Obstet Gynecol Sci.
2023 Nov;66(6):572-583. 10.5468/ogs.23142.
Randomized control trial to compare effects of ultra-low dose (Ethinylestradiol 20 μg or 15 μg) with low dose (Ethinylestradiol 30 μg) hormonal pills on lipid discordance in non-obese PCOS women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Rampurhat Government Medical College and Hospital, Birbhum, India
- 2Diamond Harbour Government Medical College and Hospital, Diamond Harbour, India
- 3Chittaranjan Seva Sadan College of Obstetrics Gynaecology and Child Health Hospital, Kolkata, India
- 4Adani Enterprises Ltd, Kolkata, India
- KMID: 2547858
- DOI: http://doi.org/10.5468/ogs.23142
Abstract
Objective
Regular users of hormonal contraceptive pills show marked heterogeneity in metabolic effects with variations in compositions. This might be due to choice of outcome variables for comparison. Total cholesterol-high-density lipoprotein ratio (TC/HDL) discordance with low-density lipoprotein (LDL-C) has now become an established marker of future risk for atherosclerotic cardiovascular disease and stable to variations in user.
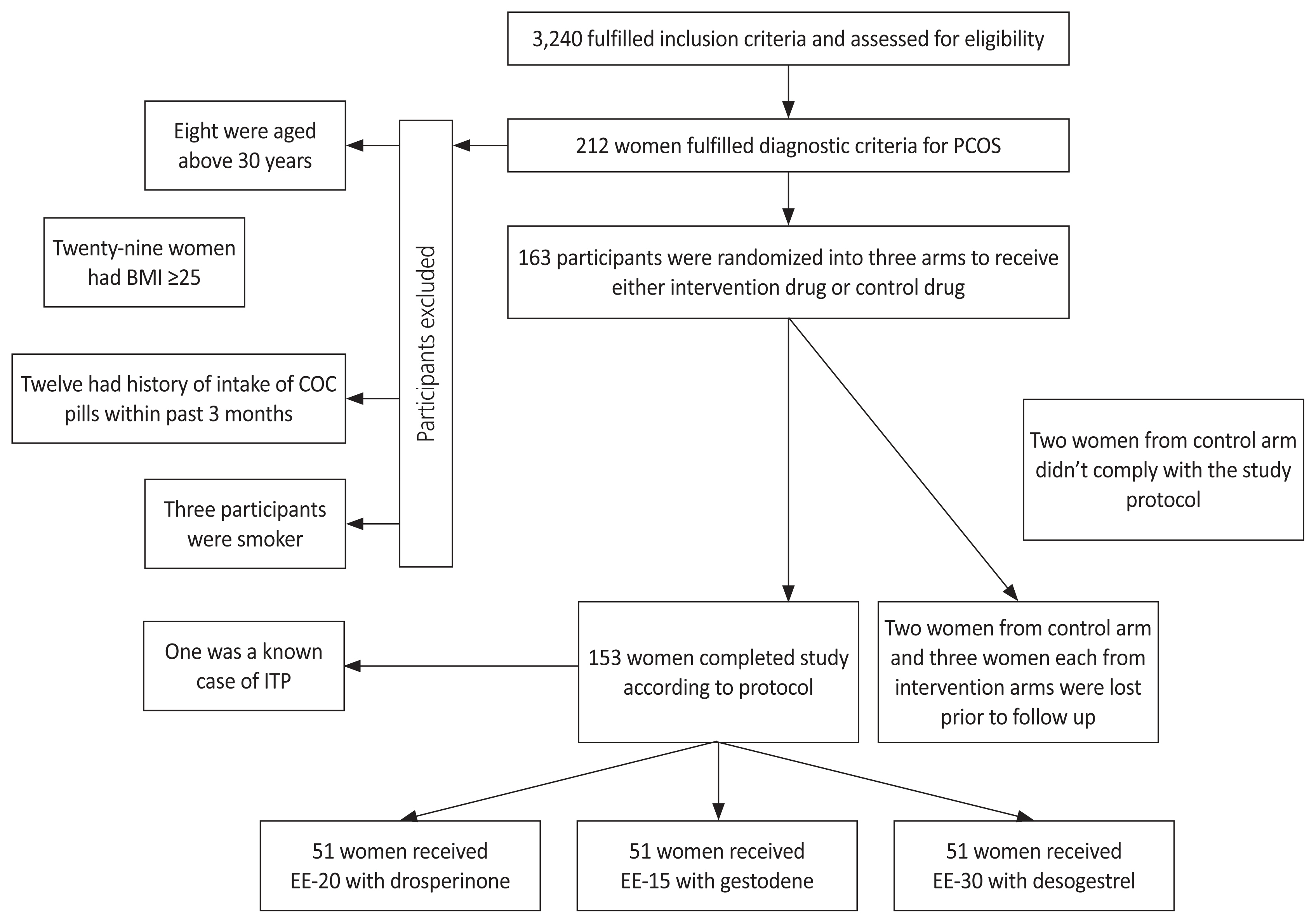
Methods
The present study was a randomized controlled trial to compare prevalence of TC/HDL and LDL discordance among non-obese women with polycystic ovarian syndrome (PCOS) treated with hormonal pills. Women were randomized into three arms, two arms received ultra-low dose pills (Ethinylestradiol [EE] 20 μg with drosperinone 3 mg or EE 15 μg with gestodene 60 μg) and one arm received low dose pill (EE 30 μg with desogestrel 150 μg). The role of baseline participant features and pill composition on discordance was determined.
Results
Discordance was observed in more than a quarter of the participants before intervention. After 1 year of treatment, less than a fifth of the participants were discordant. Ultralow-dose pill users had lower discordance, LDL, and TC than low-dose pill users after 1 year of treatment. The random forest, a non-linear classifier, showed the highest accuracy in predicting discordance. The baseline Parameters with the maximal impact on the occurrence of discordance were triglyceride, homeostatic model assessment for insulin resistance, body mass index, and high density lipoprotein.
Conclusion
Non-obese PCOS women on ultra-low dose pill have a lower risk of acquiring future atherosclerotic cardiovascular disease.
Keyword
Figure
Reference
-
References
1. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018; 110:364–79.
Article2. Roach RE, Helmerhorst FM, Lijfering WM, Stijnen T, Algra A, Dekkers OM. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015; 2015:CD011054.
Article3. de Bastos M, Stegeman BH, Rosendaal FR, Van Hylckama Vlieg A, Helmerhorst FM, Stijnen T, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014; (3):CD010813.
Article4. Halperin IJ, Kumar SS, Stroup DF, Laredo SE. The association between the combined oral contraceptive pill and insulin resistance, dysglycemia and dyslipidemia in women with polycystic ovary syndrome: a systematic review and meta-analysis of observational studies. Hum Reprod. 2011; 26:191–201.
Article5. Amiri M, Ramezani Tehrani F, Nahidi F, Kabir A, Azizi F, Carmina E. Effects of oral contraceptives on metabolic profile in women with polycystic ovary syndrome: a meta-analysis comparing products containing cyproterone acetate with third generation progestins. Metabolism. 2017; 73:22–35.
Article6. Brill K, Then A, Beisiegel U, Jene A, Wünsch C, Leidenberger F. Investigation of the influence of two low-dose monophasic oral contraceptives containing 20 micrograms ethinylestradiol/75 micrograms gestodene and 30 micrograms ethinylestradiol/75 micrograms gestodene, on lipid metabolism in an open randomized trial. Contraception. 1996; 54:291–7.
Article7. Akerlund M, Almström E, Högstedt S, Nabrink M. Oral contraceptive tablets containing 20 and 30 micrograms of ethinyl estradiol with 150 micrograms desogestrel. Their influence on lipids, lipoproteins, sex hormone binding globulin and testosterone. Acta Obstet Gynecol Scand. 1994; 73:136–43.8. Cibula D, Sindelka G, Hill M, Fanta M, Skrha J, Zivny J. Insulin sensitivity in non-obese women with polycystic ovary syndrome during treatment with oral contraceptives containing low-androgenic progestin. Hum Reprod. 2002; 17:76–82.
Article9. Dokras A, Playford M, Kris-Etherton PM, Kunselman AR, Stetter CM, Williams NI, et al. Impact of hormonal contraception and weight loss on high-density lipoprotein cholesterol efflux and lipoprotein particles in women with polycystic ovary syndrome. Clin Endocrinol (Oxf). 2017; 86:739–46.
Article10. Bhattacharya SM, Jha A, DasMukhopadhyay L. Comparison of two contraceptive pills containing drospirenone and 20 μg or 30 μg ethinyl estradiol for polycystic ovary syndrome. Int J Gynaecol Obstet. 2016; 132:210–3.
Article11. Diamanti-Kandarakis E, Papavassiliou AG, Kandarakis SA, Chrousos GP. Pathophysiology and types of dyslipidemia in PCOS. Trends Endocrinol Metab. 2007; 18:280–5.
Article12. Norman RJ, Mahabeer S, Masters S. Ethnic differences in insulin and glucose response to glucose between white and Indian women with polycystic ovary syndrome. Fertil Steril. 1995; 63:58–62.
Article13. Wijeyaratne CN, Balen AH, Barth JH, Belchetz PE. Clinical manifestations and insulin resistance (IR) in polycystic ovary syndrome (PCOS) among South Asians and Caucasians: is there a difference? Clin Endocrinol (Oxf). 2002; 57:343–50.
Article14. Cibula D, Hill M, Fanta M, Sindelka G, Zivny J. Does obesity diminish the positive effect of oral contraceptive treatment on hyperandrogenism in women with polycystic ovarian syndrome? Hum Reprod. 2001; 16:940–4.
Article15. Kim JJ, Chae SJ, Choi YM, Hwang KR, Song SH, Yoon SH, et al. Atherogenic changes in low-density lipoprotein particle profiles were not observed in non-obese women with polycystic ovary syndrome. Hum Reprod. 2013; 28:1354–60.
Article16. Chen MJ, Yang WS, Chen HF, Kuo JJ, Ho HN, Yang YS, et al. Increased follistatin levels after oral contraceptive treatment in obese and non-obese women with polycystic ovary syndrome. Hum Reprod. 2010; 25:779–85.
Article17. Cantey EP, Wilkins JT. Discordance between lipoprotein particle number and cholesterol content: an update. Curr Opin Endocrinol Diabetes Obes. 2018; 25:130–6.
Article18. Conway GS, Agrawal R, Betteridge DJ, Jacobs HS. Risk factors for coronary artery disease in lean and obese women with the polycystic ovary syndrome. Clin Endocrinol (Oxf). 1992; 37:119–25.
Article19. Zhu S, Zhang B, Jiang X, Li Z, Zhao S, Cui L, et al. Metabolic disturbances in non-obese women with polycystic ovary syndrome: a systematic review and meta-analysis. Fertil Steril. 2019; 111:168–77.
Article20. Cook H, Brennan K, Azziz R. Reanalyzing the modified Ferriman-Gallwey score: is there a simpler method for assessing the extent of hirsutism? Fertil Steril. 2011; 96:1266–70.e1.
Article21. Elshazly MB, Quispe R, Michos ED, Sniderman AD, Toth PP, Banach M, et al. Patient-level discordance in population percentiles of the total cholesterol to high-density lipoprotein cholesterol ratio in comparison with low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol: the very large database of lipids study (VLDL-2B). Circulation. 2015; 132:667–76.
Article22. Pencina MJ, D’Agostino RB, Zdrojewski T, Williams K, Thanassoulis G, Furberg CD, et al. Apolipoprotein B improves risk assessment of future coronary heart disease in the Framingham Heart Study beyond LDL-C and non-HDL-C. Eur J Prev Cardiol. 2015; 22:1321–7.
Article23. Wilkins JT, Li RC, Sniderman A, Chan C, Lloyd-Jones DM. Discordance between apolipoprotein B and LDL-cholesterol in young adults predicts coronary artery calcification: the CARDIA study. J Am Coll Cardiol. 2016; 67:193–201.
Article24. Quispe R, Elshazly MB, Zhao D, Toth PP, Puri R, Virani SS, et al. Total cholesterol/HDL-cholesterol ratio discordance with LDL-cholesterol and non-HDL-cholesterol and incidence of atherosclerotic cardiovascular disease in primary prevention: the ARIC study. Eur J Prev Cardiol. 2020; 27:1597–605.
Article25. Sharma M, Khapre M, Saxena V, Kaushal P. Polycystic ovary syndrome among Indian adolescent girls - a systematic review and metanalysis. Nepal J Epidemiol. 2021; 11:1063–75.
Article26. Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in urban and rural India: the ICMR-INDIAB study. PLoS One. 2014; 9:e96808.
Article27. Romualdi D, De Cicco S, Busacca M, Gagliano D, Lanzone A, Guido M. Clinical efficacy and metabolic impact of two different dosages of ethinyl-estradiol in association with drospirenone in normal-weight women with polycystic ovary syndrome: a randomized study. J Endocrinol Invest. 2013; 36:636–41.
Article28. de Medeiros SF. Risks, benefits size and clinical implications of combined oral contraceptive use in women with polycystic ovary syndrome. Reprod Biol Endocrinol. 2017; 15:93.
Article29. Lerchbaum E, Schwetz V, Rabe T, Giuliani A, Obermayer-Pietsch B. Hyperandrogenemia in polycystic ovary syndrome: exploration of the role of free testosterone and androstenedione in metabolic phenotype. PLoS One. 2014; 9:e108263.
Article30. Dumesic DA, Tulberg A, McNamara M, Grogan TR, Abbott DH, Naik R, et al. Serum testosterone to androstenedione ratio predicts metabolic health in normal-weight polycystic ovary syndrome women. J Endocr Soc. 2021; 5:bvab158.
Article31. Tam SP, Archer TK, Deeley RG. Biphasic effects of estrogen on apolipoprotein synthesis in human hepatoma cells: mechanism of antagonism by testosterone. Proc Natl Acad Sci U S A. 1986; 83:3111–5.
Article32. Zhu XD, Bonet B, Knopp RH. 17beta-estradiol, progesterone, and testosterone inversely modulate low-density lipoprotein oxidation and cytotoxicity in cultured placental trophoblast and macrophages. Am J Obstet Gynecol. 1997; 177:196–209.
Article33. Lüdicke F, Gaspard UJ, Demeyer F, Scheen A, Lefebvre P. Randomized controlled study of the influence of two low estrogen dose oral contraceptives containing gestodene or desogestrel on carbohydrate metabolism. Contraception. 2002; 66:411–5.
Article34. Legro RS, Dodson WC, Kris-Etherton PM, Kunselman AR, Stetter CM, Williams NI, et al. Randomized controlled trial of preconception interventions in infertile women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015; 100:4048–58.
Article35. Tikkanen MJ. Estrogens, progestins and lipid metabolism. Maturitas. 1996; 23(Suppl):S51–5.
Article36. Root-Bernstein R, Podufaly A, Dillon PF. Estradiol binds to insulin and insulin receptor decreasing insulin binding in vitro. Front Endocrinol (Lausanne). 2014; 5:118.
Article37. Engmann L, Jin S, Sun F, Legro RS, Polotsky AJ, Hansen KR, et al. Racial and ethnic differences in the polycystic ovary syndrome metabolic phenotype. Am J Obstet Gynecol. 2017; 216:493.e1–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on Calibration of Definition of Drug Resistance for Secondline Antituberculous Drugs
- Antinociceptive effects of intrathecal cimifugin treatment: a preliminary rat study based on formalin test
- Comparison of dexmedetomidine alone with dexmedetomidine and fentanyl during awake fiberoptic intubation in patients with difficult airway: a randomized clinical trial
- Comparative Study of Heavy Metal Blood Serum Level Between Organic and Conventional Farmers in Eastern Taiwan
- A study to evaluate the safety of iodine intake levels in women of childbearing age: 2013–2015 Korea National Health and Nutrition Examination Survey