y, Kim MS, Koh KH, Jeon IH. Clinical results of revision total elbow arthroplasty: comparison of infected and non-infected total elbow arthroplasty. Int Orthop. 2019; 43((6)):1421–1427. DOI: 10.1007/s00264-018-4267-2. PMID: 30617613.27. Kwak JM, So SP, Jeon IH. Staged revision still works for chronic and deep infection of total elbow arthroplasty? Sicot J. 2022; 8:21. DOI: 10.1051/sicotj/2022019. PMID: 35616598. PMCID: PMC9135019.28. Kwak JM, Koh KH, Jeon IH. Total elbow arthroplasty: clinical outcomes, complications, and revision surgery. Clin Orthop Surg. 2019; 11((4)):369–379. DOI: 10.4055/cios.2019.11.4.369. PMID: 31788158. PMCID: PMC6867907.29. Macken AA, Lans J, Miyamura S, Eberlin KR, Chen NC. Soft-tissue coverage for wound complications following total elbow arthroplasty. Clin Shoulder Elb. 2021; 24((4)):245–252. DOI: 10.5397/cise.2021.00409. PMID: 34875731. PMCID: PMC8651597.30. Pattu R, Chellamuthu G, Sellappan K, Chendrayan K. Total elbow arthroplasty for active primary tuberculosis of the elbow: a curious case of misdiagnosis. Clin Shoulder Elb. 2022; 25((2)):158–162. DOI: 10.5397/cise.2021.00304. PMID: 35045599. PMCID: PMC9185115.31. Morrow RM, McIlvian GE, Johnson J, Timmons MK. Youth throwing athletes do not show bilateral differences in medial elbow width or flexor tendon thickness. Clin Shoulder Elb. 2022; 25((3)):188–194. DOI: 10.5397/cise.2022.00766. PMID: 35791681. PMCID: PMC9471821.32. Bexkens R, van den Ende KIM, Ogink PT, van Bergen CJA, van den Bekerom MPJ, Eygendaal D. Clinical outcome after arthroscopic debridement and microfracture for osteochondritis dissecans of the capitellum. Am J Sports Med. 2017; 45((10)):2312–2318. DOI: 10.1177/0363546517704842. PMID: 28520461.33. Adams JE, Fowler J, Osterman M, Steinmann S. Nerve conditions of the upper limb: how not to miss or mismanage. Instr Course Lect. 2023; 72:627–636.34. Patterson JMM, Medina MA, Yang A, Mackinnon SE. Posterior interosseous nerve compression in the forearm, AKA radial tunnel syndrome: a clinical diagnosis. Hand. 2022; Sep. 8. [Epub]. DOI: 10.1177/15589447221122822. PMID: 36082441.35. Węgiel A, Karauda P, Zielinska N, Tubbs RS, Olewnik Ł. Radial nerve compression: anatomical perspective and clinical consequences. Neurosurg Rev. 2023; 46((1)):53. DOI: 10.1007/s10143-023-01944-2. PMID: 36781706. PMCID: PMC9925568.36. Wolf JM, Patel R, Ghosh K. Radial tunnel syndrome: review and best evidence. J Am Acad Orthop Surg. 2023; 31((15)):813–819. DOI: 10.5435/JAAOS-D-23-00314. PMID: 37276490.37. Tang JB. Some misconceptions in the treatment of cubital tunnel syndrome, radial tunnel syndrome, and median nerve compression in the forearm. Hand Clin. 2022; 38((3)):321–328. DOI: 10.1016/j.hcl.2022.02.003. PMID: 35985756.38. Shin W, Kang T, Han J. Cubital tunnel syndrome associated with previous ganglion cyst excision in the elbow: a case report. Clin Shoulder Elb. 2022; Nov. 11. [Epub]. DOI: 10.5397/cise.2022.01102.39. Kholinne E, Alsharidah MM, Almutair O, Aljasser S, Alhothali W, Kwak JM, et al. Revision surgery for refractory cubital tunnel syndrome: a systematic review. Orthop Traumatol Surg Res. 2019; 105((5)):867–876. DOI: 10.1016/j.otsr.2019.03.020. PMID: 31331798.