Ann Surg Treat Res.
2023 Nov;105(5):264-270. 10.4174/astr.2023.105.5.264.
Observation of changes in quality of life for 5 years after thyroid surgery: an observational cross-sectional study in Korean population
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Surgery, SMG-SNU Boramae Medical Center, Seoul, Korea
- KMID: 2547531
- DOI: http://doi.org/10.4174/astr.2023.105.5.264
Abstract
- Purpose
As thyroid cancer patients are experiencing longer disease-free survival periods, evaluating their quality of life after surgery has become crucial. However, studies on this topic have primarily focused on Western populations, leaving a gap in understanding the Korean patient population’s experiences and needs. This study aims to address this gap and provide insights into the quality of life of thyroid cancer patients in Korea.
Methods
This cross-sectional study evaluated the quality of life of Korean thyroid cancer patients who underwent thyroid lobectomy or total thyroidectomy. Patients were surveyed using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC-QLQ-C30, ver. 3.0) during outpatient clinic visits from January to September 2015. The results were analyzed by comparing them to scores of the general population and based on the time elapsed since surgery. This approach allowed for a comprehensive evaluation of the quality-of-life outcomes in this patient population.
Results
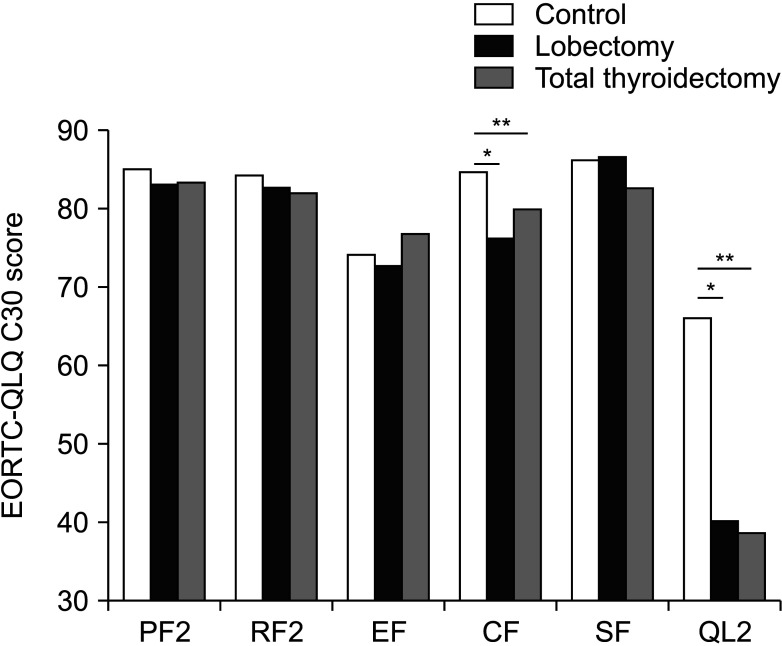
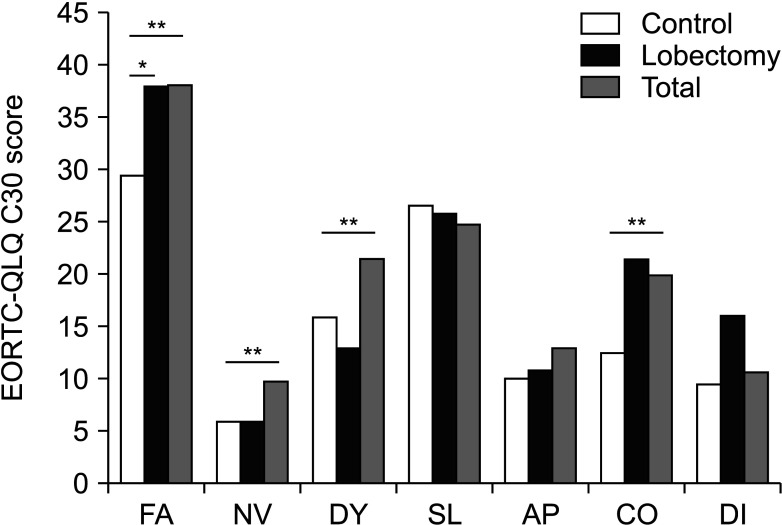
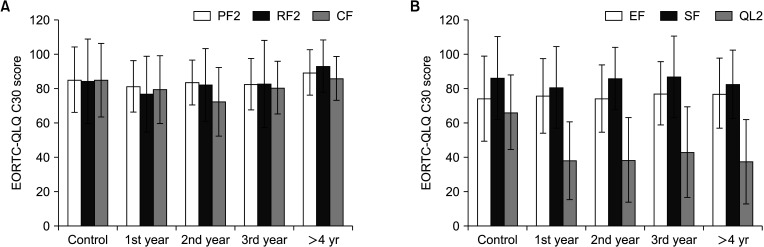
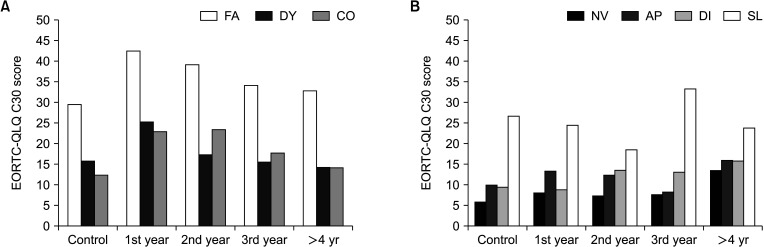
The study found that thyroidectomy had a notable impact on patients’ role and cognitive functions. Patients also experienced worsened symptoms such as fatigue, dyspnea, and constipation, which improved over time and returned to normal levels. However, there were no significant changes in other functions and symptoms after surgery.
Conclusion
The study’s findings showed that thyroidectomy had a relatively minor impact on the functional and symptomatic well-being of patients. Therefore, the results suggest that thyroid surgery may be a safe and effective treatment option for thyroid cancer patients seeking to maintain a good quality of life.
Keyword
Figure
Reference
-
1. The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995; 41:1403–1409. PMID: 8560308.2. Urbach DR. Measuring quality of life after surgery. Surg Innov. 2005; 12:161–165. PMID: 16034507.
Article3. Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005; 23:7428–7436. PMID: 16234510.
Article4. Sprangers MA, Taal BG, Aaronson NK, te Velde A. Quality of life in colorectal cancer: stoma vs. nonstoma patients. Dis Colon Rectum. 1995; 38:361–369. PMID: 7720441.5. Wedding U, Pientka L, Höffken K. Quality-of-life in elderly patients with cancer: a short review. Eur J Cancer. 2007; 43:2203–2210. PMID: 17662595.
Article6. Oerlemans S, Schagen SB, van den Hurk CJ, Husson O, Schoormans D, van de Poll-Franse LV. Self-perceived cognitive functioning and quality of life among cancer survivors: results from the PROFILES registry. J Cancer Surviv. 2022; 16:303–313. PMID: 33728574.
Article7. Husson O, Haak HR, Oranje WA, Mols F, Reemst PH, van de Poll-Franse LV. Health-related quality of life among thyroid cancer survivors: a systematic review. Clin Endocrinol (Oxf). 2011; 75:544–554. PMID: 21615448.
Article8. Applewhite MK, James BC, Kaplan SP, Angelos P, Kaplan EL, Grogan RH, et al. Quality of life in thyroid cancer is similar to that of other cancers with worse survival. World J Surg. 2016; 40:551–561. PMID: 26546191.
Article9. Mongelli MN, Giri S, Peipert BJ, Helenowski IB, Yount SE, Sturgeon C. Financial burden and quality of life among thyroid cancer survivors. Surgery. 2020; 167:631–637. PMID: 31862171.
Article10. Tagay S, Herpertz S, Langkafel M, Erim Y, Bockisch A, Senf W, et al. Health-related quality of life, depression and anxiety in thyroid cancer patients. Qual Life Res. 2006; 15:695–703. PMID: 16688502.
Article11. Büttner M, Hinz A, Singer S, Musholt TJ. Quality of life of patients more than 1 year after surgery for thyroid cancer. Hormones (Athens). 2020; 19:233–243. PMID: 32201929.
Article12. Haraj NE, Bouri H, El Aziz S, Nani S, Habti N, Chadli A. Evaluation of the quality of life in patients followed for differentiated cancer of the thyroid. Ann Endocrinol (Paris). 2019; 80:26–31. PMID: 29571888.
Article13. Nolte S, Liegl G, Petersen MA, Aaronson NK, Costantini A, Fayers PM, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur J Cancer. 2019; 107:153–163. PMID: 30576971.
Article14. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868. PMID: 15129896.
Article15. Mirallié E, Borel F, Tresallet C, Hamy A, Mathonnet M, Lifante JC, et al. Impact of total thyroidectomy on quality of life at 6 months: the prospective ThyrQoL multicentre trial. Eur J Endocrinol. 2020; 182:195–205. PMID: 31804967.
Article16. van Velsen EF, Massolt ET, Heersema H, Kam BL, van Ginhoven TM, Visser WE, et al. Longitudinal analysis of quality of life in patients treated for differentiated thyroid cancer. Eur J Endocr inol. 2019; 181:671–679.
Article17. Lee JI, Kim SH, Tan AH, Kim HK, Jang HW, Hur KY, et al. Decreased health-related quality of life in disease-free survivors of differentiated thyroid cancer in Korea. Health Qual Life Outcomes. 2010; 8:101. PMID: 20840792.
Article18. Hughes DT, Reyes-Gastelum D, Kovatch KJ, Hamilton AS, Ward KC, Haymart MR. Energy level and fatigue after surgery for thyroid cancer: a population-based study of patient-reported outcomes. Surgery. 2020; 167:102–109. PMID: 31582311.
Article19. Husson O, Haak HR, Buffart LM, Nieuwlaat WA, Oranje WA, Mols F, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta Oncol. 2013; 52:249–258. PMID: 23181387.
Article20. Hoftijzer HC, Heemstra KA, Corssmit EP, van der Klaauw AA, Romijn JA, Smit JW. Quality of life in cured patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab. 2008; 93:200–203. PMID: 17956954.
Article21. Yu YR, Fallon SC, Carpenter JL, Athanassaki I, Brandt ML, Wesson DE, et al. Perioperative determinants of transient hypocalcemia after pediatric total thyroidectomy. J Pediatr Surg. 2017; 52:684–688. PMID: 28189449.
Article22. Baldassarre RL, Chang DC, Brumund KT, Bouvet M. Predictors of hypocalcemia after thyroidectomy: results from the nationwide inpatient sample. ISRN Surg. 2012; 2012:838614. PMID: 22844618.
Article23. Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014; 101:307–320. PMID: 24402815.
Article24. Seo ST, Chang JW, Jin J, Lim YC, Rha KS, Koo BS. Transient and permanent hypocalcemia after total thyroidectomy: early predictive factors and long-term follow-up results. Surgery. 2015; 158:1492–1499. PMID: 26144879.
Article25. Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009; 63:624–629. PMID: 19335706.
Article26. Lang BH, Chu KK, Tsang RK, Wong KP, Wong BY. Evaluating the incidence, clinical significance and predictors for vocal cord palsy and incidental laryngopharyngeal conditions before elective thyroidectomy: is there a case for routine laryngoscopic examination? World J Surg. 2014; 38:385–391. PMID: 24065418.
Article27. Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007; 133:481–485. PMID: 17520762.
Article28. Filho JG, Kowalski LP. Postoperative complications of thyroidectomy for differentiated thyroid carcinoma. Am J Otolaryngol. 2004; 25:225–230. PMID: 15239027.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing Quality of Life in Thyroid Cancer Patients with Thyroidectomy
- Alcohol Intake and Risk of Thyroid Cancer: A Meta-Analysis of Observational Studies
- Clinical Factors Associated with Quality of Life in Patients with Thyroid Cancer
- Associations of Illness Symptoms, Perception of Illness, and Coping with Quality of Life of Thyroid Cancer Patients after Thyroidectomy
- Vision of Thyroid Surgery: Past, Present and Future