J Yeungnam Med Sci.
2023 Oct;40(4):343-351. 10.12701/jyms.2023.00717.
Management and rehabilitation of moderate-to-severe diabetic foot infection: a narrative review
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea
- KMID: 2547357
- DOI: http://doi.org/10.12701/jyms.2023.00717
Abstract
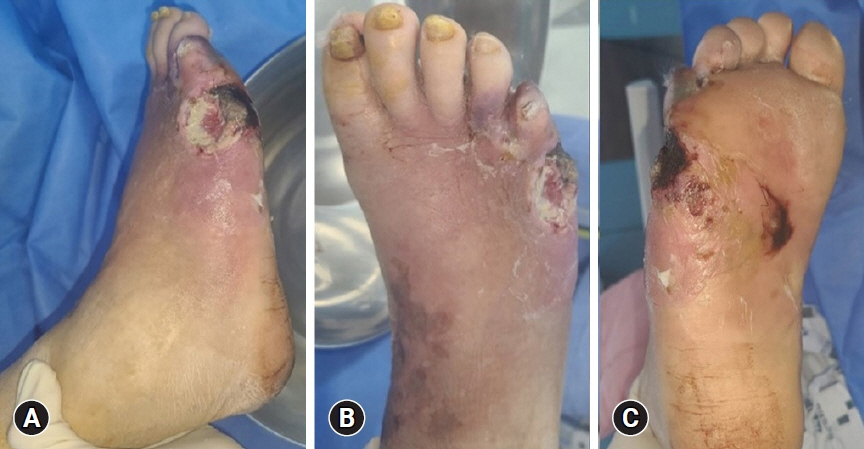
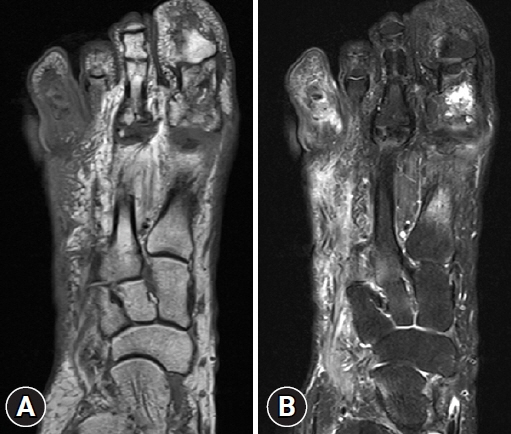
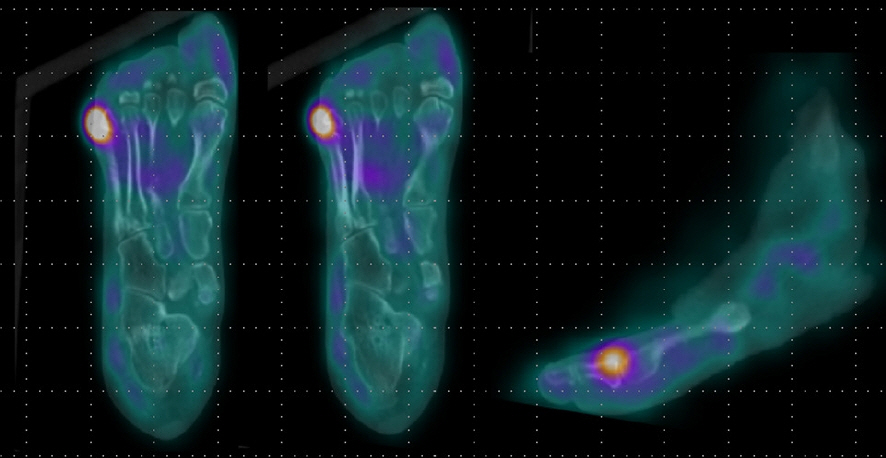
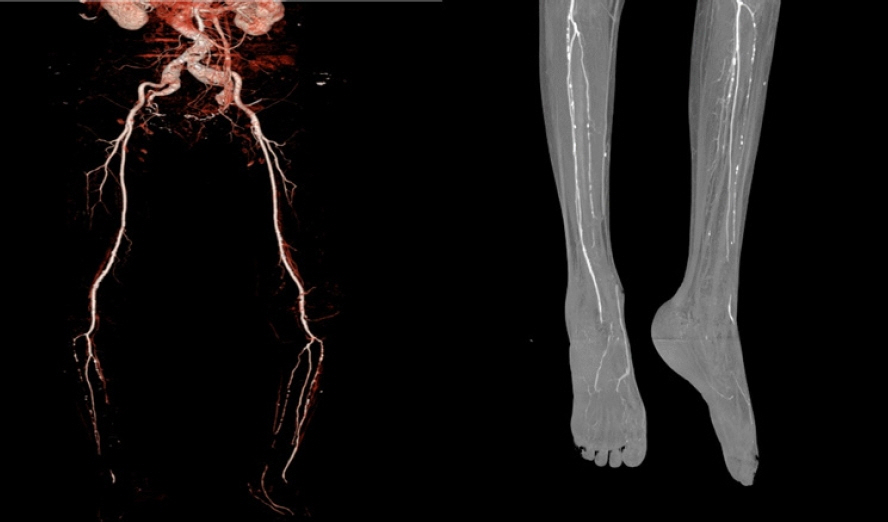
- Diabetic foot is one of the most devastating consequences of diabetes, resulting in amputation and possibly death. Therefore, early detection and vigorous treatment of infections in patients with diabetic foot are critical. This review seeks to provide guidelines for the therapy and rehabilitation of patients with moderate-to-severe diabetic foot. If a diabetic foot infection is suspected, bacterial cultures should be initially obtained. Numerous imaging studies can be used to identify diabetic foot, and recent research has shown that white blood cell single-photon emission computed tomography/computed tomography has comparable diagnostic specificity and sensitivity to magnetic resonance imaging. Surgery is performed when a diabetic foot ulcer is deep and is accompanied by bone and soft tissue infections. Patients should be taught preoperative rehabilitation before undergoing stressful surgery. During surgical procedures, it is critical to remove all necrotic tissue and drain the inflammatory area. It is critical to treat wounds with suitable dressings after surgery. Wet dressings promote the formation of granulation tissues and new blood vessels. Walking should begin as soon as the patient’s general condition allows it, regardless of the wound status or prior walking capacity. Adequate treatment of comorbidities, including hypertension and dyslipidemia, and smoking cessation are necessary. Additionally, broad-spectrum antibiotics are required to treat diabetic foot infections.
Keyword
Figure
Cited by 1 articles
-
Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Chul Hyun Park
J Yeungnam Med Sci. 2023;40(4):319-320. doi: 10.12701/jyms.2023.01011.
Reference
-
References
1. Lee CW. Diagnosis and management of diabetic foot. J Korean Diabetes. 2018; 19:168–74.
Article2. Bae SY. Treatment of diabetic foot: procedures, surgery, and care. Monthly Diabetes. 2013; 289:26–36.3. Armstrong DG, Wrobel J, Robbins JM. Guest Editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007; 4:286–7.
Article4. Shankar P, Grewal VS, Agrawal S, Nair SV. A study on quality of life among lower limb amputees at a tertiary prosthetic rehabilitation center. Med J Armed Forces India. 2020; 76:89–94.
Article5. Ahn KJ. Epidemiology of diabetic foot disease. J Korean Diabetes. 2011; 12:72–5.
Article6. Rubio JA, Jiménez S, Lázaro-Martínez JL. Mortality in patients with diabetic foot ulcers: causes, risk factors, and their association with evolution and severity of ulcer. J Clin Med. 2020; 9:3009.
Article7. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005; 293:217–28.
Article8. Ahmad A, Abujbara M, Jaddou H, Younes NA, Ajlouni K. Anxiety and depression among adult patients with diabetic foot: prevalence and associated factors. J Clin Med Res. 2018; 10:411–8.
Article9. Choi Y. Rehabilitation of patients after diabetic foot amputation. J Korean Med Assoc. 2021; 64:537–42.
Article10. Shi C, Wang C, Liu H, Li Q, Li R, Zhang Y, et al. Selection of appropriate wound dressing for various wounds. Front Bioeng Biotechnol. 2020; 8:182.
Article11. Williams DT, Hilton JR, Harding KG. Diagnosing foot infection in diabetes. Clin Infect Dis. 2004; 39(Suppl 2):S83–6.
Article12. Weigelt C, Rose B, Poschen U, Ziegler D, Friese G, Kempf K, et al. Immune mediators in patients with acute diabetic foot syndrome. Diabetes Care. 2009; 32:1491–6.
Article13. Wang Y, Shao T, Wang J, Huang X, Deng X, Cao Y, et al. An update on potential biomarkers for diagnosing diabetic foot ulcer at early stage. Biomed Pharmacother. 2021; 133:110991.
Article14. Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020; 36(Suppl 1):e3280.
Article15. Seo DK, Lee HS. Management of diabetic foot ulcer. J Korean Foot Ankle Soc. 2014; 18:1–7.
Article16. Erdman WA, Buethe J, Bhore R, Ghayee HK, Thompson C, Maewal P, et al. Indexing severity of diabetic foot infection with 99mTc-WBC SPECT/CT hybrid imaging. Diabetes Care. 2012; 35:1826–31.
Article17. Lauri C, Glaudemans AW, Campagna G, Keidar Z, Muchnik Kurash M, Georga S, et al. Comparison of white blood cell scintigraphy, FDG PET/CT and MRI in suspected diabetic foot infection: results of a large retrospective multicenter study. J Clin Med. 2020; 9:1645.
Article18. Low KT, Peh WC. Magnetic resonance imaging of diabetic foot complications. Singapore Med J. 2015; 56:23–33.
Article19. Sherwood A, Rubitschung K, Killeen A, Crisologo P, Haley R, Hwang H, et al. Comparison of WBC-SPECT/CT and MRI in diagnosis and evaluation of antibiotic response in diabetic foot osteomyelitis. J Nucl Med. 2022; 63(Suppl 2):2772.20. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020; 36(Suppl 1):e3266.
Article21. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Fitridge R, Game F, et al. 2023 IWGDF guidelines on the prevention and management of diabetes-related foot disease [Internet]. The International Working Group on the Diabetic Foot (IWGDF); 2023 [cited 2023 Aug 9]. https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-Guidelines-2023.pdf.22. Song JY. Antimicrobial therapy in diabetic foot infections. J Korean Diabetes. 2011; 12:83–7.
Article23. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Fitridge R, Game F, et al. Practical guidelines on the prevention and management of diabetes-related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev. 2023; e3657.
Article24. Hong JP, Oh TS. An algorithm for limb salvage for diabetic foot ulcers. Clin Plast Surg. 2012; 39:341–52.
Article25. Turan Y, Ertugrul BM, Lipsky BA, Bayraktar K. Does physical therapy and rehabilitation improve outcomes for diabetic foot ulcers? World J Exp Med. 2015; 5:130–9.
Article26. Uustal H. Prosthetic rehabilitation issues in the diabetic and dysvascular amputee. Phys Med Rehabil Clin N Am. 2009; 20:689–703.
Article27. Ditmyer MM, Topp R, Pifer M. Prehabilitation in preparation for orthopaedic surgery. Orthop Nurs. 2002; 21:43–51.
Article28. Hijmans JM, Dekker R, Geertzen JH. Pre-operative rehabilitation in lower-limb amputation patients and its effect on post-operative outcomes. Med Hypotheses. 2020; 143:110134.
Article29. Castillo R, Haas A. Chest physical therapy: comparative efficacy of preoperative and postoperative in the elderly. Arch Phys Med Rehabil. 1985; 66:376–9.30. Lee DY, Kim IY. Surgical treatment of diabetic foot disease. J Korean Diabetes. 2011; 12:88–94.
Article31. Brem H, Stojadinovic O, Diegelmann RF, Entero H, Lee B, Pastar I, et al. Molecular markers in patients with chronic wounds to guide surgical debridement. Mol Med. 2007; 13:30–9.
Article32. Oh TS, Lee HS, Hong JP. Diabetic foot reconstruction using free flaps increases 5-year-survival rate. J Plast Reconstr Aesthet Surg. 2013; 66:243–50.
Article33. Lee HS. Prevention and management of the diabetic foot. J Korean Med Assoc. 2013; 56:220–8.
Article34. Rezvani Ghomi E, Khalili S, Nouri Khorasani S, Esmaeely Neisiany R, Ramakrishna S. Wound dressings: current advances and future directions. J App Polym Sci. 2019; 136:47738.
Article35. Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020; 125:492–504.
Article36. Von Rueden KT, Harris JR. Pulmonary dysfunction related to immobility in the trauma patient. AACN Clin Issues. 1995; 6:212–28.
Article37. Yoo H, Choo E, Lee S. Study of hospitalization and mortality in Korean diabetic patients using the diabetes complications severity index. BMC Endocr Disord. 2020; 20:122.
Article