J Yeungnam Med Sci.
2023 Oct;40(4):394-401. 10.12701/jyms.2023.00087.
Depression, sleep quality, and body image disturbances among pregnant women in India: a cross-sectional study
- Affiliations
-
- 1Department of Psychiatry, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, India
- 2Department of Psychiatry, Tata Memorial Hospital, Mumbai, India
- 3Department of Nuclear Medicine, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, India
- 4ASEAN Youth Coalition against Non-Communicable Diseases, Manila, Philippines
- 5National Medical Research Association, London, United Kingdom
- KMID: 2547363
- DOI: http://doi.org/10.12701/jyms.2023.00087
Abstract
- Background
Pregnancy is associated with a number of physical, emotional, and biological changes that can exacerbate maternal psychological disturbances, such as body image concerns and depression. Sleep disturbances during pregnancy can also have adverse impacts. This study aimed to determine the prevalence of depression, sleep disturbances, and body image concerns among pregnant women. The study also examined the relationship between these factors and pregnancy-related variables, such as bad obstetric history and whether the pregnancies were unplanned.
Methods
A cross-sectional study of 146 pregnant patients was conducted at a tertiary care center over 15 months. The patients were administered the Beck Depression Inventory, Pittsburgh Sleep Quality Index, and Body Image Concern Inventory questionnaires. Contingency tables, Fisher exact test, and Spearman correlation were used to identify underlying relationships.
Results
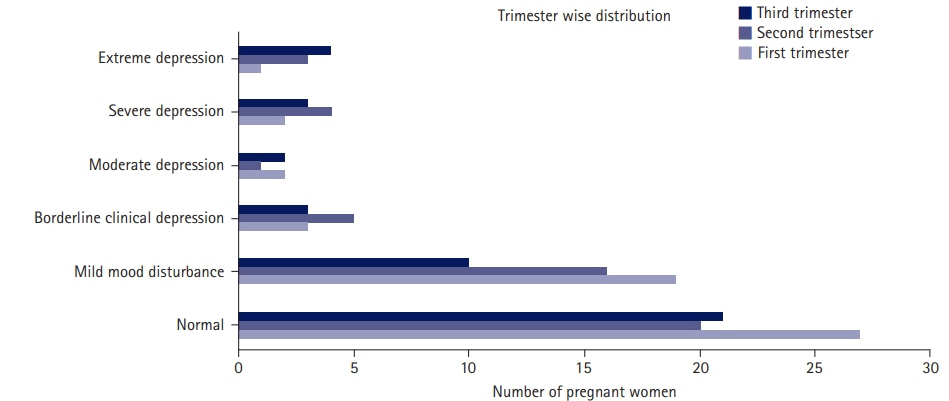
The prevalence of depression was 22.6%. Although body image disturbance was noted in only 2.7% of patients, 46.6% had poor sleep quality. Poor sleep was associated with primigravida status. Bad obstetric history and unplanned pregnancy were associated with depression. Depression was found to be significantly correlated with body image disturbances and poor sleep quality.
Conclusion
Psychiatric disorders were prevalent during pregnancy. This study highlights the importance of screening for depression in pregnant patients. Counselling and caregiver education can be useful for mitigating psychological disturbances. Management of pregnancies by multidisciplinary teams that include psychiatrists could be immensely useful in improving the pregnancy experiences of patients.
Keyword
Figure
Reference
-
References
1. Williams D. Pregnancy: a stress test for life. Curr Opin Obstet Gynecol. 2003; 15:465–71.2. Van Mullem C, Tillett J. Psychiatric disorders in pregnancy. J Perinat Neonatal Nurs. 2009; 23:124–30.
Article3. Hegde SS, Pai KK, Sandeep K. Prevalence of antenatal depression and gender preference: a cross sectional study among Mangalore population, Karnataka, India. J Pharm Biomed Sci. 2013; 30:1011–4.4. George C, Lalitha AR, Antony A, Kumar AV, Jacob KS. Antenatal depression in coastal South India: prevalence and risk factors in the community. Int J Soc Psychiatry. 2016; 62:141–7.
Article5. Varma D, Chandra PS, Thomas T, Carey MP. Intimate partner violence and sexual coercion among pregnant women in India: relationship with depression and post-traumatic stress disorder. J Affect Disord. 2007; 102:227–35.
Article6. Yin X, Sun N, Jiang N, Xu X, Gan Y, Zhang J, et al. Prevalence and associated factors of antenatal depression: systematic reviews and meta-analyses. Clin Psychol Rev. 2021; 83:101932.
Article7. Oren DA, Wisner KL, Spinelli M, Epperson CN, Peindl KS, Terman JS, et al. An open trial of morning light therapy for treatment of antepartum depression. Am J Psychiatry. 2002; 159:666–9.
Article8. Accortt EE, Cheadle AC, Dunkel Schetter C. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J. 2015; 19:1306–37.
Article9. Colten HR, Altevogt BM. Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC): National Academies Press;2006.10. Palagini L, Gemignani A, Banti S, Manconi M, Mauri M, Riemann D. Chronic sleep loss during pregnancy as a determinant of stress: impact on pregnancy outcome. Sleep Med. 2014; 15:853–9.
Article11. Kim Y, Wilkens LR, Schembre SM, Henderson BE, Kolonel LN, Goodman MT. Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other diseases: the Multiethnic Cohort Study. Prev Med. 2013; 57:377–85.
Article12. Wang H, Leng J, Li W, Wang L, Zhang C, Li W, et al. Sleep duration and quality, and risk of gestational diabetes mellitus in pregnant Chinese women. Diabet Med. 2017; 34:44–50.
Article13. Mehta UJ, Siega-Riz AM, Herring AH. Effect of body image on pregnancy weight gain. Matern Child Health J. 2011; 15:324–32.
Article14. Brown A, Rance J, Warren L. Body image concerns during pregnancy are associated with a shorter breast feeding duration. Midwifery. 2015; 31:80–9.
Article15. Adewuya AO, Ola BA, Aloba OO. Prevalence of major depressive disorders and a validation of the Beck Depression Inventory among Nigerian adolescents. Eur Child Adolesc Psychiatry. 2007; 16:287–92.
Article16. Ibeneme SC, Nwosu AO, Ibeneme GC, Bakare MO, Fortwengel G, Limaye D. Distribution of symptoms of post-stroke depression in relation to some characteristics of the vulnerable patients in socio-cultural context. Afr Health Sci. 2017; 17:70–8.
Article17. Amaricai E, Poenaru DV. The post-stroke depression and its impact on functioning in young and adult stroke patients of a rehabilitation unit. J Ment Health. 2016; 25:137–41.
Article18. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28:193–213.
Article19. Ghadakzadeh S, Ghazipour A, Khajeddin N, Karimian N, Borhani M. Body Image Concern Inventory (BICI) for identifying patients with BDD seeking rhinoplasty: using a Persian (Farsi) version. Aesthetic Plast Surg. 2011; 35:989–94.
Article20. Littleton HL, Axsom D, Pury CL. Development of the body image concern inventory. Behav Res Ther. 2005; 43:229–41.
Article21. Littleton H, Breitkopf CR. The Body Image Concern Inventory: validation in a multiethnic sample and initial development of a Spanish language version. Body Image. 2008; 5:381–8.
Article22. Pajulo M, Savonlahti E, Sourander A, Helenius H, Piha J. Antenatal depression, substance dependency and social support. J Affect Disord. 2001; 65:9–17.
Article23. Humayun A, Haider II, Imran N, Iqbal H, Humayun N. Antenatal depression and its predictors in Lahore, Pakistan. East Mediterr Health J. 2013; 19:327–32.
Article24. Kadam KS, Anvekar S, Angane AY, Unnithan VB. The silent survivor: a cross-sectional study of domestic violence, perceived stress, coping strategies, and suicidal risk in the wives of patients with alcohol use disorder. Indian J Soc Psychiatry. 2022; 38:188–94.
Article25. Roomruangwong C, Kanchanatawan B, Sirivichayakul S, Maes M. High incidence of body image dissatisfaction in pregnancy and the postnatal period: associations with depression, anxiety, body mass index and weight gain during pregnancy. Sex Reprod Healthc. 2017; 13:103–9.
Article26. Kadam KS, Bagal RP, Angane AY, Ghorpade GS, Anvekar AR, Unnithan VB. A cross-sectional study of quality of life, psychiatric illness, perceived social support, suicidal risk and selfesteem among patients with burns. J Family Med Prim Care. 2021; 10:432–8.
Article27. Spatuzzi R, Vespa A, Lorenzi P, Miccinesi G, Ricciuti M, Cifarelli W, et al. Evaluation of social support, quality of life, and body image in women with breast cancer. Breast Care (Basel). 2016; 11:28–32.
Article28. Zeng K, Li Y, Yang R. The mediation role of psychological capital between family relationship and antenatal depressive symptoms among women with advanced maternal age: a cross sectional study. BMC Pregnancy Childbirth. 2022; 22:488.
Article29. Duke CH, Williamson JA, Snook KR, Finch KC, Sullivan KL. Association between fruit and vegetable consumption and sleep quantity in pregnant women. Matern Child Health J. 2017; 21:966–73.
Article30. Oboro OF, Ebulue V, Oboro VO, Ohenhen V, Oyewole A, Akindele R, et al. The magnitude and determinants of depressive symptoms amongst women in early pregnancy in Southern Nigeria: a cross-sectional study. S Afr J Psychiatr. 2022; 28:1691.
Article31. Okun ML, Tolge M, Hall M. Low socioeconomic status negatively affects sleep in pregnant women. J Obstet Gynecol Neonatal Nurs. 2014; 43:160–7.
Article32. Wyatt S, Ostbye T, De Silva V, Lakmali P, Long Q. Predictors and occurrence of antenatal depressive symptoms in Galle, Sri Lanka: a mixed-methods cross-sectional study. BMC Pregnancy Childbirth. 2021; 21:758.
Article33. Martínez-Galiano JM, Hernández-Martínez A, Rodríguez-Almagro J, Delgado-Rodríguez M, Gómez-Salgado J. Relationship between parity and the problems that appear in the postpartum period. Sci Rep. 2019; 9:11763.
Article34. Bassi M, Delle Fave A, Cetin I, Melchiorri E, Pozzo M, Vescovelli F, et al. Psychological well-being and depression from pregnancy to postpartum among primiparous and multiparous women. J Reprod Infant Psychol. 2017; 35:183–95.
Article35. Chen YH, Huang JP, Au HK, Chen YH. High risk of depression, anxiety, and poor quality of life among experienced fathers, but not mothers: a prospective longitudinal study. J Affect Disord. 2019; 242:39–47.
Article36. Fekadu Dadi A, Miller ER, Mwanri L. Antenatal depression and its association with adverse birth outcomes in low and middle-income countries: a systematic review and meta-analysis. PLoS One. 2020; 15:e0227323.
Article37. Moreau C, Bonnet C, Beuzelin M, Blondel B. Pregnancy planning and acceptance and maternal psychological distress during pregnancy: results from the National Perinatal Survey, France, 2016. BMC Pregnancy Childbirth. 2022; 22:162.
Article38. Goyal D, Gay CL, Lee KA. Patterns of sleep disruption and depressive symptoms in new mothers. J Perinat Neonatal Nurs. 2007; 21:123–9.
Article39. Wolfson AR, Crowley SJ, Anwer U, Bassett JL. Changes in sleep patterns and depressive symptoms in first-time mothers: last trimester to 1-year postpartum. Behav Sleep Med. 2003; 1:54–67.
Article40. Cash TF. The treatment of body image disturbances. In : Thompson J, editor. Body image, eating disorders, and obesity: an integrative guide for assessment and treatment. Washington (DC): American Psychological Association;1996. p. 83–107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relations between Stress and Quality of Life among Women in Late Pregnancy: The Parallel Mediating Role of Depressive Symptoms and Sleep Quality
- Influencing Factors on Antenatal Depression
- Quality of Sleep and Quality of Life during Pregnancy
- Prevalence of Internet Addiction, Poor Sleep Quality, and Depressive Symptoms Among Medical Students: A Cross-Sectional Study
- Sleep in Pregnancy