Anesth Pain Med.
2023 Jul;18(3):252-259. 10.17085/apm.22252.
Comparison of remimazolam–remifentanil and propofol–remifentanil during laparoscopic cholecystectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Dong-A university Hospital, Busan, Korea
- KMID: 2547033
- DOI: http://doi.org/10.17085/apm.22252
Abstract
- Background
Remimazolam is a novel benzodiazepine with fast onset and short half-life. We compared the effects of remimazolam and propofol on recovery profiles for general anesthesia in patients undergoing laparoscopic cholecystectomy.
Methods
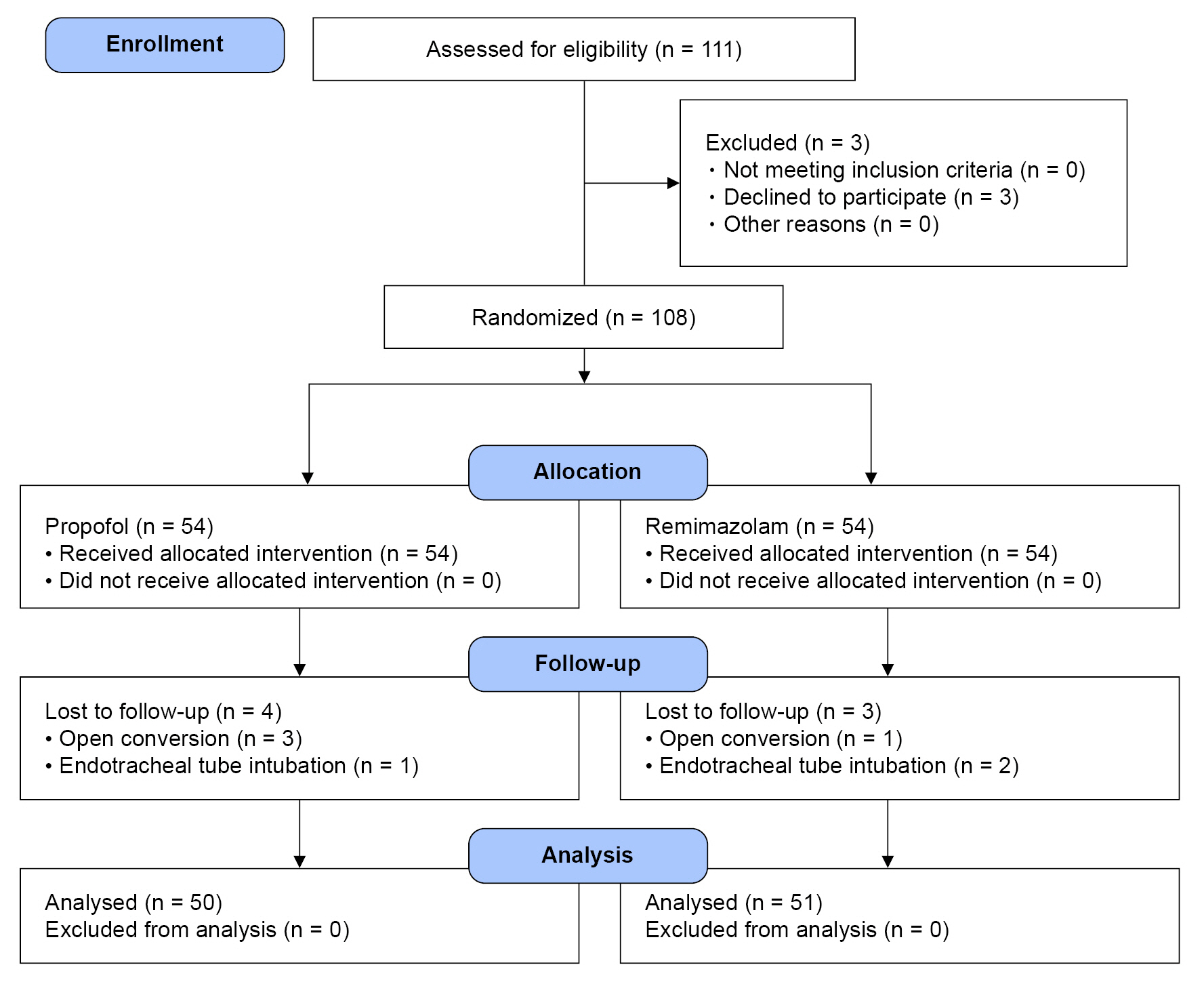
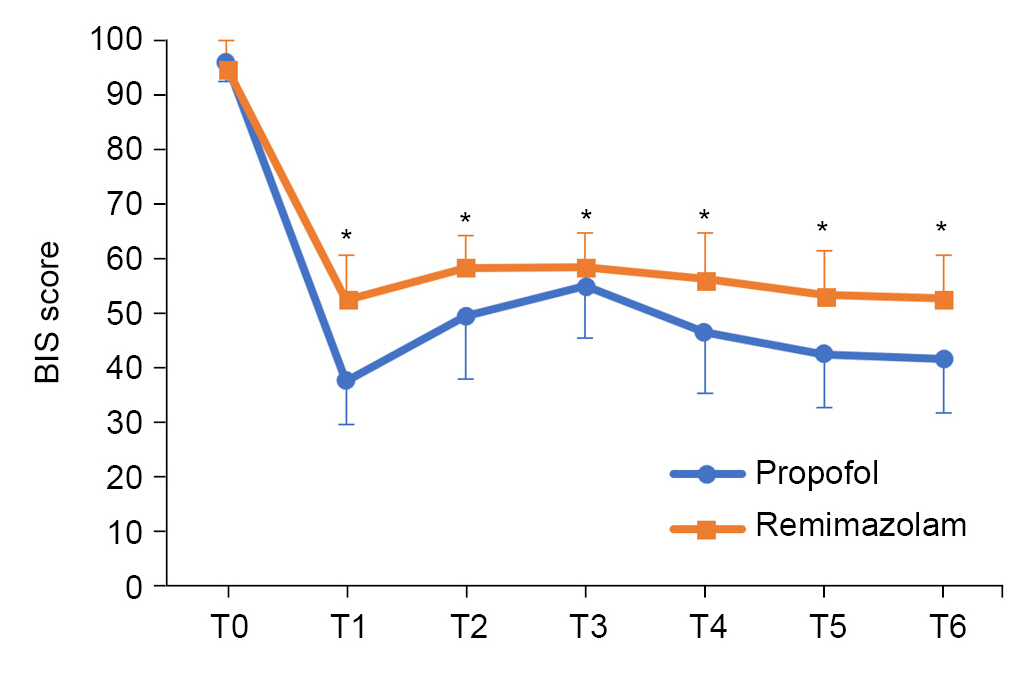
We randomly assigned 108 patients to either a remimazolam (n=54) or propofol (n=54) group. Remimazolam and propofol were used for induction and maintanance of anesthesia. Following anesthesia, we recorded the time until an Aldrete score of 9 was achieved as the primary surrogate marker of complete recovery. The time to reach a Modified Observer’s Assessment of Alertness/Sedation (MOAA/S) score of 2 and the time from the end of anesthesia to eye opening time, recovery time of orientation, time to spontaneous breathing, extubation time, and the time required for analgesics were measured. Heart rate, blood pressure, and bispectral index were assessed before, during, and after pneumoperitoneum.
Results
We included 101 patients in the analysis. In the remimazolam group, it took longer to reach an Aldrete score of 9 after the drug infusion ended (P = 0.031). There was no difference in the time to reach MOAA/S 2 between the two groups. The time to eye opening, recovery time of orientation, and time required for analgesics were longer and heart rate was higher in the remimazolam group. Neither blood pressure, nor extubation time differed between groups.
Conclusions
Remimazolam and propofol provided safe induction and maintenance of anesthesia in patients undergoing laparoscopic cholecystectomy. The recovery time from anesthesia was longer than that with propofol. Fewer hemodynamic changes were observed with remimazolam, but further studies are needed.
Keyword
Figure
Reference
-
1. Juckenhöfel S, Feisel C, Schmitt HJ, Biedler A. TIVA with propofol-remifentanil or balanced anesthesia with sevoflurane-fentanyl in laparoscopic operations. Hemodynamics, awakening and adverse effects. Anaesthesist. 1999; 48:807–12.
Article2. Kiriyama S, Naitoh H, Kuwano H. Propofolsedationduringendoscopictreatmentforearlygastriccancercomparedtomidazolam. World J Gastroenterol. 2014; 20:11985–90.
Article3. Zhang Y, Shan GJ, Zhang YX, Cao SJ, Zhu SN, Li HJ, First Study of Perioperative Organ Protection (SPOP1) investigators, et al. Propofolcomparedwithsevofluranegeneralanaesthesiaisassociatedwithdecreaseddelayedneurocognitiverecoveryinolderadults. Br J Anaesth. 2018; 121:595–604.
Article4. Sahinovic MM, Struys MMRF, Absalom AR. Clinical pharmacokinetics and pharmacodynamics of propofol. Clin Pharmacokinet. 2018; 57:1539–58.
Article5. Hemphill S, McMenamin L, Bellamy MC, Hopkins PM. Propofol infusion syndrome: a structured literature review and analysis of published case reports. Br J Anaesth. 2019; 122:448–59.
Article6. Wesolowski AM, Zaccagnino MP, Malapero RJ, Kaye AD, Urman RD. Remimazolam: Pharmacologic Considerations and Clinical Role in Anesthesiology. Pharmacotherapy. 2016; 36:1021–7.
Article7. Tuk B, Van Oostenbruggen MF van, Herben VM, Mandema JW, Danhof M. Characterization of the pharmacodynamic interaction between parent drug and active metabolite in vivo: midazolam and alpha-OH-midazolam. J Pharmacol Exp Ther. 1999; 289:1067–74.8. Cornett EM, Novitch MB, Brunk AJ, Davidson KS, Menard BL, Urman RD, et al. New benzodiazepines for sedation. Best Pract Res Clin Anaesthesiol. 2018; 32:149–64.
Article9. Noor N, Legendre R, Cloutet A, Chitneni A, Varrassi G, Kaye AD. A comprehensive review of remimazolam for sedation. Heal Psychol Res. 2021; 9:1–11.
Article10. Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med. 2022; 17:1–11.
Article11. Schüttler J, Eisenried A, Lerch M, Fechner J, Jeleazcov C, Ihmsen H. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers Part I. Pharmacokinetics and clinical pharmacodynamics. Anesthesiology. 2020; 132:636–51.12. Liu T, Lai T, Chen J, Lu Y, He F, Chen Y, et al. Effect of remimazolam induction on hemodynamics in patients undergoing valve replacement surgery: A randomized, double-blind, controlled trial. Pharmacol Res Perspect. 2021; 9:e00851.
Article13. Shi F, Chen Y, Li H, Zhang Y, Zhao T. Efficacy and Safety of Remimazolam Tosilate versus Propofol for General Anesthesia in Cirrhotic Patients Undergoing Endoscopic Variceal Ligation. Int J Gen Med. 2022; 15:583–91.
Article14. Dai G, Pei L, Duan F, Liao M, Zhang Y, Zhu M, et al. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol. 2021; 87:1073–9.
Article15. Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020; 34:543–53.
Article16. Zhang X, Li S, Liu J. Efficacy and safety of remimazolam besylate versus propofol during hysteroscopy: single-centre randomized controlled trial. BMC Anesthesiol. 2021; 21:156.
Article17. Pastis NJ, Yarmus LB, Schippers F, Ostroff R, Chen A, Akulian J, et al. Safety and Efficacy of Remimazolam Compared With Placebo and Midazolam for Moderate Sedation During Bronchoscopy. Chest. 2019; 155:137–46.
Article18. Mashour GA, Kent C, Picton P, Ramachandran SK, Tremper KK, Turner CR, et al. Assessment of intraoperative awareness with explicit recall: A comparison of 2 METHODS. Anesth Analg. 2013; 116:889–91.19. Chiang MH, Wu SC, Hsu SW, Chin JC. Bispectral Index and non-Bispectral Index anesthetic protocols on postoperative recovery outcomes. Minerva Anestesiol. 2018; 84:216–28.
Article20. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral Index for Improving Anaesthetic Delivery and Postoperative Recovery, Cochrane Database of Systematic Reviews. Cochrane Database Syst Rev. 2014; 17:CD003843.21. Kazuhiro S, Keiko N, Shota T, Kazuya I, Kosuke N, Shinnosuke T, et al. Neurological sedative indicators during general anesthesia with remimazolam. J Anesth. 2022; 36:194–200.
Article22. Oh J, Park SY, Lee SY, Song JY, Lee GY, Park JH, et al. Determination of the 95% effective dose of remimazolam to achieve loss of consciousness during anesthesia induction in different age groups. Korean J Anesthesiol. 2022; 75:510–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Remifentanil and Fentanyl on Postoperative Nausea and Vomiting in Laparoscopic Cholecystectomy with using Propofol
- Comparison of Total Intravenous Anesthesia and Sevoflurane-Alfentanil Anesthesia for Laparoscopic Cholecystectomy
- Effects of preanesthetic single administration of dexmedetomidine on the remifentanil and propofol requirement during laparoscopic cholecystectomy
- The Experience of the Total Intravenous Anesthesia of Patient with Noonan Syndrome: A case report
- The Effects of Different Doses of Remifentanil on Propofol Injection Pain: A Placebo Controlled Comparison of Ketamine