Acute Crit Care.
2023 Aug;38(3):286-297. 10.4266/acc.2023.00507.
Patterns of inflammatory immune responses in patients with septic shock receiving vitamin C, hydrocortisone, and thiamine: clustering analysis in Korea
- Affiliations
-
- 1Department of Global Innovative Drugs, Graduate School of Chung-Ang University, Chung-Ang University, Seoul, Korea
- 2Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 3College of Pharmacy, Chung-Ang University, Seoul, Korea
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2547022
- DOI: http://doi.org/10.4266/acc.2023.00507
Abstract
- Background
Sepsis is characterized by heterogeneous immune responses that may evolve during the course of illness. This study identified inflammatory immune responses in septic patients receiving vitamin C, hydrocortisone, and thiamine.
Methods
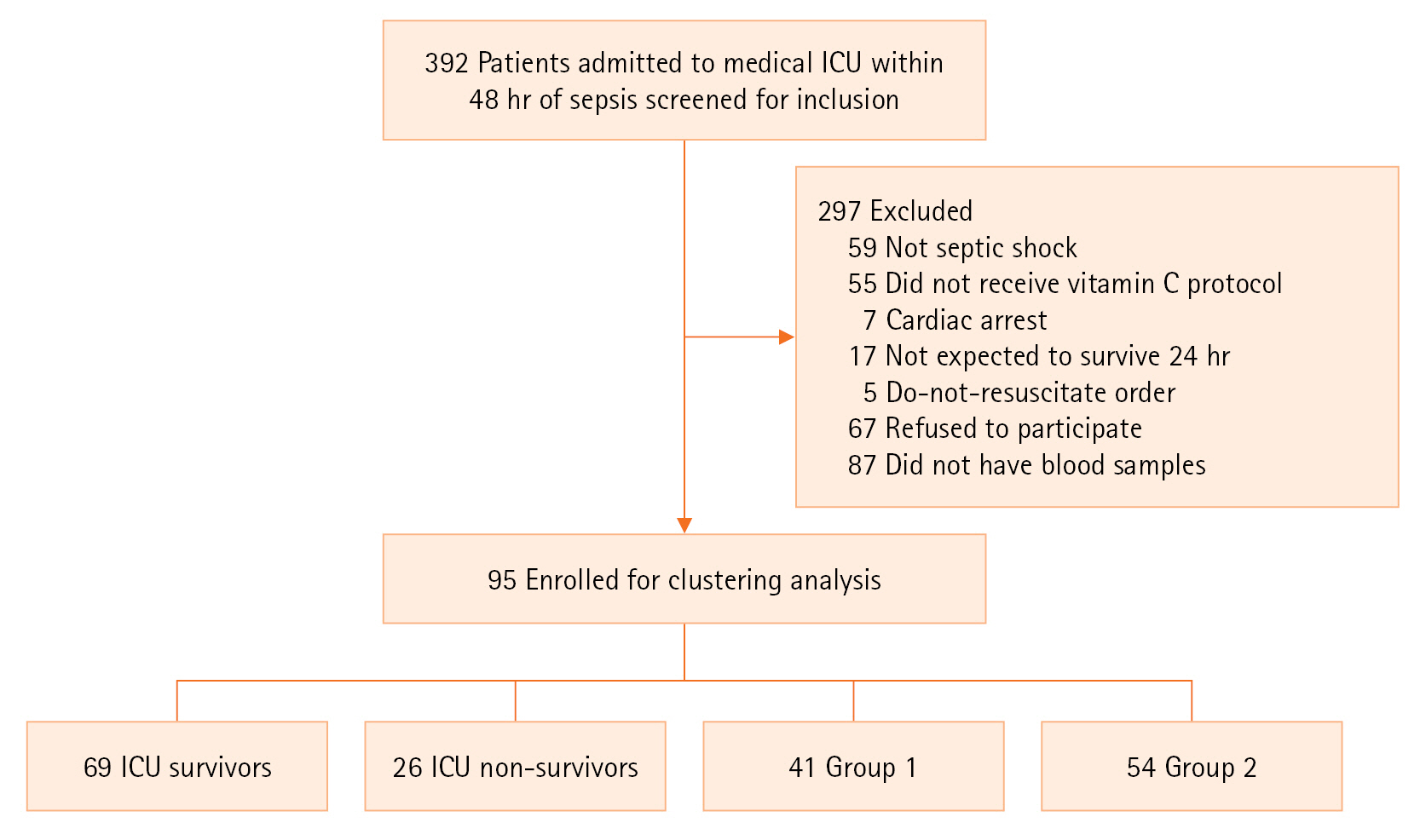
This was a single-center, post-hoc analysis of 95 patients with septic shock who received the vitamin C protocol. Blood samples were drawn on days 1–2, 3–4, and 6–8 after shock onset. Group-based multi-trajectory modeling was used to identify immune trajectory groups.
Results
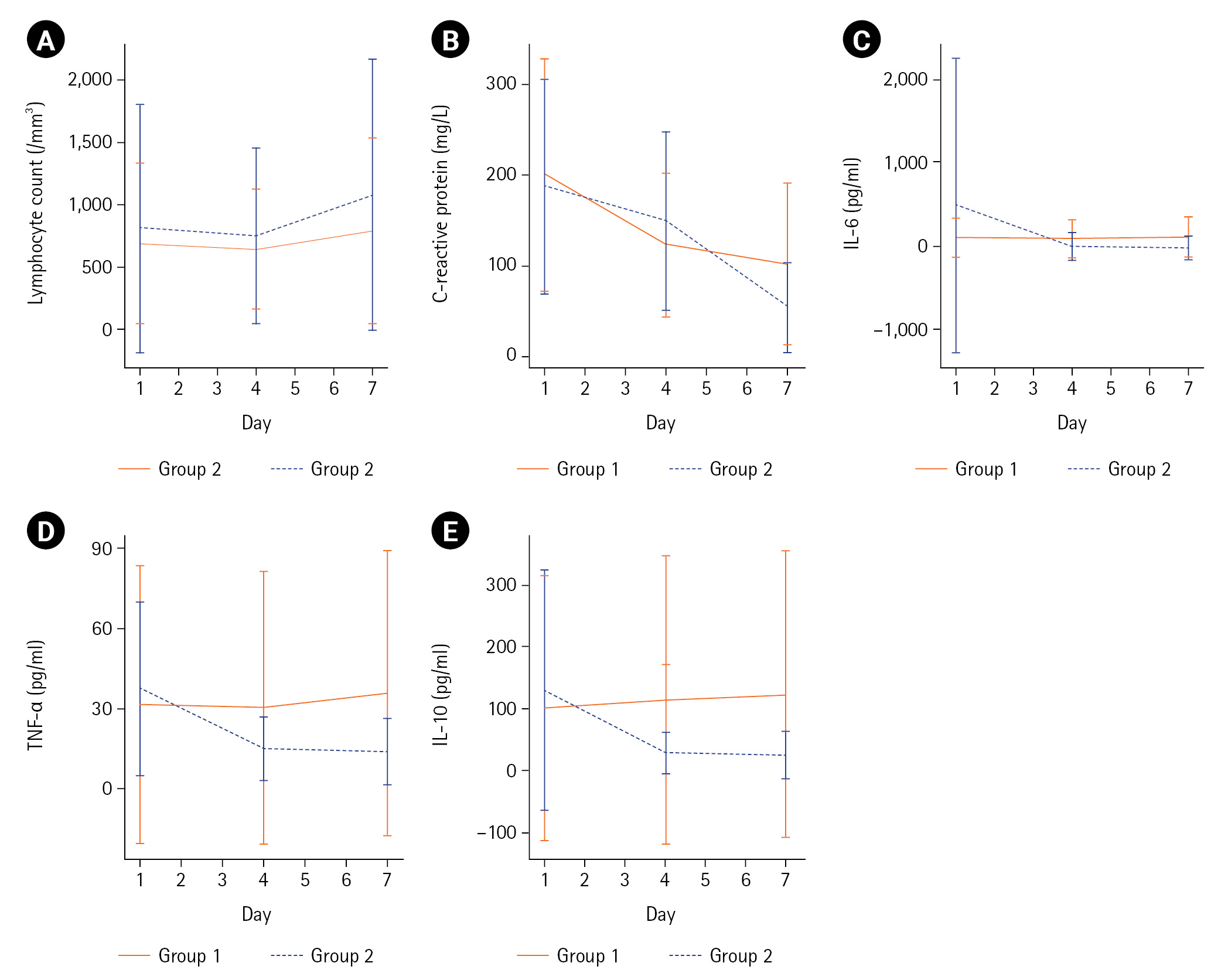
The median age was 78 years (interquartile range, 70–84 years), and 56% were male. Clustering analysis identified group 1 (n=41), which was characterized by lower interleukin (IL)-6, tumor necrosis factor (TNF)-α, and IL-10 levels, and these levels remained stationary or mildly increased until day 7. Conversely, group 2 (n=54) expressed initially higher IL-6, TNF-α, and IL-10 levels that decreased rapidly by day 4. There was a nonsignificant increase in lymphocyte count and a decrease in C-reactive protein level until day 7 in group 2. The intensive care unit mortality rate was significantly lower in group 2 (39.0% vs. 18.5%, P=0.03). Group 2 also had a significantly higher decrease in the mean (standard deviation) vasopressor dose (norepinephrine equivalent: –0.09±0.16 μg/kg/min vs. –0.23±0.31 μg/kg/min, P<0.001) and Sequential Organ Failure Assessment score (0±5 vs. –4±3, P=0.002) between days 1 and 4.
Conclusions
There may be different subphenotypes in septic patients receiving the vitamin C protocol.
Keyword
Figure
Reference
-
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–10.
Article2. Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. 2020; 395:200–11.
Article3. Gotts JE, Matthay MA. Sepsis: pathophysiology and clinical management. BMJ. 2016; 353:i1585.
Article4. Laterre PF, Pickkers P, Marx G, Wittebole X, Meziani F, Dugernier T, et al. Safety and tolerability of non-neutralizing adrenomedullin antibody adrecizumab (HAM8101) in septic shock patients: the AdrenOSS-2 phase 2a biomarker-guided trial. Intensive Care Med. 2021; 47:1284–94.
Article5. Kashiouris MG, L'Heureux M, Cable CA, Fisher BJ, Leichtle SW, Fowler AA. The emerging role of vitamin c as a treatment for sepsis. Nutrients. 2020; 12:292.
Article6. Barabutis N, Khangoora V, Marik PE, Catravas JD. Hydrocortisone and ascorbic acid synergistically prevent and repair lipopolysaccharide-induced pulmonary endothelial barrier dysfunction. Chest. 2017; 152:954–62.
Article7. Donnino MW, Carney E, Cocchi MN, Barbash I, Chase M, Joyce N, et al. Thiamine deficiency in critically ill patients with sepsis. J Crit Care. 2010; 25:576–81.
Article8. Assouline B, Faivre A, Verissimo T, Sangla F, Berchtold L, Giraud R, et al. Thiamine, ascorbic acid, and hydrocortisone as a metabolic resuscitation cocktail in sepsis: a meta-analysis of randomized controlled trials with trial sequential analysis. Crit Care Med. 2021; 49:2112–20.
Article9. Sato R, Hasegawa D, Prasitlumkum N, Ueoka M, Nishida K, Takahashi K, et al. Effect of IV high-dose vitamin C on mortality in patients with sepsis: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2021; 49:2121–30.
Article10. Lamontagne F, Masse MH, Menard J, Sprague S, Pinto R, Heyland DK, et al. Intravenous vitamin C in adults with sepsis in the intensive care unit. N Engl J Med. 2022; 386:2387–98.
Article11. Iglesias J, Vassallo AV, Liesenfeld O, Levine JS, Patel VV, Sullivan JB, et al. A 33-mRNA classifier is able to produce inflammopathic, adaptive, and coagulopathic endotypes with prognostic significance: the outcomes of metabolic resuscitation using ascorbic acid, thiamine, and glucocorticoids in the early treatment of sepsis (ORANGES) trial. J Pers Med. 2020; 11:9.
Article12. Kim WY, Jung JW, Choi JC, Shin JW, Kim JY. Subphenotypes in patients with septic shock receiving vitamin C, hydrocortisone, and thiamine: a retrospective cohort analysis. Nutrients. 2019; 11:2976.
Article13. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43:304–77.14. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.15. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article16. Khanna A, English SW, Wang XS, Ham K, Tumlin J, Szerlip H, et al. Angiotensin II for the treatment of vasodilatory shock. N Engl J Med. 2017; 377:419–30.
Article17. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–33.18. de Grooth HJ, Elbers PWG, Vincent JL. Vitamin C for sepsis and acute respiratory failure. JAMA. 2020; 323:792.
Article19. Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018; 27:2015–23.
Article20. Magrini A. Assessment of agricultural sustainability in European Union countries: a group-based multivariate trajectory approach. AStA Adv Stat Anal. 2022; 106:673–703.
Article21. Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014; 2:611–20.
Article22. Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018; 6:691–8.23. Antcliffe DB, Burnham KL, Al-Beidh F, Santhakumaran S, Brett SJ, Hinds CJ, et al. Transcriptomic signatures in sepsis and a differential response to steroids. from the VANISH Randomized Trial. Am J Respir Crit Care Med. 2019; 199:980–6.
Article24. Fowler AA 3rd, Syed AA, Knowlson S, Sculthorpe R, Farthing D, DeWilde C, et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014; 12:32.
Article25. Zhang J, Rao X, Li Y, Zhu Y, Liu F, Guo G, et al. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann Intensive Care. 2021; 11:5.
Article26. Bhavani SV, Carey KA, Gilbert ER, Afshar M, Verhoef PA, Churpek MM. Identifying novel sepsis subphenotypes using temperature trajectories. Am J Respir Crit Care Med. 2019; 200:327–35.
Article27. Kellum JA, Pike F, Yealy DM, Huang DT, Shapiro NI, Angus DC, et al. Relationship between alternative resuscitation strategies, host response and injury biomarkers, and outcome in septic shock: analysis of the protocol-based care for early septic shock study. Crit Care Med. 2017; 45:438–45.
Article28. Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting interleukin-6 signaling in clinic. Immunity. 2019; 50:1007–23.
Article29. Stanic B, van de Veen W, Wirz OF, Rückert B, Morita H, Söllner S, et al. IL-10-overexpressing B cells regulate innate and adaptive immune responses. J Allergy Clin Immunol. 2015; 135:771–80.
Article30. Matsumoto H, Ogura H, Shimizu K, Ikeda M, Hirose T, Matsuura H, et al. The clinical importance of a cytokine network in the acute phase of sepsis. Sci Rep. 2018; 8:13995.
Article31. Weidhase L, Wellhöfer D, Schulze G, Kaiser T, Drogies T, Wurst U, et al. Is Interleukin-6 a better predictor of successful antibiotic therapy than procalcitonin and C-reactive protein?: a single center study in critically ill adults. BMC Infect Dis. 2019; 19:150.
Article32. Härtel C, Strunk T, Bucsky P, Schultz C. Effects of vitamin C on intracytoplasmic cytokine production in human whole blood monocytes and lymphocytes. Cytokine. 2004; 27:101–6.
Article33. van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017; 17:407–20.
Article34. Black S, Kushner I, Samols D. C-reactive Protein. J Biol Chem. 2004; 279:48487–90.
Article35. Nakamura K, Ogura K, Nakano H, Naraba H, Takahashi Y, Sonoo T, et al. C-reactive protein clustering to clarify persistent inflammation, immunosuppression and catabolism syndrome. Intensive Care Med. 2020; 46:437–43.
Article36. Frommelt MA, Kory P, Long MT. Letter on Update to the vitamin C, thiamine, and steroids in sepsis (VICTAS) protocol. Trials. 2020; 21:350.
Article37. Jung SY, Lee MT, Baek MS, Kim WY. Vitamin C for ≥ 5 days is associated with decreased hospital mortality in sepsis subgroups: a nationwide cohort study. Crit Care. 2022; 26:3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined treatment with vitamin C, hydrocortisone and thiamine does not attenuate morbidity and mortality of septic sheep
- Vitamin D and Immune Responses
- Combined hydrocortisone, ascorbic acid, and thiamine therapy for septic shock with complicated intraabdominal infection: before and after cohort study
- The Effect of the Vitamin Protocol for Treating Sepsis or Septic Shock in Pediatric Intensive Care Unit
- Damage-Associated Molecular Patterns in Inflammatory Diseases