J Korean Neurosurg Soc.
2023 Nov;66(6):681-689. 10.3340/jkns.2023.0157.
Neutrophil to Lymphocyte Ratio and Serum Biomarkers : A Potential Tool for Prediction of Clinically Relevant Cerebral Vasospasm after Aneurysmal Subarachnoid Hemorrhage
- Affiliations
-
- 1Department of Radiology, Trakya University Faculty of Medicine, Edirne, Turkey
- 2Department of Neurosurgery, Edirne Sultan 1.Murat State Hospital, Edirne, Turkey
- 3Department of Electroneurophysiology, Trakya University of Health Services Vocational College, Edirne, Turkey
- 4Department of Neurosurgery, Trakya University Faculty of Medicine, Edirne, Turkey
- 5Department of Bioistatistics, Trakya University Faculty of Medicine, Edirne, Turkey
- KMID: 2547462
- DOI: http://doi.org/10.3340/jkns.2023.0157
Abstract
Objective
: Subarachnoid hemorrhage (SAH) is a condition characterized by bleeding in the subarachnoid space, often resulting from the rupture of a cerebral aneurysm. Delayed cerebral ischemia caused by vasospasm is a significant cause of mortality and morbidity in SAH patients, and inflammatory markers such as systemic inflammatory response index (SIRI), systemic inflammatory index (SII), neutrophil-to-lymphocyte ratio (NLR), and derived NLR (dNLR) have shown potential in predicting clinical vasospasm and outcomes in SAH patients. This article aims to investigate the relationship between inflammatory markers and cerebral vasospasm after aneurysmatic SAH (aSAH) and evaluate the predictive value of various indices, including SIRI, SII, NLR, and dNLR, in predicting clinical vasospasm.
Methods
: A retrospective analysis was performed on a cohort of 96 patients who met the inclusion criteria out of a total of 139 patients admitted Trakya University Hospital with a confirmed diagnosis of aSAH between January 2013 and December 2021. Diagnostic procedures, neurological examinations, and laboratory tests were performed to assess the patients' condition. The Student’s t-test compared age variables, while the chi-square test compared categorical variables between the non-vasospasm (NVS) and vasospasm (VS) groups. Receiver operating characteristic (ROC) curve analyses were used to evaluate the diagnostic accuracy of laboratory parameters, calculating the area under the ROC curve, cut-off values, sensitivity, and specificity. A significance level of p<0.05 was considered statistically significant.
Results
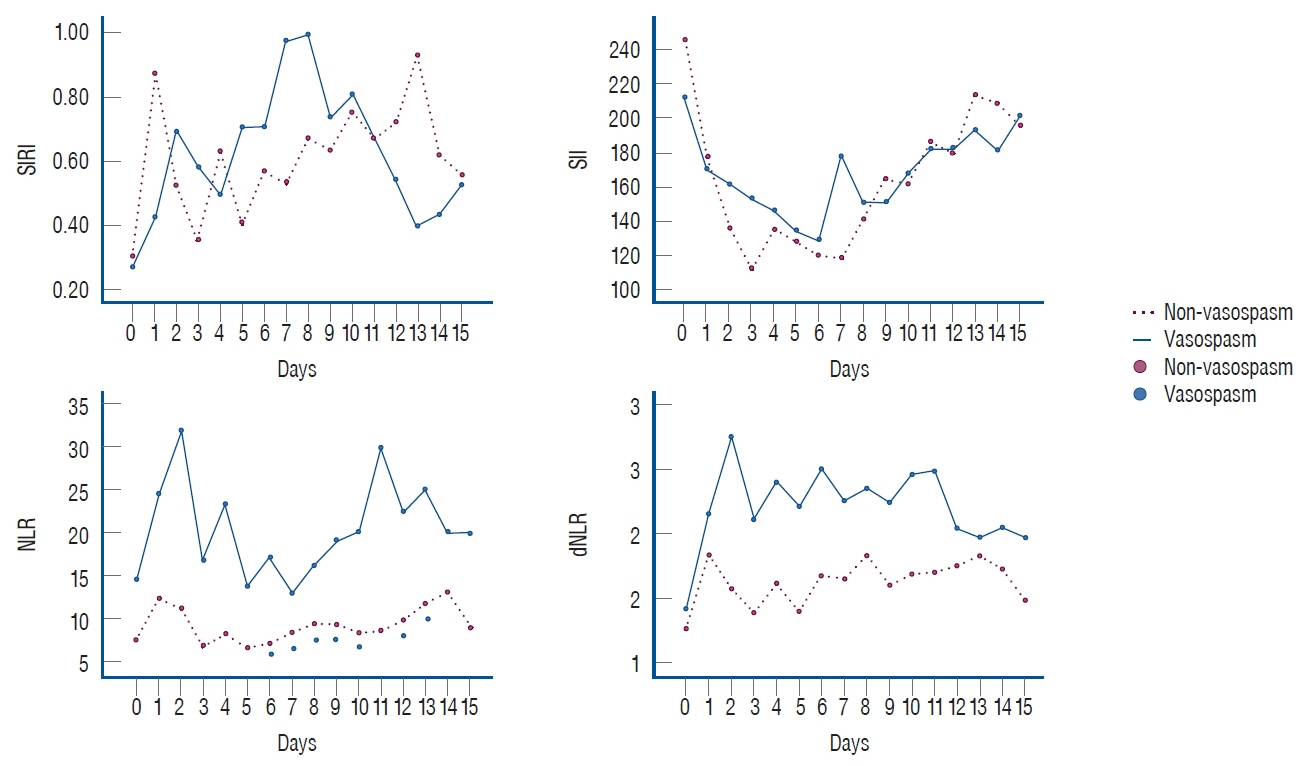
: The study included 96 patients divided into two groups : NVS and VS. Various laboratory parameters, such as NLR, SII, and dNLR, were measured daily for 15 days, and statistically significant differences were found in NLR on 7 days, with specific cut-off values identified for each day. SII showed a significant difference on day 9, while dNLR had significant differences on days 2, 4, and 9. Graphs depicting the values of these markers for each day are provided.
Conclusion
: Neuroinflammatory biomarkers, when used alongside radiology and scoring scales, can aid in predicting prognosis, determining severity and treatment decisions for aSAH, and further studies with larger patient groups are needed to gain more insights.
Keyword
Figure
Reference
-
References
1. Bjerkne Wenneberg S, Odenstedt Hergès H, Svedin P, Mallard C, Karlsson T, Adiels M, et al. Association between inflammatory response and outcome after subarachnoid haemorrhage. Acta Neurol Scand. 143:195–205. 2021.
Article2. Cai L, Zeng H, Tan X, Wu X, Qian C, Chen G. The role of the blood neutrophil-to-lymphocyte ratio in aneurysmal subarachnoid hemorrhage. Front Neurol. 12:671098. 2021.
Article3. Chen L, Pandey S, Shen R, Xu Y, Zhang Q. Increased systemic immuneinflammation index is associated with delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage patients. Front Neurol. 12:745175. 2021.
Article4. Ciurea AV, Palade C, Voinescu D, Nica DA. Subarachnoid hemorrhage and cerebral vasospasm - literature review. J Med Life. 6:120–125. 2013.5. Clozel M, Watanabe H. BQ-123, a peptidic endothelin ETA receptor antagonist, prevents the early cerebral vasospasm following subarachnoid hemorrhage after intracisternal but not intravenous injection. Life Sci. 52:825–834. 1993.
Article6. D’Souza S. Aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol. 27:222–240. 2015.
Article7. Djelilovic-Vranic J, Basic-Kes V, Tiric-Campara M, Djozic E, Kulenovic J. Follow-up of vasospasm by transcranial doppler sonography (TCD) in subarachnoid hemorrhage (SAH). Acta Inform Med. 25:14–18. 2017.
Article8. Dowlati E, Mualem W, Carpenter A, Chang JJ, Felbaum DR, Sur S, et al. Early fevers and elevated neutrophil-to-lymphocyte ratio are associated with repeat endovascular interventions for cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 36:916–926. 2022.
Article9. Feghali J, Kim J, Gami A, Rapaport S, Caplan JM, McDougall CG, et al. Monocyte-based inflammatory indices predict outcomes following aneurysmal subarachnoid hemorrhage. Neurosurg Rev. 44:3499–3507. 2021.
Article10. Geraghty JR, Lung TJ, Hirsch Y, Katz EA, Cheng T, Saini NS, et al. Systemic immune-inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 89:1071–1079. 2021.
Article11. Giede-Jeppe A, Reichl J, Sprügel MI, Lücking H, Hoelter P, Eyüpoglu IY, et al. Neutrophil-to-lymphocyte ratio as an independent predictor for unfavorable functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg. 132:400–407. 2019.
Article12. Guo Y, Liu J, Zeng H, Cai L, Wang T, Wu X, et al. Neutrophil to lymphocyte ratio predicting poor outcome after aneurysmal subarachnoid hemorrhage: a retrospective study and updated meta-analysis. Front Immunol. 13:962760. 2022.
Article13. Li J, Zhou K, Wang L, Cao Q. Predictive model of cerebral vasospasm in subarachnoid hemorrhage based on regression equation. Scanning. 2022:3397967. 2022.
Article14. Luo F, Li Y, Zhao Y, Sun M, He Q, Wen R, et al. Systemic immuneinflammation index predicts the outcome after aneurysmal subarachnoid hemorrhage. Neurosurg Rev. 45:1607–1615. 2022.
Article15. Marazzi TBM, Mendes PV. Updates on aneurysmal subarachnoid hemorrhage: is there anything really new? Arq Neuropsiquiatr. 80(5 Suppl 1):80–87. 2022.
Article16. Neifert SN, Chapman EK, Martini ML, Shuman WH, Schupper AJ, Oermann EK, et al. Aneurysmal subarachnoid hemorrhage: the last decade. Transl Stroke Res. 12:428–446. 2021.
Article17. Nóbrega Lima Rodrigues de Morais A, Ribeiro Baylão VM, Martins Silva T, Gomes Dos Santos A, Azevedo M, J M de Oliveira A. Is neutrophillymphocyte ratio a useful tool for predicting outcome in subarachnoid hemorrhage? A systematic review. Neurosurg Rev. 44:3023–3028. 2021.
Article18. Rouanet C, Silva GS. Aneurysmal subarachnoid hemorrhage: current concepts and updates. Arq Neuropsiquiatr. 77:806–814. 2019.
Article19. Yun S, Yi HJ, Lee DH, Sung JH. Systemic inflammation response index and systemic immune-inflammation index for predicting the prognosis of patients with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 30:105861. 2021.
Article20. Zhang P, Li Y, Zhang H, Wang X, Dong L, Yan Z, et al. Prognostic value of the systemic inflammation response index in patients with aneurismal subarachnoid hemorrhage and a Nomogram model construction. Br J Neurosurg. 2020; [Epub ahead of print].
Article21. Ziu E, Khan Suheb MZ, Mesfin FB : Subarachnoid hemorrhage. Available at : https://www.ncbi.nlm.nih.gov/books/NBK441958/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relation between Thromboembolism and Delayed Ischemic Neurological Deficits in Aneurysmal Subarachnoid Hemorrhage
- Evaluation of Subarachnoid Hemorrhage due to Aneurysmal Rupture and Cerebral Vasospasm by CT
- Factors Related to Clinical Vasospasm after Aneurysmal Subarachnoid Hemorrhage
- The Relationship Between CT Findings and Cerebral Vasospasm in Cerebral Aneursms
- The study of Serum Immunoglobulins and Complement C3 on Predictive Assessing Cerebral Vasospasm and Clinical Grade in Aneurysmal Subarachnoid Hemorrhage