J Liver Cancer.
2023 Sep;23(2):389-396. 10.17998/jlc.2023.06.07.
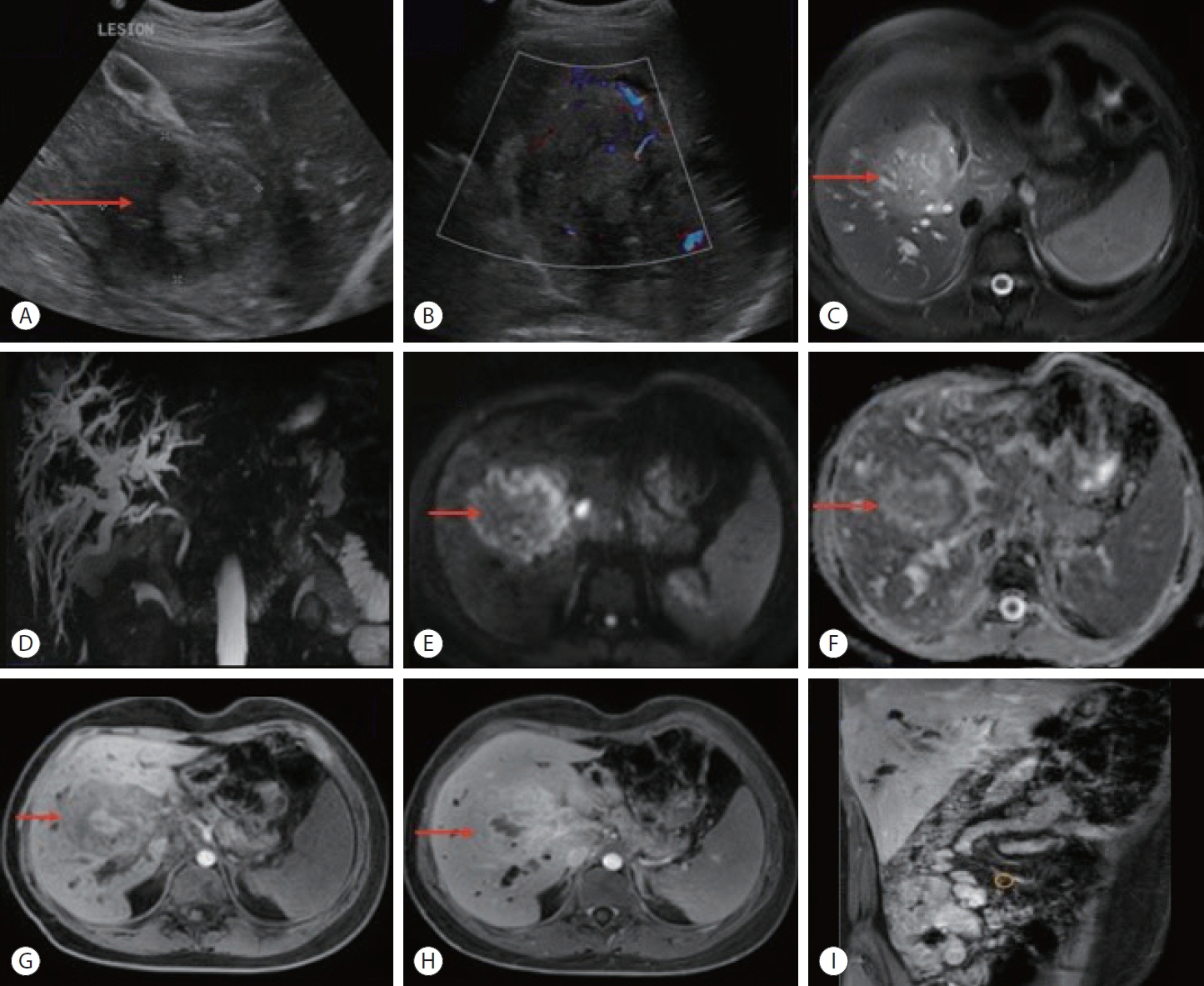
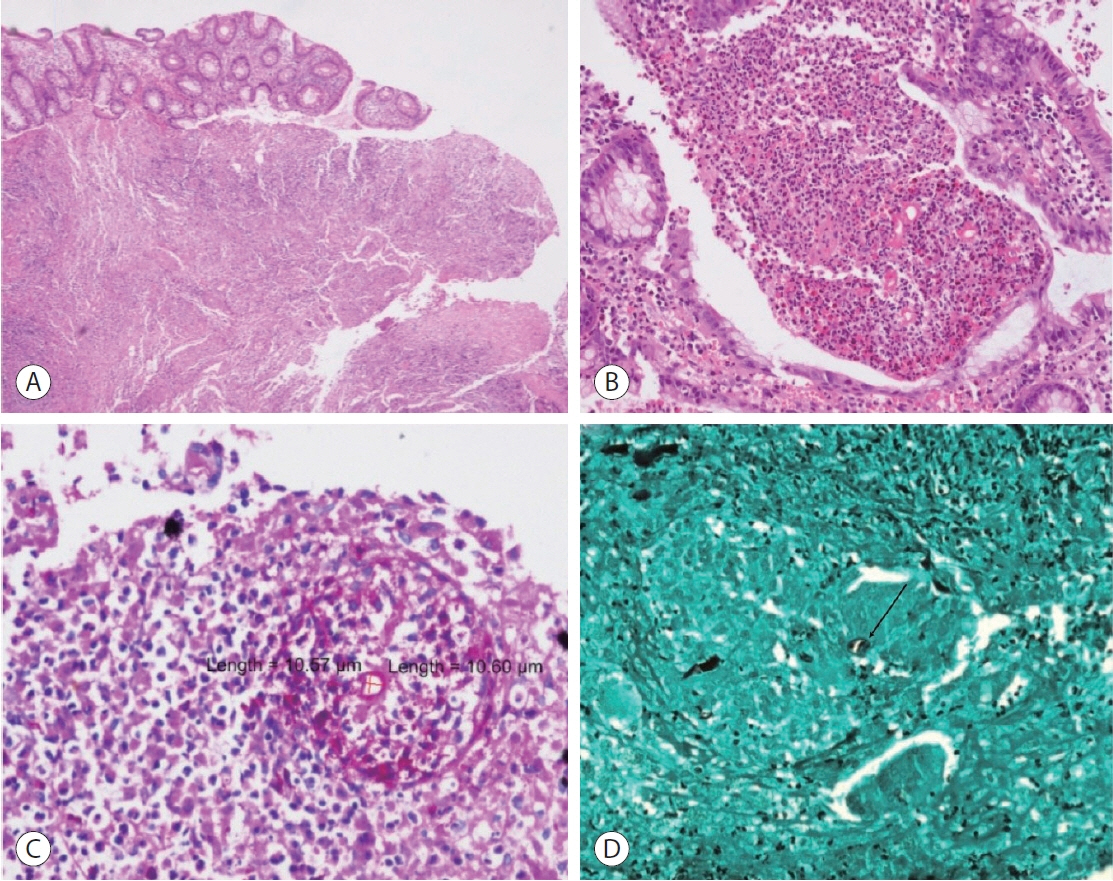
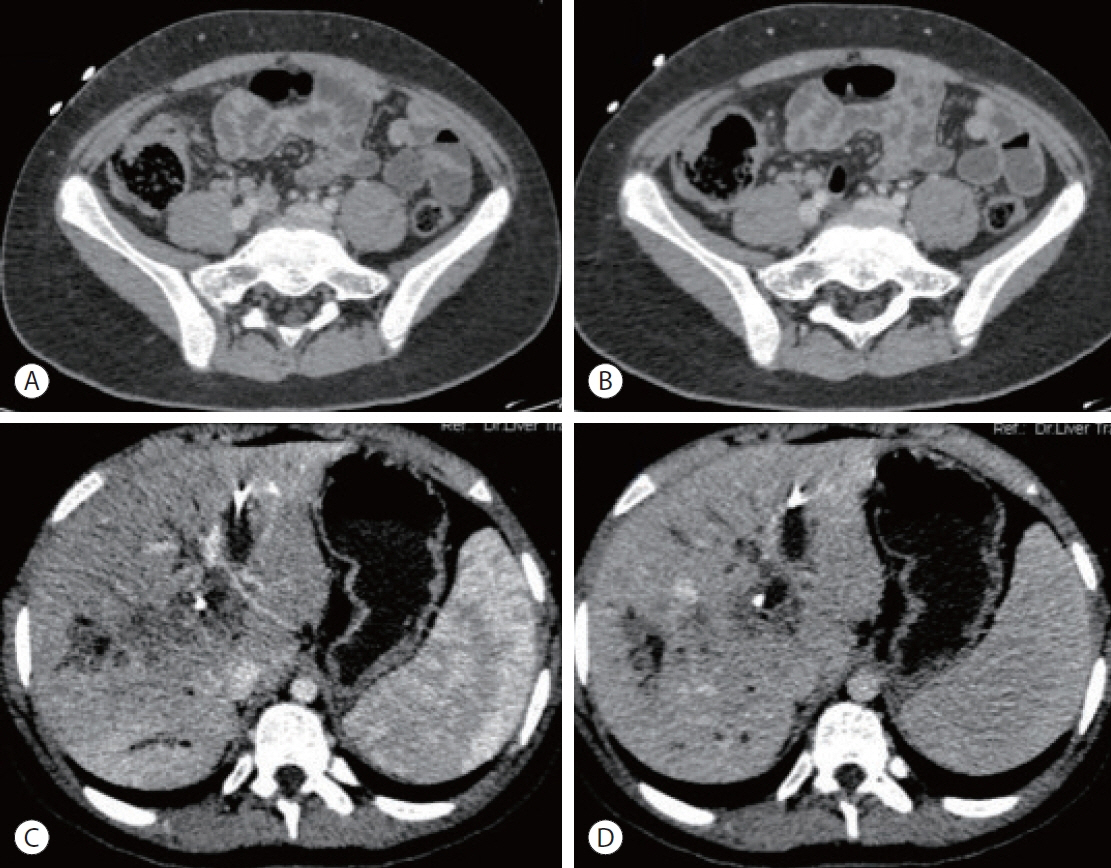
Hepatic basidiobolomycosis masquerading as cholangiocarcinoma: a case report and literature review
- Affiliations
-
- 1Department of Pathology, SGT University, Budhera, Gurugram, India
- 2Department of Liver Transplant Surgery, Aakash Healthcare Super Speciality Hospital, Dwarka, New Delhi, India
- 3Department of Nuclear Medicine & PET-CT, Fortis Memorial Research Institute (FMRI), Gurugram, India
- 4Department of Liver Transplant Surgery, Fortis Healthcare, Budhera, Gurugram, India
- KMID: 2546418
- DOI: http://doi.org/10.17998/jlc.2023.06.07
Abstract
- Basidiobolus ranarum is known to cause subcutaneous mycoses; however, rare cases of hepatic and gastrointestinal involvement by basidiobolomycosis have been reported. Hepatic basidiobolomycosis may be confused with a carcinoma on imaging, and histological examination and fungal culture can help distinguish between these two. We report a rare case of basidiobolomycosis in a 16-year-old male with liver and gastrointestinal involvement.
Keyword
Figure
Reference
-
References
1. Hussein MRA, Alqahtani AS, Alhagawi Y, Al Saglan NS, Albishi AM, Ahmed FO, et al. Primary basidiobolomycosis of the cecum in immunocompetent patients: two case reports. Gastroenterology Res. 2021; 14:116–124.2. Gugnani HC. A review of zygomycosis due to Basidiobolus ranarum. Eur J Epidemiol. 1999; 15:923–929.3. Lyon GM, Smilack JD, Komatsu KK, Pasha TM, Leighton JA, Guarner J, et al. Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literature. Clin Infect Dis. 2001; 32:1448–1455.4. Elzein F, Mursi M, Albarrag AM, Alfiaar A, Alzahrani A. Disseminated angioinvasive basidiobolomycosis with a favourable outcome. Med Mycol Case Rep. 2018; 22:30–34.5. Takrouni AO, Schammut MH, Al-Otaibi M, Al-Mulla M, Privitera A. Disseminated intestinal basidiobolomycosis with mycotic aneurysm mimicking obstructing colon cancer. BMJ Case Rep. 2019; 12:e225054.6. Gopinath D. Splendore-Hoeppli phenomenon. J Oral Maxillofac Pathol. 2018; 22:161–162.7. Abduh MS, Aldaqal SM, Almaghrabi J, Aljiffry MM, Elbadrawy HA, Alsahafi MA. A very rare basidiobolomycosis case presented with cecal perforation and concomitant hepatic involvement in an elderly male patient: a case study. Int J Environ Res Public Health. 2022; 19:3412.8. Jafarpour Z, Pouladfar G, Dehghan A, Anbardar MH, Foroutan HR. Case report: gastrointestinal basidiobolomycosis with multi-organ involvement presented with intussusception. Am J Trop Med Hyg. 2021; 105:1222–1226.9. Dashti AS, Nasimfar A, Khorami HH, Pouladfar G, Kadivar MR, Geramizadeh B, et al. Gastro-intestinal basidiobolomycosis in a 2-year-old boy: dramatic response to potassium iodide. Paediatr Int Child Health. 2018; 38:150–153.10. Zekavat OR, Abdolkarimi B, Pouladfar G, Fathpour G, Mokhtari M, Shakibazad N. Colonic basidiobolomycosis with liver involvement masquerading as gastrointestinal lymphoma: a case report and literature review. Rev Soc Bras Med Trop. 2017; 50:712–714.11. Geramizadeh B, Dashti AS, Kadivar MR, Kord S. Isolated hepatic basidiobolomycosis in a 2-year-old girl: the first case report. Hepat Mon. 2015; 15:e30117.12. Flicek KT, Vikram HR, De Petris GD, Johnson CD. Abdominal imaging findings in gastrointestinal basidiobolomycosis. Abdom Imaging. 2015; 40:246–250.13. Ejtehadi F, Anushiravani A, Bananzadeh A, Geramizadeh B. Gastrointestinal basidiobolomycosis accompanied by liver involvement: a case report. Iran Red Crescent Med J. 2014; 16:e14109.14. Saeed MA, Al Khuwaitir TS, Attia TH. Gastrointestinal basidiobolomycosis with hepatic dissemination: a case report. JMM Case Rep. 2014; 1:e003269.15. Hassan HA, Majid RA, Rashid NG, Nuradeen BE, Abdulkarim QH, Hawramy TA, et al. Eosinophilic granulomatous gastrointestinal and hepatic abscesses attributable to basidiobolomycosis and fasciolias: a simultaneous emergence in Iraqi Kurdistan. BMC Infect Dis. 2013; 13:91.16. Al-Shanafey S, AlRobean F, Bin Hussain I. Surgical management of gastrointestinal basidiobolomycosis in pediatric patients. J Pediatr Surg. 2012; 47:949–951.17. van den Berk GE, Noorduyn LA, van Ketel RJ, van Leeuwen J, Bemelman WA, Prins JM. A fatal pseudo-tumour: disseminated basidiobolomycosis. BMC Infect Dis. 2006; 6:140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary hepatic tuberculosis mimicking intrahepatic cholangiocarcinoma: report of two cases
- Intrahepatic Cholangiocarcinoma Initially Presented as a Distant Metastatic Lymph Node without Demonstrable Hepatic Mass: A Case Report
- Primary Cholangiocarcinoma of the Liver Presenting as a Complicated Hepatic Cyst: A Diagnostic Challenge
- Subcutaneous Basidiobolomycosis: A Rare and Underdiagnosed but Curable Fungal Infection -A Case Report
- MR Features of Common Hepatic Duct Cholangiocarcinoma