J Rheum Dis.
2023 Oct;30(4):260-267. 10.4078/jrd.2023.0032.
Hepatic steatosis index at diagnosis has the potential for forecasting end-stage kidney disease in patients with antineutrophil cytoplasmic antibody-associated vasculitis
- Affiliations
-
- 1Undergraduate Course, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Rheumatology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 4Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2546242
- DOI: http://doi.org/10.4078/jrd.2023.0032
Abstract
Objective
This study evaluated whether the hepatic steatosis index (HSI) at antineutrophil cytoplasmic antibody-associated vasculitis (AAV) diagnosis could forecast poor outcomes during the disease course in AAV patients.
Methods
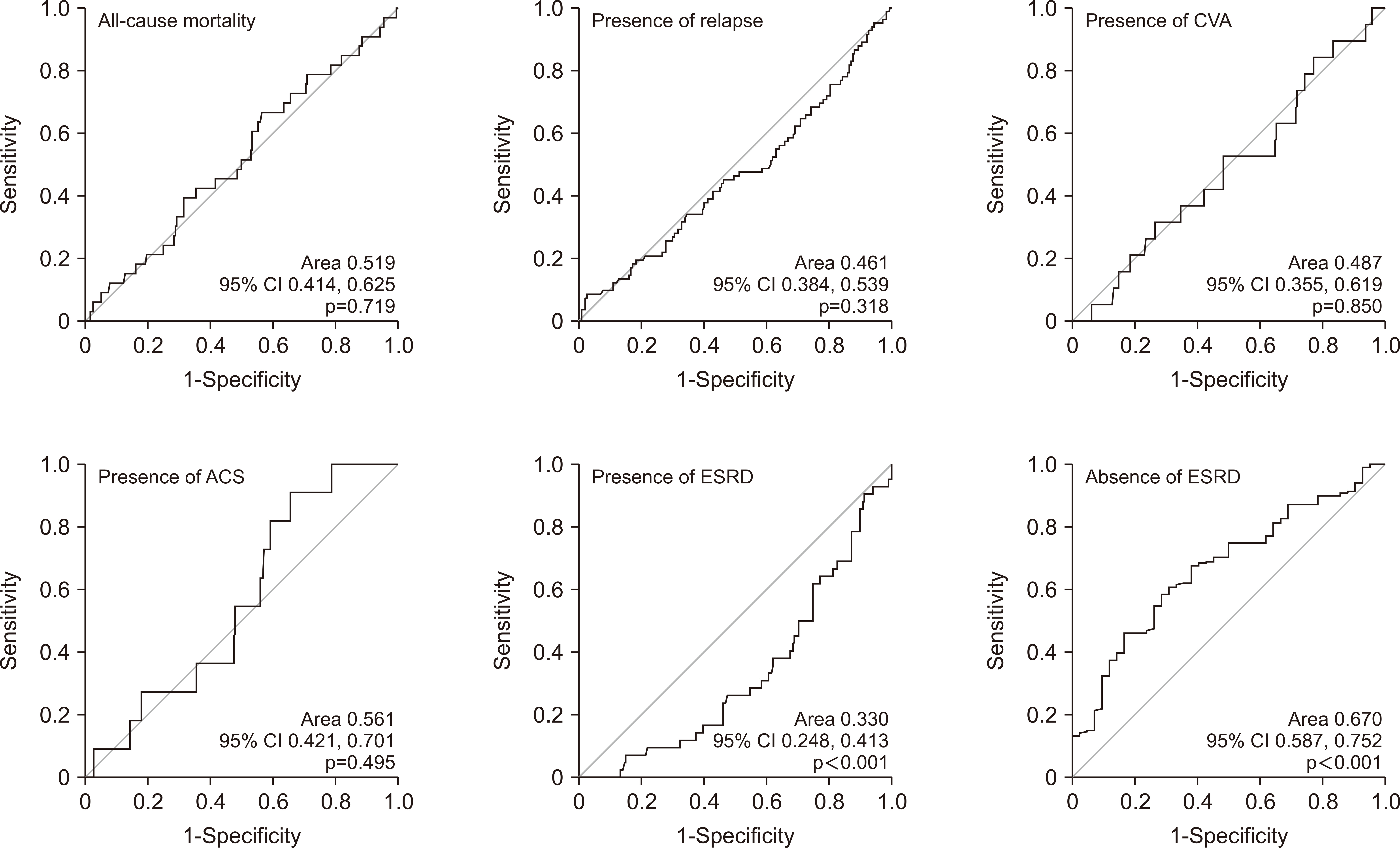
This study included 260 AAV patients. The equation for HSI is as follows: HSI=8×(alanine aminotransferase/aspartate aminotransferase)+body mass index+(2, diabetes mellitus)+(2, female). The cut-off of HSI was obtained using the receiver operating characteristic curve.
Results
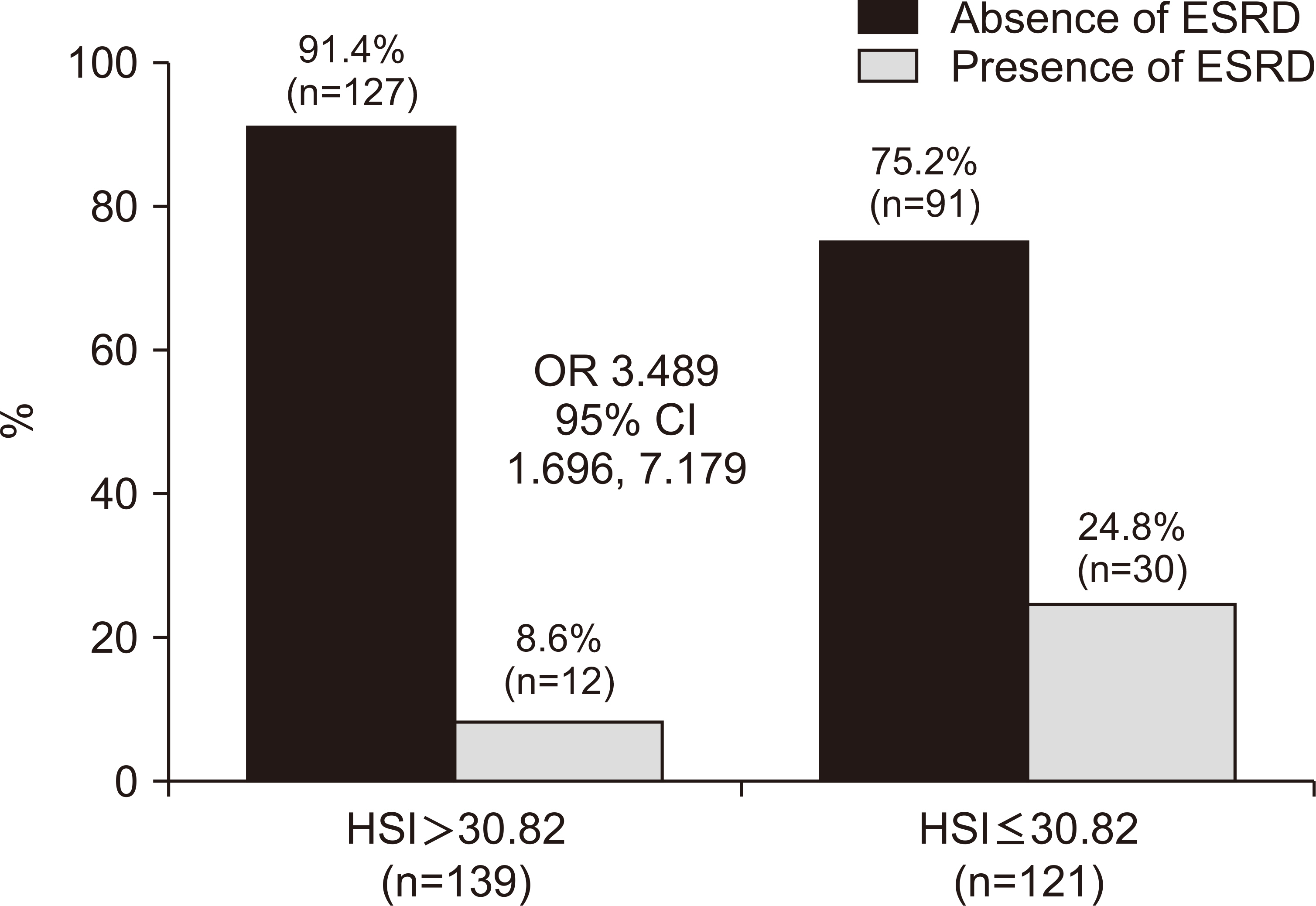
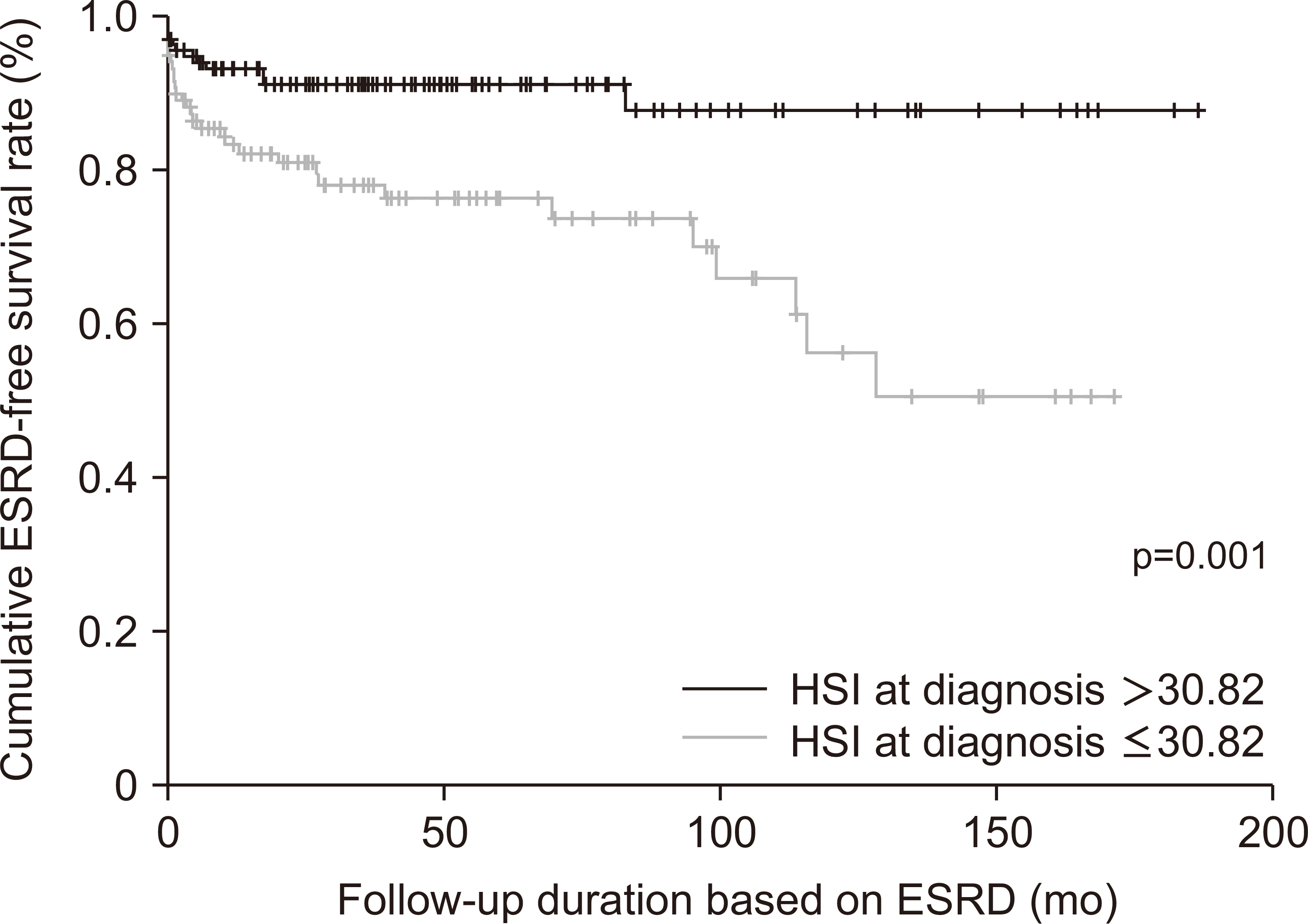
The median age of the 260 patients was 59.5 years, and 65.0% were female. Among the continuous variables excluding the parameters composing the equation for HSI, HSI was significantly correlated with Birmingham vasculitis activity score, fivefactor score, haemoglobin, blood urea nitrogen, serum creatinine, and total cholesterol. Among poor outcomes, the area under the curve of HSI for end-stage renal disease (ESRD) was significant, and the cut-off of HSI for ESRD was set at ≤30.82. AAV patients with HSI ≤30.82 exhibited a significantly higher risk of ESRD (relative risk 3.489) and a significantly lower cumulative ESRD-free survival rate than those with HSI >30.82.
Conclusion
This study is the first to demonstrate that HSI at AAV diagnosis could forecast ESRD during the disease course in AAV patients.
Keyword
Figure
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2013; 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 65:1–11. DOI: 10.1002/art.37715. PMID: 23045170.
Article2. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. 2007; Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 66:222–7. DOI: 10.1136/ard.2006.054593. PMID: 16901958. PMCID: PMC1798520.
Article3. Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. 2009; Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis. 68:1827–32. DOI: 10.1136/ard.2008.101279. PMID: 19054820.
Article4. Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Toumelin PL. French Vasculitis Study Group (FVSG). 2011; The Five-Factor Score revisited: assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore). 90:19–27. DOI: 10.1097/MD.0b013e318205a4c6. PMID: 21200183.5. Bhamra K, Luqmani R. 2012; Damage assessment in ANCA-associated vasculitis. Curr Rheumatol Rep. 14:494–500. DOI: 10.1007/s11926-012-0291-1. PMID: 22983618.
Article6. Willeke P, Schlüter B, Limani A, Becker H, Schotte H. 2016; Liver involvement in ANCA-associated vasculitis. Clin Rheumatol. 35:387–94. DOI: 10.1007/s10067-015-2882-5. PMID: 25633652.
Article7. Masiak A, Drobińska A, Zdrojewski Z. 2017; Hepatic involvement in granulomatosis with polyangiitis - diagnostic difficulties. Reumatologia. 55:318–22. DOI: 10.5114/reum.2017.72630. PMID: 29491541. PMCID: PMC5825971.
Article8. Lee SW, Kim DY, Ahn SH, Park YB, Han KH, Park JY. 2019; Subclinical but significant liver fibrosis in patients with ANCA-associated vasculitis. Clin Exp Rheumatol. 37 Suppl 117(2):26–31. PMID: 30325303.9. Pyo JY, Ahn SS, Lee LE, Choe HN, Song JJ, Park YB, et al. 2021; Efficacy of the fibrosis index for predicting end-stage renal disease in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Int J Clin Pract. 75:e13929. DOI: 10.1111/ijcp.13929. PMID: 33301633.
Article10. Pyo JY, Ahn SS, Lee LE, Choi GM, Song JJ, Park YB, et al. 2021; The novel fibrosis index at diagnosis may predict all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis without substantial liver diseases. Clinics (Sao Paulo). 76:e2501. DOI: 10.6061/clinics/2021/e2501. PMID: 33852653. PMCID: PMC8009064.
Article11. Kwon HC, Song JJ, Park YB, Lee SW. 2021; Fibrosis-5 predicts end-stage renal disease in patients with microscopic polyangiitis and granulomatosis with polyangiitis without substantial liver diseases. Clin Exp Med. 21:399–406. DOI: 10.1007/s10238-021-00691-2. PMID: 33611672. PMCID: PMC8266773.
Article12. Park HJ, Park JY, Jung SM, Song JJ, Park YB, Lee SW. 2019; Fibrosis-4 index at diagnosis is associated with all-cause mortality in patients with microscopic polyangiitis and granulomatosis with polyangiitis. BMC Gastroenterol. 19:90. DOI: 10.1186/s12876-019-1007-z. PMID: 31196158. PMCID: PMC6567497.
Article13. Xu L, Lu W, Li P, Shen F, Mi YQ, Fan JG. 2017; A comparison of hepatic steatosis index, controlled attenuation parameter and ultrasound as noninvasive diagnostic tools for steatosis in chronic hepatitis B. Dig Liver Dis. 49:910–7. DOI: 10.1016/j.dld.2017.03.013. PMID: 28433586.
Article14. Sviklāne L, Olmane E, Dzērve Z, Kupčs K, Pīrāgs V, Sokolovska J. 2018; Fatty liver index and hepatic steatosis index for prediction of non-alcoholic fatty liver disease in type 1 diabetes. J Gastroenterol Hepatol. 33:270–6. DOI: 10.1111/jgh.13814. PMID: 28464337.15. Wang C, Cai Z, Deng X, Li H, Zhao Z, Guo C, et al. 2021; Association of hepatic steatosis index and fatty liver index with carotid atherosclerosis in type 2 diabetes. Int J Med Sci. 18:3280–9. DOI: 10.7150/ijms.62010. PMID: 34400897. PMCID: PMC8364463.
Article16. Weng CH, Liu ZC. 2019; Drug-induced anti-neutrophil cytoplasmic antibody-associated vasculitis. Chin Med J (Engl). 132:2848–55. DOI: 10.1097/CM9.0000000000000539. PMID: 31856057. PMCID: PMC6940077.
Article17. McAdoo SP, Medjeral-Thomas N, Gopaluni S, Tanna A, Mansfield N, Galliford J, et al. 2019; Long-term follow-up of a combined rituximab and cyclophosphamide regimen in renal anti-neutrophil cytoplasm antibody-associated vasculitis. Nephrol Dial Transplant. 34:63–73. Erratum in: Nephrol Dial Transplant 2018;33:899. DOI: 10.1093/ndt/gfx378. PMID: 29462348. PMCID: PMC6322443.
Article18. Lee JH, Kim D, Kim HJ, Lee CH, Yang JI, Kim W, et al. 2010; Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 42:503–8. DOI: 10.1016/j.dld.2009.08.002. PMID: 19766548.
Article19. Musso G, Cassader M, Cohney S, De Michieli F, Pinach S, Saba F, et al. 2016; Fatty liver and chronic kidney disease: novel mechanistic insights and therapeutic opportunities. Diabetes Care. 39:1830–45. DOI: 10.2337/dc15-1182. PMID: 27660122.
Article20. Ochiai H, Shirasawa T, Yoshimoto T, Nagahama S, Sakamoto K, Azuma M, et al. 2021; Hepatic steatosis index and chronic kidney disease among middle-aged individuals: a large-scale study in Japan. Dis Markers. 2021:9941834. DOI: 10.1155/2021/9941834. PMID: 34211614. PMCID: PMC8211514.
Article21. Guo Q, Yu L, Zhang X, Shang J, Duan X. 2023; Analysis of the risk factors for end-stage renal disease and mortality in ANCA-associated vasculitis: a study from a single center of the Chinese Rheumatism Data Center. Clin Rheumatol. 42:489–99. DOI: 10.1007/s10067-022-06419-1. PMID: 36367596.
Article22. Toraman A, Soysal Gündüz Ö. 2021; Predictors of renal and patient outcomes in anti-neutrophil cytoplasmic antibody-associated vasculitis: our single-center, tertiary care experience. Arch Rheumatol. 36:445–57. DOI: 10.46497/ArchRheumatol.2021.8687. PMID: 34870177. PMCID: PMC8612491.
Article23. Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. 2023; Application of the 2022 ACR/EULAR criteria for microscopic polyangiitis to patients with previously diagnosed microscopic polyangiitis. Clin Exp Rheumatol. 41:792–9. DOI: 10.55563/clinexprheumatol/vmrk76. PMID: 35616581.
Article24. Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. 2023; Reclassification of previously diagnosed GPA patients using the 2022 ACR/EULAR classification criteria. Rheumatology (Oxford). 62:1179–86. DOI: 10.1093/rheumatology/keac267. PMID: 35512176.
Article25. Pyo JY, Ahn SS, Song JJ, Park YB, Lee SW. 2023; The reclassification of patients with previously diagnosed eosinophilic granulomatosis with polyangiitis based on the 2022 ACR/EULAR criteria for antineutrophil cytoplasmic antibody-associated vasculitis. J Rheumatol. 50:213–8. DOI: 10.3899/jrheum.220560. PMID: 36109070.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ANCA : The Marker Antibody of Vasculitis
- ANCA-Associated Vasculitis Presenting with Hypertrophic Pachymeningitis
- ANCA-Associated Vasculitic Neuropathy with Concurrent Pulmonary Tuberculosis
- Methimazole-Induced Anti-Neutrophil Cytoplasmic Antibody-Associated Vasculitis in the Peripheral Nerves
- A Case of Propylthiouracil-induced Lupus Erythematosus Accompanied by Antineutrophil Cytoplasmic Antibody-positive Vasculitis