J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):306-310. 10.7461/jcen.2023.E2022.06.005.
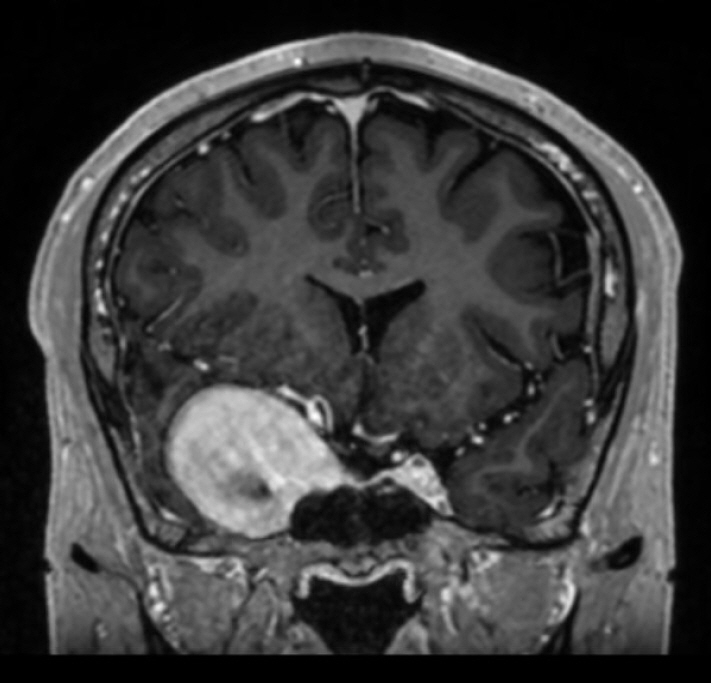
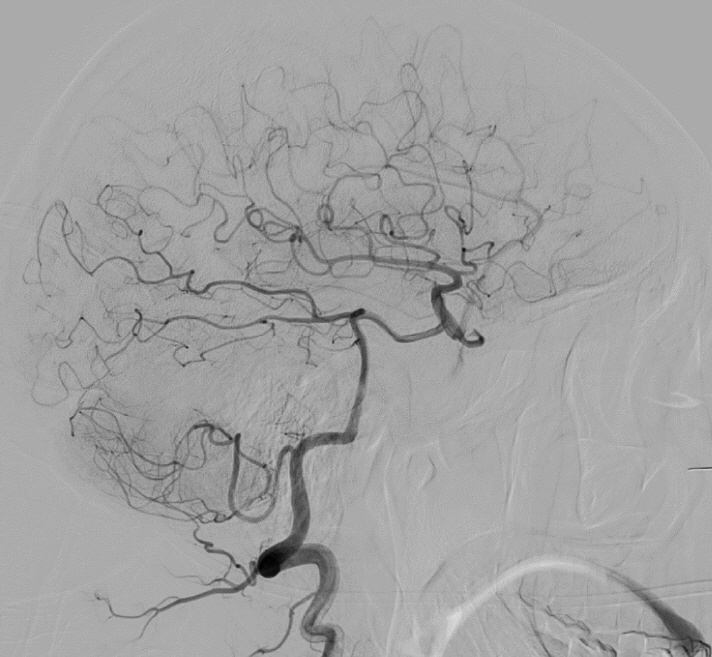
Parent artery occlusion of a giant internal carotid artery pseudoaneurysm-related direct carotid cavernous fistula: A case report
- Affiliations
-
- 1Department of Neurology, Beth Israel Deaconess Medical Center, Boston, MA 02215, USA
- 2Division of Neurosurgery, Beth Israel Deaconess Medical Center, Boston, MA 02215, USA
- KMID: 2546167
- DOI: http://doi.org/10.7461/jcen.2023.E2022.06.005
Abstract
- Traumatic internal carotid artery injuries can produce direct carotid-cavernous fistulas as well as giant internal carotid artery pseudoaneurysms. Clinical sequelae can include headaches, cranial nerves palsies, proptosis, chemosis and optic neuropathy with visual loss as the most dangerous complication. Herein, we present a case of one of the largest reported internal carotid artery pseudoaneurysms associated with a direct carotid cavernous fistula. We describe the techniques and pitfalls of treatment with parent vessel occlusion.
Figure
Reference
-
1. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985; Feb. 62(2):248–56.2. Choulakian A, Drazin D, Alexander MJ. Endosaccular treatment of 113 cavernous carotid artery aneurysms. J Neurointerv Surg. 2010; Dec. 2(4):359–62.3. Eliava SS, Filatov YM, Yakovlev SB, Shekhtman OD, Kheireddin AS, Sazonov IA, et al. Results of microsurgical treatment of large and giant ICA aneurysms using the retrograde suction decompression (RSD) technique: series of 92 patients. World Neurosurg. 2010; Jun. 73(6):683–7.4. Ghorbani M, Griessenauer CJ, Wipplinger C, Abdolhoseinpour H, Bahrami R, Asaadi S, et al. Combined endovascular and endoscopic approach for treatment of concomitant sphenoid sinus giant traumatic aneurysm and direct carotid cavernous fistulas. World Neurosurg. 2020; Feb. 134:211–4.5. Hauck EF, Welch BG, White JA, Replogle RE, Purdy PD, Pride LG, et al. Stent/coil treatment of very large and giant unruptured ophthalmic and cavernous aneurysms. Surg Neurol. 2009; Jan. 71(1):19–24. discussion 24.6. Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye (Lond. Engl.). 2018; Feb. 32(2):164–72.7. Hoffmann M. Isolated right temporal lobe stroke patients present with Geschwind Gastaut syndrome, frontal network syndrome and delusional misidentification syndromes. Behav Neurol. 2008; 20(3):83–9.8. Narayan DN, Jayprakash SV, Arjun D, Achal G. Coil embolisation of post traumatic giant supraclinoid pseudoaneurysm presenting as carotid cavernous fistula. Asian J Neurosurg. 2018; Oct-Dec. 13(4):1244–6.9. Ringer AJ, Salud L, Tomsick TA. Carotid cavernous fistulas: anatomy, classification, and treatment. Neurosurg Clin N Am. 2005; Apr. 16(2):279–95, viii.10. Thomas AJ, Chua M, Fusco M, Ogilvy CS, Tubbs RS, Harrigan MR, et al. Proposal of venous drainage-based classification system for carotid cavernous fistulae with validity assessment in a multicenter cohort. Neurosurgery. 2015; Sep. 77(3):380–5. discussion 385.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Spontaneous Thrombosis of Neglected Direct Carotid-Cavernous Fistula: A Case Report
- Spontaneous Regression of the Pseudoaneurysm Developed after Balloon Occlusion of the Direct Carotid-cavernous Fistula
- Direct Microsurgical Repair of Traumatic Carotid-Cavernous Fistula
- Treatment of carotid-carvenous fistula and internal carotid aneurysm with Latex detachable balloons
- Is the retrograde access for endovascular treatment of a traumatic carotid cavernous fistula associated with dissection of the ipsilateral carotid possible?