Obstet Gynecol Sci.
2023 Nov;66(6):562-571. 10.5468/ogs.23071.
Postoperative outcomes of ovarian preserving surgery in premenopausal women with adnexal torsion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Institute of Women’s Life Medical Science, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 4Department of Obstetrics and Gynecology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2547857
- DOI: http://doi.org/10.5468/ogs.23071
Abstract
Objective
We aimed to determine whether ovarian-preserving surgery for adnexal torsion helps preserve ovarian function without increasing the risk of postoperative complications.
Methods
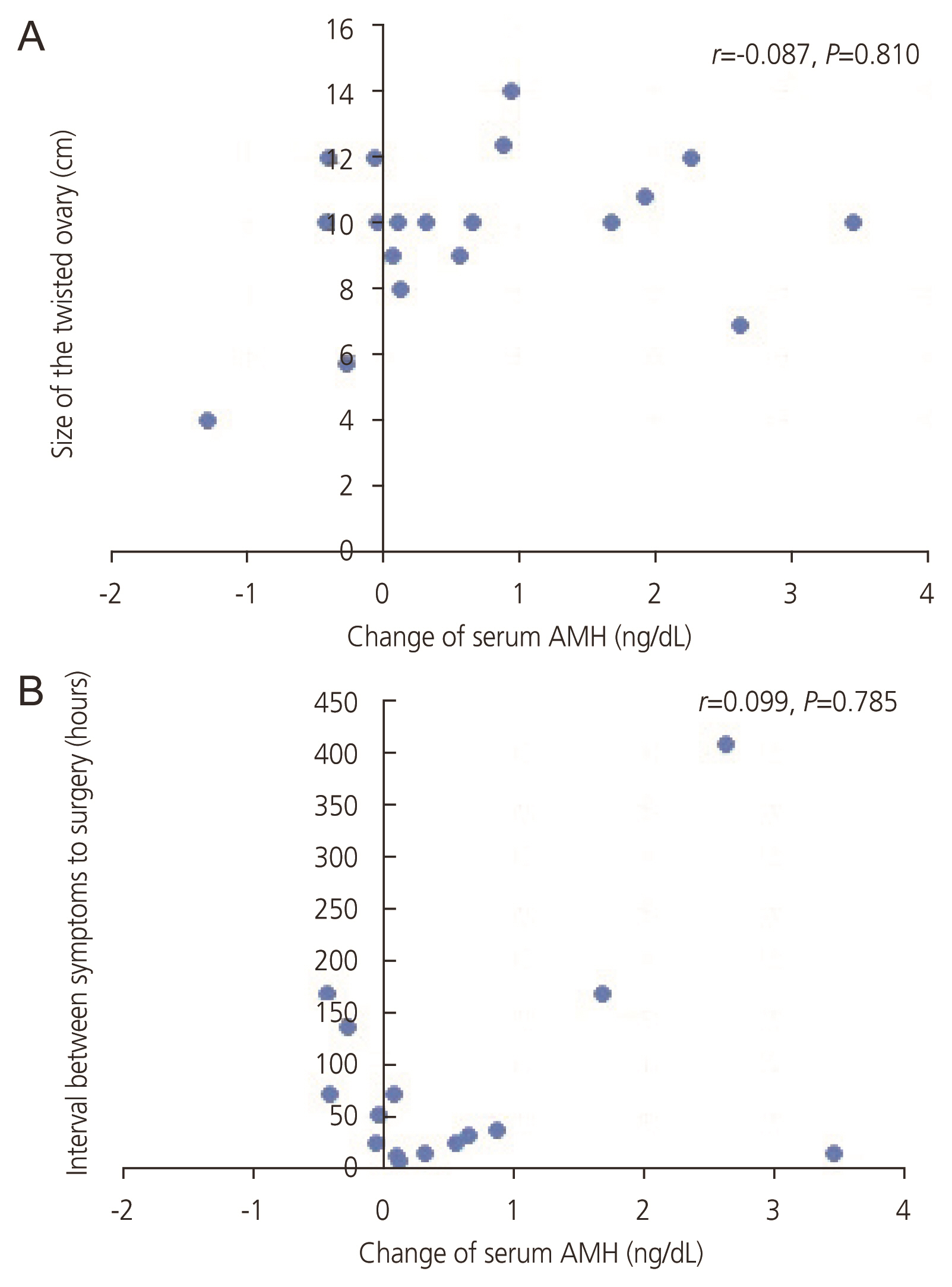
We retrospectively evaluated 71 women who were surgically diagnosed with adnexal torsion between January 2015 and December 2019 at Severance Hospital, Yonsei University College of Medicine (ovarian preservation group, 56; oophorectomy, 15). Serum anti-Müllerian hormone (AMH) levels measured within 6 months before surgery were compared to levels measured 6-24 months after surgery. Surgical findings and postoperative complications were compared between the groups.
Results
There was a borderline significant difference in the decrease in serum AMH levels between the oophorectomy group and ovarian preservation group before and after surgery. There were no significant differences between the groups in terms of fever, infection, or duration of admission. Discoloration of the twisted ovary was found in 27.3% and 33.3% of the patients in the ovarian preservation and oophorectomy groups, respectively. There was no difference in the decrease in serum AMH levels between patients with and those without discoloration.
Conclusion
Ovarian-preserving surgery may not increase postoperative complications in patients with adnexal torsion, even if a twisted mass is suspected to be necrotic. Moreover, the ovarian reserve may not be affected by torsion if the ovary is preserved. Conservative ovarian surgery can be safely performed to preserve the reproductive potential of women with adnexal torsion and cystic masses.
Figure
Reference
-
References
1. Spinelli C, Di Giacomo M, Cei M, Mucci N. Functional ovarian lesions in children and adolescents: when to remove them. Gynecol Endocrinol. 2009; 25:294–8.
Article2. Spinelli C, Di Giacomo M, Mucci N, Massart F. Hemorrhagic corpus luteum cysts: an unusual problem for pediatric surgeons. J Pediatr Adolesc Gynecol. 2009; 22:163–7.
Article3. Lawrence AE, Minneci PC, Deans KJ. Ovarian masses and torsion: new approaches for ovarian salvage. Adv Pediatr. 2020; 67:113–21.4. Huchon C, Fauconnier A. Adnexal torsion: a literature review. Eur J Obstet Gynecol Reprod Biol. 2010; 150:8–12.
Article5. Huang C, Hong MK, Ding DC. A review of ovary torsion. Ci Ji Yi Xue Za Zhi. 2017; 29:143–7.
Article6. Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol. 2006; 49:459–63.
Article7. Göçmen A, Karaca M, Sari A. Conservative laparoscopic approach to adnexal torsion. Arch Gynecol Obstet. 2008; 277:535–8.
Article8. Adnexal torsion in adolescents: ACOG committee opinion no, 783 summary. Obstet Gynecol. 2019; 134:435–6.9. Rey-Bellet Gasser C, Gehri M, Joseph JM, Pauchard JY. Is it ovarian torsion? A systematic literature review and evaluation of prediction signs. Pediatr Emerg Care. 2016; 32:256–61.
Article10. Beaunoyer M, Chapdelaine J, Bouchard S, Ouimet A. Asynchronous bilateral ovarian torsion. J Pediatr Surg. 2004; 39:746–9.
Article11. Galinier P, Carfagna L, Delsol M, Ballouhey Q, Lemasson F, Le Mandat A, et al. Ovarian torsion. Management and ovarian prognosis: a report of 45 cases. J Pediatr Surg. 2009; 44:1759–65.
Article12. Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000–2006. Pediatrics. 2010; 125:532–8.
Article13. McGovern PG, Noah R, Koenigsberg R, Little AB. Adnexal torsion and pulmonary embolism: case report and review of the literature. Obstet Gynecol Surv. 1999; 54:601–8.14. Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Pediatric ovarian malignancy presenting as ovarian torsion: incidence and relevance. J Pediatr Surg. 2010; 45:135–9.
Article15. Savic D, Stankovic ZB, Djukic M, Mikovic Z, Djuricic S. Torsion of malignant ovarian tumors in childhood and adolescence. J Pediatr Endocrinol Metab. 2008; 21:1073–8.
Article16. Templeman C, Hertweck SP, Fallat ME. The clinical course of unresected ovarian torsion. J Pediatr Surg. 2000; 35:1385–7.
Article17. Robertson JJ, Long B, Koyfman A. Myths in the evaluation and management of ovarian torsion. J Emerg Med. 2017; 52:449–56.
Article18. Bergeron LM, Bishop KC, Hoefgen HR, Abraham MS, Tutlam NT, Merritt DF, et al. Surgical management of benign adnexal masses in the pediatric/adolescent population: an 11-year review. J Pediatr Adolesc Gynecol. 2017; 30:123–7.
Article19. Ashwal E, Krissi H, Hiersch L, Less S, Eitan R, Peled Y. Presentation, diagnosis, and treatment of ovarian torsion in premenarchal girls. J Pediatr Adolesc Gynecol. 2015; 28:526–9.
Article20. Lipsett SC, Haines L, Monuteaux MC, Hayes K, Michelson KA. Variation in oophorectomy rates for children with ovarian torsion across US children’s hospitals. J Pediatr. 2021; 231:269–72e1.
Article21. Celik A, Ergün O, Aldemir H, Ozcan C, Ozok G, Erdener A, et al. Long-term results of conservative management of adnexal torsion in children. J Pediatr Surg. 2005; 40:704–8.
Article22. Taskin O, Birincioglu M, Aydin A, Buhur A, Burak F, Yilmaz I, et al. The effects of twisted ischaemic adnexa managed by detorsion on ovarian viability and histology: an ischaemia-reperfusion rodent model. Hum Reprod. 1998; 13:2823–7.
Article23. Sommerville M, Grimes DA, Koonings PP, Campbell K. Ovarian neoplasms and the risk of adnexal torsion. Am J Obstet Gynecol. 1991; 164:577–8.
Article24. Aziz D, Davis V, Allen L, Langer JC. Ovarian torsion in children: is oophorectomy necessary? J Pediatr Surg. 2004; 39:750–3.
Article25. Yasa C, Dural O, Bastu E, Zorlu M, Demir O, Ugurlucan FG. Impact of laparoscopic ovarian detorsion on ovarian reserve. J Obstet Gynaecol Res. 2017; 43:298–302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Premenarchal ovarian torsion
- A retrospective review of pathological outcomes of 129 adnexal torsion cases in pre and post-menopausal women
- Ovarian Torsion in a Postmenopausal Woman: A Case Report and Review of Literature
- Ultrasonography of adnexal causes of acute pelvic pain in pre-menopausal non-pregnant women
- A Clinical Study for Laparoscopic Conservative Therapy of Adnexal Torsion