J Korean Assoc Oral Maxillofac Surg.
2023 Oct;49(5):297-303. 10.5125/jkaoms.2023.49.5.297.
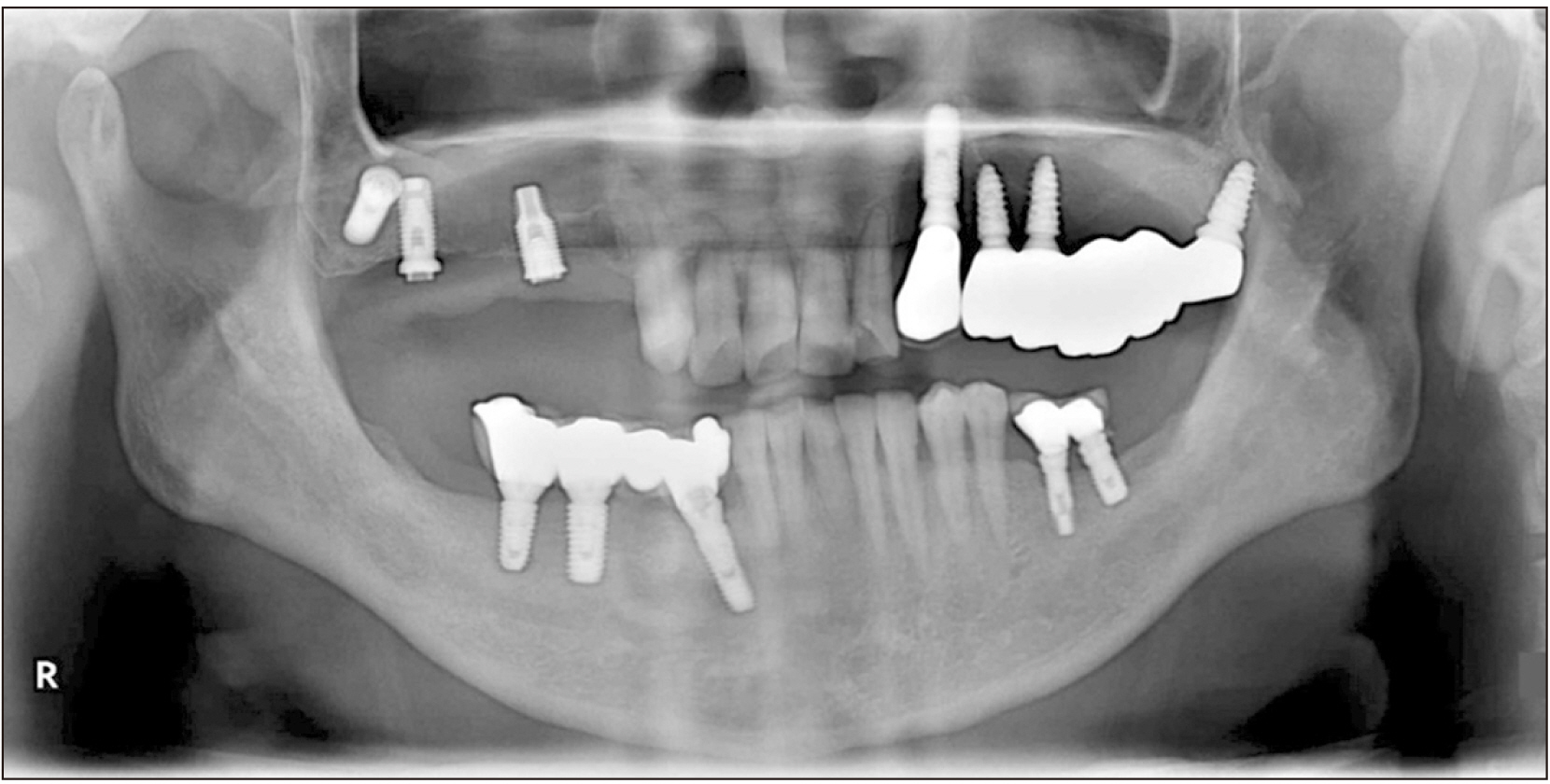
Intra-sinus rigid fixation of a resorbable barrier membrane to repair a large perforation of the sinus membrane: a technical note
- Affiliations
-
- 1Division of Oral and Maxillofacial Surgery, Department of Dentistry, College of Medicine, Hanyang University, Seoul, Korea
- 2Department of Oral and Maxillofacial Surgery, Woori General Hospital, Pocheon, Korea
- 3Department of Oral and Maxillofacial Surgery, The 22nd Century Seoul Dental Hospital, Incheon, Korea
- 4Department of Medicine, Surgery, and Pharmacy, University of Sassari, Sassari, Italy
- KMID: 2547575
- DOI: http://doi.org/10.5125/jkaoms.2023.49.5.297
Abstract
- A resorbable barrier membrane is commonly used for the repair of perforated sinus membranes during sinus lifting surgeries. However, repairing largescale perforations poses challenges for clinicians as the protection and isolation of graft material remain uncertain. With this technique, we aimed to prevent graft material loss and subsequent sinus-related complications using intra-sinus rigid fixation of the resorbable barrier membrane in cases with a large perforation of the sinus membrane.
Figure
Reference
-
References
1. Proussaefs P, Lozada J. 2003; The "Loma Linda pouch": a technique for repairing the perforated sinus membrane. Int J Periodontics Restorative Dent. 23:593–7.2. Proussaefs P, Lozada J, Kim J, Rohrer MD. 2004; Repair of the perforated sinus membrane with a resorbable collagen membrane: a human study. Int J Oral Maxillofac Implants. 19:413–20. PMID: 15214227.3. Hernández-Alfaro F, Torradeflot MM, Marti C. 2008; Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implants Res. 19:91–8. https://doi.org/10.1111/j.1600-0501.2007.01372.x. DOI: 10.1111/j.1600-0501.2007.01372.x. PMID: 17961185.
Article4. Testori T, Wallace SS, Del Fabbro M, Taschieri S, Trisi P, Capelli M, et al. 2008; Repair of large sinus membrane perforations using stabilized collagen barrier membranes: surgical techniques with histologic and radiographic evidence of success. Int J Periodontics Restorative Dent. 28:9–17. PMID: 18351198.5. Pikos MA. 1999; Maxillary sinus membrane repair: report of a technique for large perforations. Implant Dent. 8:29–34. https://doi.org/10.1097/00008505-199901000-00003. DOI: 10.1097/00008505-199901000-00003. PMID: 10356454.
Article6. Schwartz-Arad D, Herzberg R, Dolev E. 2004; The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 75:511–6. https://doi.org/10.1902/jop.2004.75.4.511. DOI: 10.1902/jop.2004.75.4.511. PMID: 15152813.
Article7. Karabuda C, Arisan V, Özyuvaci H. 2006; Effects of sinus membrane perforations on the success of dental implants placed in the augmented sinus. J Periodontol. 77:1991–7. https://doi.org/10.1902/jop.2006.060102. DOI: 10.1902/jop.2006.060102. PMID: 17209783.
Article8. Kim YK, Hwang JW, Yun PY. 2008; Closure of large perforation of sinus membrane using pedicled buccal fat pad graft: a case report. Int J Oral Maxillofac Implants. 23:1139–42.9. Choi BH, Zhu SJ, Jung JH, Lee SH, Huh JY. 2006; The use of autologous fibrin glue for closing sinus membrane perforations during sinus lifts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101:150–4. https://doi.org/10.1016/j.tripleo.2005.04.008. DOI: 10.1016/j.tripleo.2005.04.008. PMID: 16448914.
Article10. Cho YS, Park HK, Park CJ. 2012; Bony window repositioning without using a barrier membrane in the lateral approach for maxillary sinus bone grafts: clinical and radiologic results at 6 months. Int J Oral Maxillofac Implants. 27:211–7. PMID: 22299099.11. Park CJ, Lim JH, Tallarico M, Hwang KG, Choi H, Cho GJ, et al. 2020; Coating of a sand-blasted and acid-etched implant surface with a pH-buffering agent after vacuum-UV photofunctionalization. Coatings. 10:1040. https://doi.org/10.3390/coatings10111040. DOI: 10.3390/coatings10111040.
Article12. Fugazzotto PA, Vlassis J. 2003; A simplified classification and repair system for sinus membrane perforations. J Periodontol. 74:1534–41. https://doi.org/10.1902/jop.2003.74.10.1534. DOI: 10.1902/jop.2003.74.10.1534. PMID: 14653401.
Article13. Le B, Rohrer MD, Prasad HS. 2010; Screw "tent-pole" grafting technique for reconstruction of large vertical alveolar ridge defects using human mineralized allograft for implant site preparation. J Oral Maxillofac Surg. 68:428–35. https://doi.org/10.1016/j.joms.2009.04.059. DOI: 10.1016/j.joms.2009.04.059. PMID: 20116718.
Article14. Petruson B. 2004; Sinuscopy in patients with titanium implants in the nose and sinuses. Scand J Plast Reconstr Surg Hand Surg. 38:86–93. https://doi.org/10.1080/02844310310023909. DOI: 10.1080/02844310310023909. PMID: 15202665.
Article15. Jung JH, Choi BH, Zhu SJ, Lee SH, Huh JY, You TM, et al. 2006; The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 102:602–5. https://doi.org/10.1016/j.tripleo.2005.10.061. DOI: 10.1016/j.tripleo.2005.10.061. PMID: 17052635.
Article16. Block MS, Kaleem A. 2014; Use of sintered xenograft over allograft for ridge augmentation: technique note. J Oral Maxillofac Surg. 72:496–502. https://doi.org/10.1016/j.joms.2013.11.002. DOI: 10.1016/j.joms.2013.11.002. PMID: 24388178.
Article17. Jensen SS, Bosshardt DD, Gruber R, Buser D. 2014; Long-term stability of contour augmentation in the esthetic zone: histologic and histomorphometric evaluation of 12 human biopsies 14 to 80 months after augmentation. J Periodontol. 85:1549–56. https://doi.org/10.1902/jop.2014.140182. DOI: 10.1902/jop.2014.140182. PMID: 25008214.
Article18. Koo TH, Song YW, Cha JK, Jung UW, Kim CS, Lee JS. 2020; Histologic analysis following grafting of damaged extraction sockets using deproteinized bovine or porcine bone mineral: a randomized clinical trial. Clin Oral Implants Res. 31:93–102. https://doi.org/10.1111/clr.13557. DOI: 10.1111/clr.13557. PMID: 31724239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Techniques for Reparation of Perforations of the Maxillary Sinus Membrane: Article Review
- Evaluation of clinical outcomes of implants placed into the maxillary sinus with a perforated sinus membrane: a retrospective study
- Repair of the perforated sinus membrane with a micro-suture technique : Report of cases
- Cyanoacrylate adhesive for closing of sinus membrane perforation during sinus lifts
- Prognosis of closure of large sinus membrane perforations using pedicled buccal fat pads and a resorbable collagen membrane: case series study