Ann Surg Treat Res.
2023 Nov;105(5):252-263. 10.4174/astr.2023.105.5.252.
Fluorescence-guided colorectal surgery: applications, clinical results, and protocols
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Division of Colon and Rectal Surgery, Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2547530
- DOI: http://doi.org/10.4174/astr.2023.105.5.252
Abstract
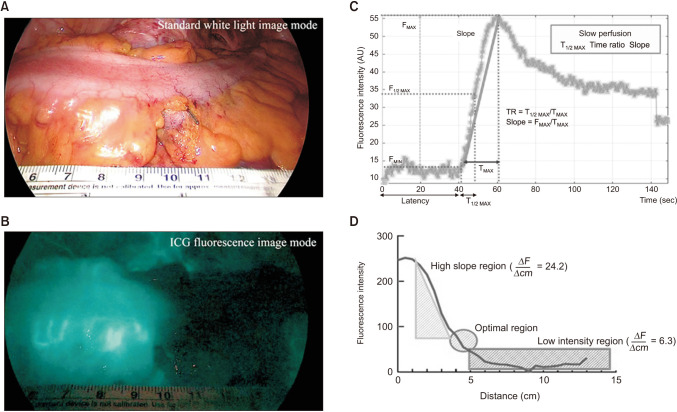
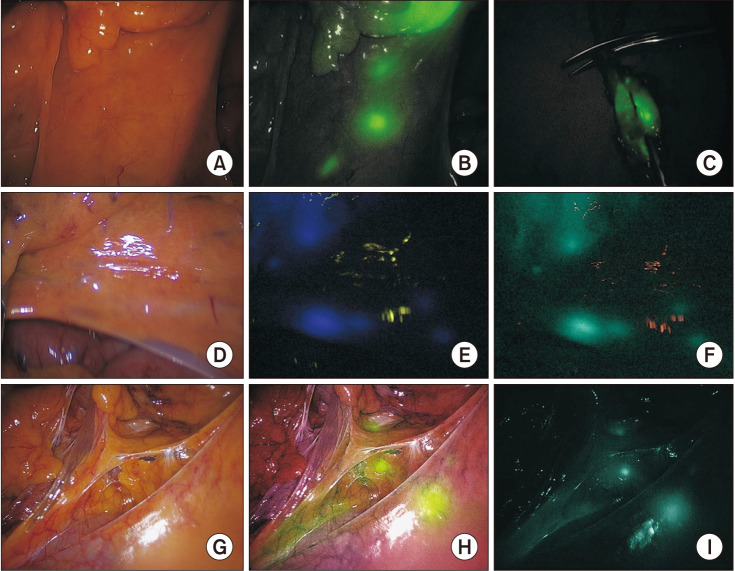
- In recent years, the rise of minimally invasive surgery has driven the development of surgical devices. Indocyanine green (ICG) fluorescence imaging is receiving increased attention in colorectal surgery for improved intraoperative visualization and decision-making. ICG, approved by the U.S. Food and Drug Administration in 1959, rapidly binds to plasma proteins and is primarily intravascular. ICG absorption of near-infrared light (750–800 nm) and emission as fluorescence (830 nm) when bound to tissue proteins enhances deep tissue visualization. Applications include assessing anastomotic perfusion, identifying sentinel lymph nodes, and detecting colorectal cancer metastasis. However, standardized protocols and research on clinical outcomes remain limited. This study explores ICG’s role, advantages, disadvantages, and potential clinical impact in colorectal surgery.
Figure
Reference
-
1. Shah MF, Naeem A, Haq IU, Riaz S, Shakeel O, Panteleimonitis S, et al. Laparoscopy offers bet ter clinical outcomes and long-term survival in patients with right colon cancer: experience from national cancer center. Ann Coloproctol. 2022; 38:223–229. PMID: 34167186.
Article2. Son GM, Kwon MS, Kim Y, Kim J, Kim SH, Lee JW. Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc. 2019; 33:1640–1649. PMID: 30203201.
Article3. Cahill RA, Ris F, Mortensen NJ. Near-infrared laparoscopy for real-time intra-operative arterial and lymphatic perfusion imaging. Colorectal Dis. 2011; 13 Suppl 7:12–17. PMID: 22098511.
Article4. Piozzi GN, Kim SH. Robotic intersphincteric resection for low rectal cancer: technical controversies and a systematic review on the perioperative, oncological, and functional outcomes. Ann Coloproctol. 2021; 37:351–367. PMID: 34784706.
Article5. Ryu HS, Kim J. Current status and role of robotic approach in patients with low-lying rectal cancer. Ann Surg Treat Res. 2022; 103:1–11. PMID: 35919115.
Article6. Cahill RA, Anderson M, Wang LM, Lindsey I, Cunningham C, Mortensen NJ. Near-infrared (NIR) laparoscopy for intraoperative lymphatic road-mapping and sentinel node identification during definitive surgical resection of early-stage colorectal neoplasia. Surg Endosc. 2012; 26:197–204. PMID: 21853392.
Article7. Son GM, Ahn HM, Lee IY, Ha GW. Multifunctional indocyanine green applications for fluorescence-guided laparoscopic colorectal surgery. Ann Coloproctol. 2021; 37:133–140. PMID: 34102813.
Article8. Ahn HM, Son GM, Lee IY, Park SH, Kim NS, Baek KR. Optimization of indocyanine green angiography for colon perfusion during laparoscopic colorectal surgery. Colorectal Dis. 2021; 23:1848–1859. PMID: 33894016.
Article9. Boni L, Fingerhut A, Marzorati A, Rausei S, Dionigi G, Cassinotti E. Indocyanine green fluorescence angiography during laparoscopic low anterior resection: results of a case-matched study. Surg Endosc. 2017; 31:1836–1840. PMID: 27553790.
Article10. Kim S, Kang SI, Kim SH, Kim JH. The effect of anastomotic leakage on the incidence and severity of low anterior resection syndrome in patients undergoing proctectomy: a propensity score matching analysis. Ann Coloproctol. 2021; 37:281–290. PMID: 34098631.
Article11. Koedam TW, Bootsma BT, Deijen CL, van de Brug T, Kazemier G, Cuesta MA, et al. Oncological outcomes after anastomotic leakage after surgery for colon or rectal cancer: increased risk of local recurrence. Ann Surg. 2022; 275:e420–e427. PMID: 32224742.12. Chaouch MA, Kellil T, Jeddi C, Saidani A, Chebbi F, Zouari K. How to prevent anastomotic leak in colorectal surgery?: a systematic review. Ann Coloproctol. 2020; 36:213–222. PMID: 32919437.
Article13. Mizuuchi Y, Tanabe Y, Sada M, Tamura K, Nagayoshi K, Nagai S, et al. Cross-sectional area of psoas muscle as a predictive marker of anastomotic failure in male rectal cancer patients: Japanese single institutional retrospective observational study. Ann Coloproctol. 2022; 38:353–361. PMID: 35410111.
Article14. Oh BY, Park YA, Huh JW, Cho YB, Yun SH, Kim HC, et al. Neoadjuvant chemoradiotherapy determines the prognostic impact of anastomotic leakage in advanced rectal cancer. Ann Surg Treat Res. 2022; 103:235–243. PMID: 36304190.
Article15. Degiuli M, Elmore U, De Luca R, De Nardi P, Tomatis M, Biondi A, et al. Risk factors for anastomotic leakage after anterior resection for rectal cancer (RALAR study): a nationwide retrospective study of the Italian Society of Surgical Oncology Colorectal Cancer Network Collaborative Group. Colorectal Dis. 2022; 24:264–276. PMID: 34816571.
Article16. Varela C, Nassr M, Razak A, Kim NK. Double-layered hand-sewn anastomosis: a valuable resource for the colorectal surgeon. Ann Coloproctol. 2022; 38:271–275. PMID: 35295072.
Article17. Crafa F, Striano A, Esposito F, Rossetti AR, Baiamonte M, Gianfreda V, et al. The “reverse air leak test”: a new technique for the assessment of low colorectal anastomosis. Ann Coloproctol. 2022; 38:20–27. PMID: 33332954.
Article18. Benčurik V, Škrovina M, Martínek L, Bartoš J, Macháčková M, Dosoudil M, et al. Intraoperative fluorescence angiography and risk factors of anastomotic leakage in mini-invasive low rectal resections. Surg Endosc. 2021; 35:5015–5023. PMID: 32970211.
Article19. Alekseev M, Rybakov E, Khomyakov E, Zarodnyuk I, Shelygin Y. Intraoperative fluorescence angiography as an independent factor of anastomotic leakage and a nomogram for predicting leak for colorectal anastomoses. Ann Coloproctol. 2022; 38:380–386. PMID: 34289650.
Article20. Dinallo AM, Kolarsick P, Boyan WP, Protyniak B, James A, Dressner RM, et al. Does routine use of indocyanine green fluorescence angiography prevent anastomotic leaks?: a retrospective cohort analysis. Am J Surg. 2019; 218:136–139. PMID: 30360896.
Article21. Renna MS, Grzeda MT, Bailey J, Hainsworth A, Ourselin S, Ebner M, et al. Intraoperative bowel perfusion assessment methods and their effects on anastomotic leak rates: meta-analysis. Br J Surg. 2023; 110:1131–1142. PMID: 37253021.
Article22. Emile SH, Khan SM, Wexner SD. Impact of change in the surgical plan based on indocyanine green fluorescence angiography on the rates of colorectal anastomotic leak: a systematic review and meta-analysis. Surg Endosc. 2022; 36:2245–2257. PMID: 35024926.
Article23. Trastulli S, Munzi G, Desiderio J, Cirocchi R, Rossi M, Parisi A. Indocyanine green fluorescence angiography versus standard intraoperative methods for prevention of anastomotic leak in colorectal surgery: meta-analysis. Br J Surg. 2021; 108:359–372. PMID: 33778848.
Article24. De Nardi P, Elmore U, Maggi G, Maggiore R, Boni L, Cassinotti E, et al. Intraoperative angiography with indocyanine green to assess anastomosis perfusion in patients undergoing laparoscopic colorectal resection: results of a multicenter randomized controlled trial. Surg Endosc. 2020; 34:53–60. PMID: 30903276.
Article25. Alekseev M, Rybakov E, Shelygin Y, Chernyshov S, Zarodnyuk I. A study investigating the perfusion of colorectal anastomoses using fluorescence angiography: results of the FLAG randomized trial. Colorectal Dis. 2020; 22:1147–1153. PMID: 32189424.
Article26. Jafari MD, Pigazzi A, McLemore EC, Mutch MG, Haas E, Rasheid SH, et al. Perfusion Assessment in Left-Sided/Low Anterior Resection (PILLAR III): a randomized, controlled, parallel, multicenter study assessing perfusion outcomes with PINPOINT near-infrared fluorescence imaging in low anterior resection. Dis Colon Rectum. 2021; 64:995–1002. PMID: 33872284.
Article27. De Robles MS, Young CJ. Triple-staple technique effectively reduces operating time for rectal anastomosis. Ann Coloproctol. 2021; 37:16–20. PMID: 32054240.
Article28. Tebala GD, Mingoli A, Natili A, Khan AQ, Brachini G. Surgical risk and pathological results of emergency resection in the treatment of acutely obstructing colorectal cancers: a retrospective cohort study. Ann Coloproctol. 2021; 37:21–28. PMID: 32178504.
Article29. Meijer RP, Faber RA, Bijlstra OD, Braak JP, Meershoek-Klein Kranenbarg E, Putter H, et al. AVOID; a phase III, randomised controlled trial using indocyanine green for the prevention of anastomotic leakage in colorectal surgery. BMJ Open. 2022; 12:e051144.
Article30. Iguchi K, Watanabe J, Suwa Y, Chida K, Atsumi Y, Numata M, et al. The usefulness of indocyanine green fluorescence imaging for intestinal perfusion assessment of intracorporeal anastomosis in laparoscopic colon cancer surgery. Int J Colorectal Dis. 2023; 38:7. PMID: 36625972.
Article31. Rottoli M, Tanzanu M, Lanci AL, Gentilini L, Boschi L, Poggioli G. Mesenteric lengthening during pouch surgery: technique and outcomes in a tertiary centre. Updates Surg. 2021; 73:581–586. PMID: 33492620.
Article32. Freund MR, Kent I, Agarwal S, Wexner SD. Use of indocyanine green fluorescence angiography during ileal J-pouch surgery requiring lengthening maneuvers. Tech Coloproctol. 2022; 26:181–186. PMID: 35091791.
Article33. Hardy NP, Dalli J, Khan MF, Andrejevic P, Neary PM, Cahill RA. Inter-user variation in the interpretation of near infrared perfusion imaging using indocyanine green in colorectal surgery. Surg Endosc. 2021; 35:7074–7081. PMID: 33398567.
Article34. Faber RA, Tange FP, Galema HA, Zwaan TC, Holman FA, Peeters KC, et al. Quantification of indocyanine green near-infrared fluorescence bowel perfusion assessment in colorectal surgery. Surg Endosc. 2023; 37:6824–6833. PMID: 37286750.
Article35. Soares AS, Bano S, Clancy NT, Stoyanov D, Lovat LB, Chand M. Multisensor perfusion assessment cohort study: Preliminary evidence toward a standardized assessment of indocyanine green fluorescence in colorectal surgery. Surgery. 2022; 172:69–73. PMID: 35168814.
Article36. Skrovina M, Bencurik V, Martinek L, Machackova M, Bartos J, Andel P, et al. The significance of intraoperative fluorescence angiography in miniinvasive low rectal resections. Wideochir Inne Tech Maloinwazyjne. 2020; 15:43–48. PMID: 32117485.
Article37. Yanagita T, Hara M, Osaga S, Nakai N, Maeda Y, Shiga K, et al. Efficacy of intraoperative ICG fluorescence imaging evaluation for preventing anastomotic leakage after left-sided colon or rectal cancer surgery: a propensity score-matched analysis. Surg Endosc. 2021; 35:2373–2385. PMID: 33495878.
Article38. Castagneto-Gissey L, Iodice A, Urciuoli P, Pontone S, Salvati B, Casella G. Novel modality of endoluminal anastomotic integrity assessment with fluoroangiography after left-sided colorectal resections. World J Surg. 2023; 47:1303–1309. PMID: 36694037.
Article39. Lauricella S, Peyser D, Carrano FM, Sylla P. Intraluminal anastomotic assessment using indocyanine green near-infrared imaging for left-sided colonic and rectal resections: a systematic review. J Gastrointest Surg. 2023; 27:615–625. PMID: 36604377.
Article40. Chand M, Keller DS, Joshi HM, Devoto L, Rodriguez-Justo M, Cohen R. Feasibility of fluorescence lymph node imaging in colon cancer: FLICC. Tech Coloproctol. 2018; 22:271–277. PMID: 29551004.
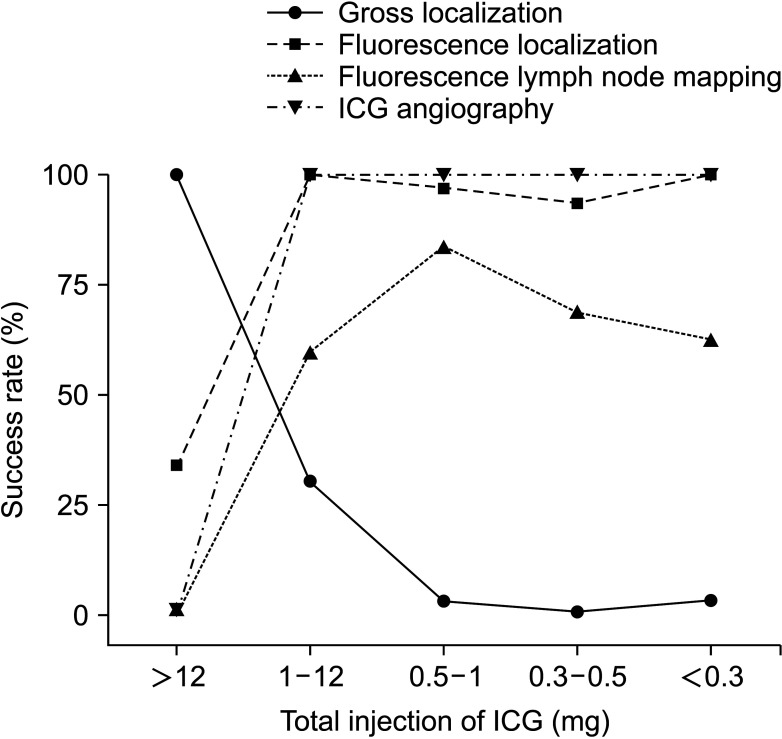
Article41. Ahn HM, Son GM, Lee IY, Shin DH, Kim TK, Park SB, et al. Optimal ICG dosage of preoperative colonoscopic tattooing for fluorescence-guided laparoscopic colorectal surgery. Surg Endosc. 2022; 36:1152–1163. PMID: 33638107.
Article42. Ribero D, Mento F, Sega V, Lo Conte D, Mellano A, Spinoglio G. ICG-guided lymphadenectomy during surgery for colon and rectal cancer-interim analysis of the GREENLIGHT Trial. Biomedicines. 2022; 10:541. PMID: 35327344.
Article43. Wan J, Wang S, Yan B, Tang Y, Zheng J, Ji H, et al. Indocyanine green for radical lymph node dissection in patients with sigmoid and rectal cancer: randomized clinical trial. BJS Open. 2022; 6:zrac151. PMID: 36515673.
Article44. Ho MF, Futaba K, Mak TW, Ng SS. Personalized laparoscopic resection of colon cancer with the use of indocyanine green lymph node mapping: technical and clinical outcomes. Asian J Endosc Surg. 2022; 15:563–568. PMID: 35261162.
Article45. Ushijima H, Kawamura J, Ueda K, Yane Y, Yoshioka Y, Daito K, et al. Visualization of lymphatic flow in laparoscopic colon cancer surgery using indocyanine green fluorescence imaging. Sci Rep. 2020; 10:14274. PMID: 32868829.
Article46. Kinoshita H, Kawada K, Itatani Y, Okamura R, Oshima N, Okada T, et al. Timing of real-time indocyanine green fluorescence visualization for lymph node dissection during laparoscopic colon cancer surgery. Langenbecks Arch Surg. 2023; 408:38. PMID: 36650252.
Article47. Lucas K, Melling N, Giannou AD, Reeh M, Mann O, Hackert T, et al. Lymphatic mapping in colon cancer depending on injection time and tracing agent: a systematic review and meta-analysis of prospective designed studies. Cancers (Basel). 2023; 15:3196. PMID: 37370806.
Article48. Ankersmit M, Bonjer HJ, Hannink G, Schoonmade LJ, van der Pas MH, Meijerink WJ. Near-infrared fluorescence imaging for sentinel lymph node identification in colon cancer: a prospective single-center study and systematic review with meta-analysis. Tech Coloproctol. 2019; 23:1113–1126. PMID: 31741099.
Article49. Villegas-Tovar E, Jimenez-Lillo J, Jimenez-Valerio V, Diaz-Giron-Gidi A, Faes-Petersen R, Otero-Piñeiro A, et al. Performance of Indocyanine green for sentinel lymph node mapping and lymph node metastasis in colorectal cancer: a diagnostic test accuracy meta-analysis. Surg Endosc. 2020; 34:1035–1047. PMID: 31754853.
Article50. Burghgraef TA, Zweep AL, Sikkenk DJ, van der Pas MH, Verheijen PM, Consten EC. In vivo sentinel lymph node identification using fluorescent tracer imaging in colon cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2021; 158:103149. PMID: 33450679.
Article51. Kim MC, Oh JH. Lateral pelvic lymph node dissection after neoadjuvant chemoradiotherapy in patients with rectal cancer: a single-center experience and literature review. Ann Coloproctol. 2021; 37:382–394. PMID: 34961302.
Article52. Mahendran B, Balasubramanya S, Sebastiani S, Smolarek S. Extended lymphadenectomy in locally advanced rectal cancers: a systematic review. Ann Coloproctol. 2022; 38:3–12. PMID: 34788526.
Article53. Ogura A, Konishi T, Cunningham C, Garcia-Aguilar J, Iversen H, Toda S, et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol. 2019; 37:33–43. PMID: 30403572.
Article54. Lim BL, Park IJ, Kim YI, Kim CW, Lee JL, Yoon YS, et al. Difference in prognostic impact of lateral pelvic lymph node metastasis between pre- and post-neoadjuvant chemoradiotherapy in rectal cancer patients. Ann Surg Treat Res. 2023; 104:205–213. PMID: 37051159.
Article55. Zhou SC, Tian YT, Wang XW, Zhao CD, Ma S, Jiang J, et al. Application of indocyanine green-enhanced near-infrared fluorescence-guided imaging in laparoscopic lateral pelvic lymph node dissection for middle-low rectal cancer. World J Gastroenterol. 2019; 25:4502–4511. PMID: 31496628.
Article56. Dai JY, Han ZJ, Wang JD, Liu BS, Liu JY, Wang YC. Short-term outcomes of near-infrared imaging using indocyanine green in laparoscopic lateral pelvic lymph node dissection for middle-lower rectal cancer: a propensity score-matched cohort analysis. Front Med (Lausanne). 2022; 9:1039928. PMID: 36438036.
Article57. Kim HJ, Choi GS, Park JS, Park SY, Cho SH, Seo AN, et al. S122: impact of fluorescence and 3D images to completeness of lateral pelvic node dissection. Surg Endosc. 2020; 34:469–476. PMID: 31139999.
Article58. Watanabe J, Ohya H, Sakai J, Suwa Y, Goto K, Nakagawa K, et al. Long-term outcomes of indocyanine green fluorescence imaging-guided laparoscopic lateral pelvic lymph node dissection for clinical stage II/III middle-lower rectal cancer: a propensity score-matched cohort study. Tech Coloproctol. 2023; 27:759–767. PMID: 36773172.
Article59. Su H, Xu Z, Bao M, Luo S, Liang J, Pei W, et al. Lateral pelvic sentinel lymph node biopsy using indocyanine green fluorescence navigation: can it be a powerful supplement tool for predicting the status of lateral pelvic lymph nodes in advanced lower rectal cancer. Surg Endosc. 2023; 37:4088–4096. PMID: 36997652.
Article60. Yasui M, Ohue M, Noura S, Miyoshi N, Takahashi Y, Matsuda C, et al. Exploratory analysis of lateral pelvic sentinel lymph node status for optimal management of laparoscopic lateral lymph node dissection in advanced lower rectal cancer without suspected lateral lymph node metastasis. BMC Cancer. 2021; 21:911. PMID: 34380428.
Article61. Satou S, Ishizawa T, Masuda K, Kaneko J, Aoki T, Sakamoto Y, et al. Indocyanine green fluorescent imaging for detecting extrahepatic metastasis of hepatocellular carcinoma. J Gastroenterol. 2013; 48:1136–1143. PMID: 23179608.
Article62. Barabino G, Klein JP, Porcheron J, Grichine A, Coll JL, Cottier M. Intraoperative near-infrared fluorescence imaging using indocyanine green in colorectal carcinomatosis surgery: proof of concept. Eur J Surg Oncol. 2016; 42:1931–1937. PMID: 27378159.
Article63. Liberale G, Vankerckhove S, Caldon MG, Ahmed B, Moreau M, Nakadi IE, et al. Fluorescence imaging after indocyanine green injection for detection of peritoneal metastases in patients undergoing cytoreductive surgery for peritoneal carcinomatosis from colorectal cancer: a pilot study. Ann Surg. 2016; 264:1110–1115. PMID: 27828822.
Article64. Maeda H, Wu J, Sawa T, Matsumura Y, Hori K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release. 2000; 65:271–284. PMID: 10699287.
Article65. Maeda H. The link between infection and cancer: tumor vasculature, free radicals, and drug delivery to tumors via the EPR effect. Cancer Sci. 2013; 104:779–789. PMID: 23495730.
Article66. Liberale G, Bourgeois P, Larsimont D, Moreau M, Donckier V, Ishizawa T. Indocyanine green fluorescence-guided surgery after IV injection in metastatic colorectal cancer: a systematic review. Eur J Surg Oncol. 2017; 43:1656–1667. PMID: 28579357.
Article67. Kim YJ, Kim CH. Treatment for peritoneal metastasis of patients with colorectal cancer. Ann Coloproctol. 2021; 37:425–433. PMID: 34961304.
Article68. Lieto E, Auricchio A, Cardella F, Mabilia A, Basile N, Castellano P, et al. Fluorescence-guided surgery in the combined treatment of peritoneal carcinomatosis from colorectal cancer: preliminary results and considerations. World J Surg. 2018; 42:1154–1160. PMID: 28929277.
Article69. González-Abós C, Selva AB, de Lacy FB, Valverde S, A lmenara R, Lacy AM. Quantitative indocyanine green fluorescence imaging assessment for nonmucinous peritoneal metastases: preliminary results of the ICCP Study. Dis Colon Rectum. 2022; 65:314–321. PMID: 34775406.
Article70. Baiocchi GL, Gheza F, Molfino S, Arru L, Vaira M, Giacopuzzi S. Indocyanine green fluorescence-guided intraoperative detection of peritoneal carcinomatosis: systematic review. BMC Surg. 2020; 20:158. PMID: 32680492.
Article71. Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg. 2006; 141:460–467. PMID: 16702517.72. Park SH, Shin JK, Lee WY, Yun SH, Cho YB, Huh JW, et al. Clinical outcomes of neoadjuvant chemotherapy in colorectal cancer patients with synchronous resectable liver metastasis: a propensity score matching analysis. Ann Coloproctol. 2021; 37:244–252. PMID: 34182620.
Article73. Liu W, Zhang ZY, Yin SS, Yan K, Xing BC. Contrast-enhanced intraoperative ultrasound improved sensitivity and positive predictive value in colorectal liver metastasis: a systematic review and meta-analysis. Ann Surg Oncol. 2021; 28:3763–3773. PMID: 33247361.
Article74. Peloso A, Franchi E, Canepa MC, Barbieri L, Briani L, Ferrario J, et al. Combined use of intraoperative ultrasound and indocyanine green fluorescence imaging to detect liver metastases from colorectal cancer. HPB (Oxford). 2013; 15:928–934. PMID: 23458105.
Article75. He K, Hong X, Chi C, Cai C, An Y, Li P, et al. Efficacy of near-infrared fluorescence-guided hepatectomy for the detection of colorectal liver metastases: a randomized controlled trial. J Am Coll Surg. 2022; 234:130–137. PMID: 35213433.
Article76. ASGE Technology Committee. Kethu SR, Banerjee S, Desilets D, Diehl DL, Farraye FA, et al. Endoscopic tattooing. Gastrointest Endosc. 2010; 72:681–685. PMID: 20883844.
Article77. Miyoshi N, Ohue M, Noura S, Yano M, Sasaki Y, Kishi K, et al. Surgical usefulness of indocyanine green as an alternative to India ink for endoscopic marking. Surg Endosc. 2009; 23:347–351. PMID: 18443867.
Article78. Watanabe M, Tsunoda A, Narita K, Kusano M, Miwa M. Colonic tattooing using fluorescence imaging with light-emitting diode-activated indocyanine green: a feasibility study. Surg Today. 2009; 39:214–218. PMID: 19280280.
Article79. Konstantinidis MK, Ioannidis A, Vassiliu P, Arkadopoulos N, Papanikolaou IS, Stavridis K, et al. Preoperative tumor marking with indocyanine green (ICG) prior to minimally invasive colorectal cancer: a systematic review of current literature. Front Surg. 2023; 10:1258343. PMID: 37638121.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multifunctional Indocyanine Green Applications for Fluorescence-Guided Laparoscopic Colorectal Surgery
- Indocyanine Green-Guided Video-Assisted Thoracoscopic Surgery for Resection of an Ectopic Mediastinal Parathyroid Adenoma
- 5-Aminolevulinic Acid Fluorescence Discriminates the Histological Grade of Extraventricular Neurocytoma
- Fluorescence Guided Surgery with 5-Aminolevulinic Acid for Resection of Spinal Cord Ependymomas
- Educational Benefits of Intraoperative Indocyanine Green Angiography for Surgical Beginners During Laparoscopic Colorectal Surgery