J Korean Med Sci.
2023 Oct;38(40):e327. 10.3346/jkms.2023.38.e327.
Case 15: A 53-Year-Old Woman With Bilateral Leg Pain and Weakness
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Rheumatology, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Rheumatology, Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2546935
- DOI: http://doi.org/10.3346/jkms.2023.38.e327
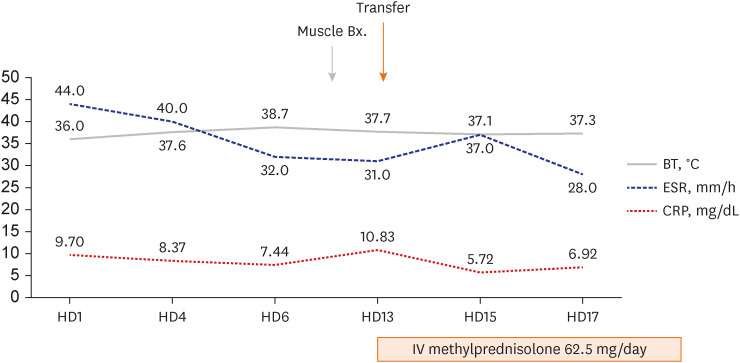
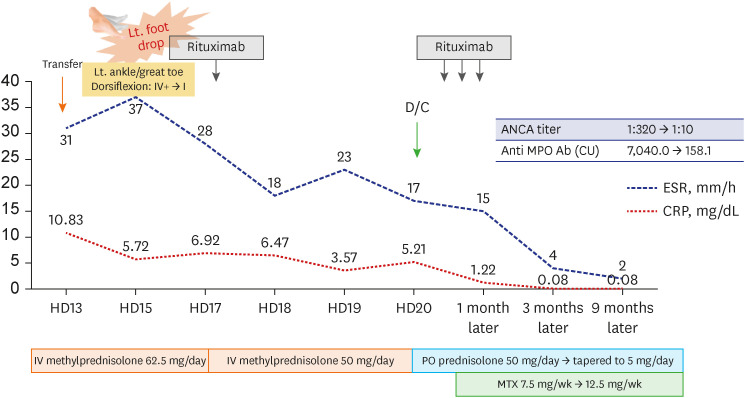
Figure
Reference
-
1. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007; 66(2):222–227. PMID: 16901958.2. Choi CB, Park YB, Lee SW. Antineutrophil cytoplasmic antibody-associated vasculitis in Korea: a narrative review. Yonsei Med J. 2019; 60(1):10–21. PMID: 30554486.3. Suppiah R, Robson JC, Grayson PC, Ponte C, Craven A, Khalid S, et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for microscopic polyangiitis. Arthritis Rheumatol. 2022; 74(3):400–406. PMID: 35106973.4. Chung SA, Langford CA, Maz M, Abril A, Gorelik M, Guyatt G, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the management of antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheumatol. 2021; 73(8):1366–1383. PMID: 34235894.5. Wallace ZS, Miloslavsky EM. Management of ANCA associated vasculitis. BMJ. 2020; 368:m421. PMID: 32188597.6. Conticini E, d’Alessandro M, Al Khayyat SG, D’Alessandro R, D’Ignazio E, Pata AP, et al. Inflammatory muscle involvement in systemic vasculitis: a systematic review. Autoimmun Rev. 2022; 21(3):103029. PMID: 34971804.7. Oiwa H, Kurashige T. Muscle weakness as a presenting symptom in ANCA-associated vasculitis. Eur J Rheumatol. 2018; 5(2):139–141. PMID: 30185364.8. Nagiah S, Saranapala DM. Severe proximal muscle weakness with normal CK as a presenting feature of ANCA-associated vasculitis. BMJ Case Rep. 2020; 13(1):e232854.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Leg Weakness Caused by Bilateral Piriformis Syndrome: A Case Report
- A Case of Gait Disturbance Resolved with Hysterectomy in a Woman
- Cauda Equina Syndrome Caused by Bilateral Facet Cyst Accompanying Spinal Stenosis
- Motor Weakness on Lower Extremities after the Combined Spinal-epidural Anesthesia and Analgesia: A case report
- Multiple Hemangioendotheliomas of the Spinal Cord and Cauda Equina: Case Report