J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):260-266. 10.7461/jcen.2023.E2023.01.005.
A comparison study of vessel twisting by different microsurgical suture techniques in a chicken wing artery side to side bypass training model
- Affiliations
-
- 1Department of Neurosurgery, Hallym University Dongtan Sacred Heart Hospital, Hwasung, Korea
- 2Department of Neurosurgery, Danwon Hospital, Ansan, Korea
- KMID: 2546162
- DOI: http://doi.org/10.7461/jcen.2023.E2023.01.005
Abstract
Objective
Microvascular anastomosis, particularly side-to-side (STS) bypass, is a complex surgical procedure. While several suture techniques exist, none of them is superior to the others. We assessed the association between various STS bypass techniques and vessel twisting using chicken wing training models.
Methods
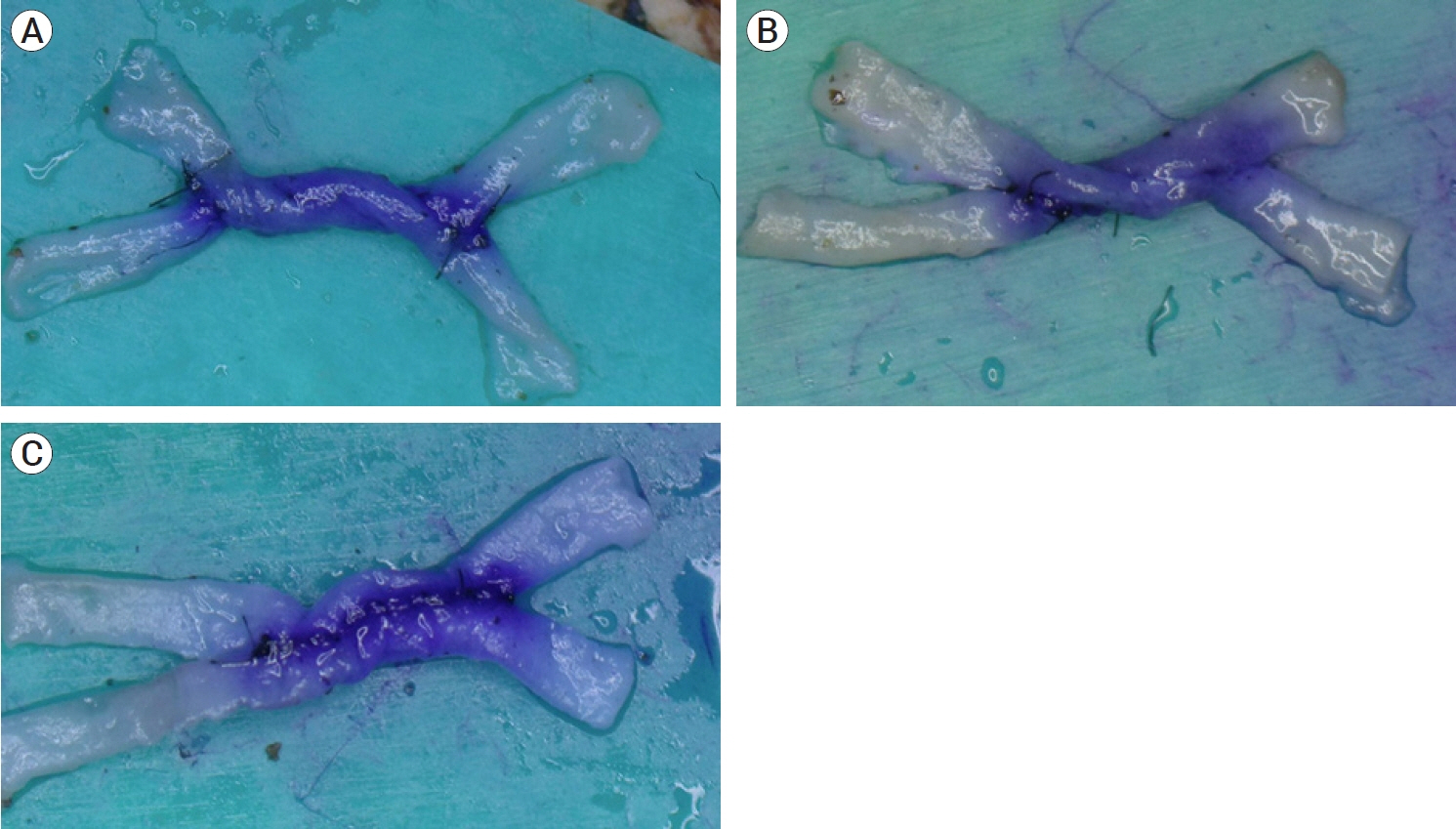
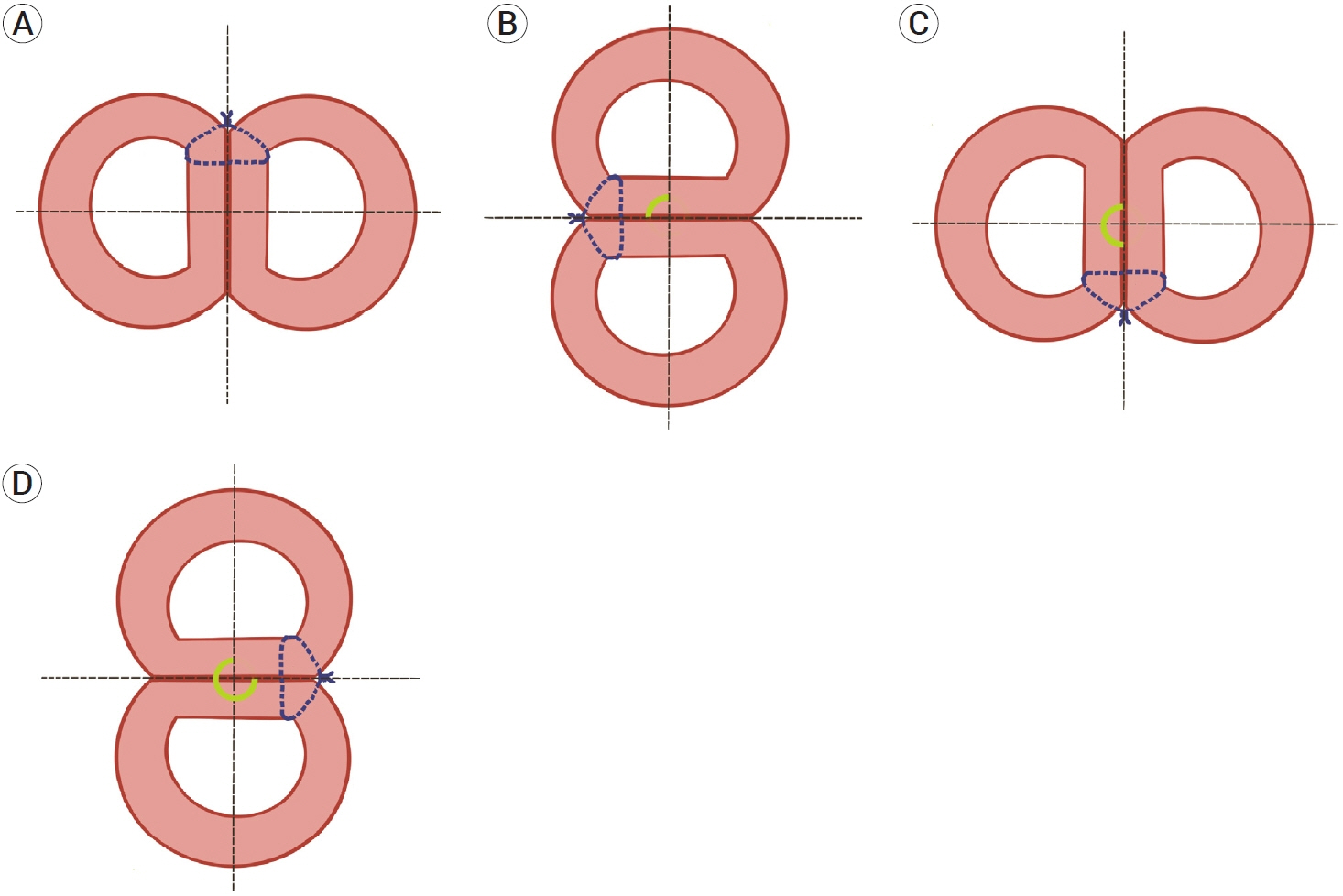
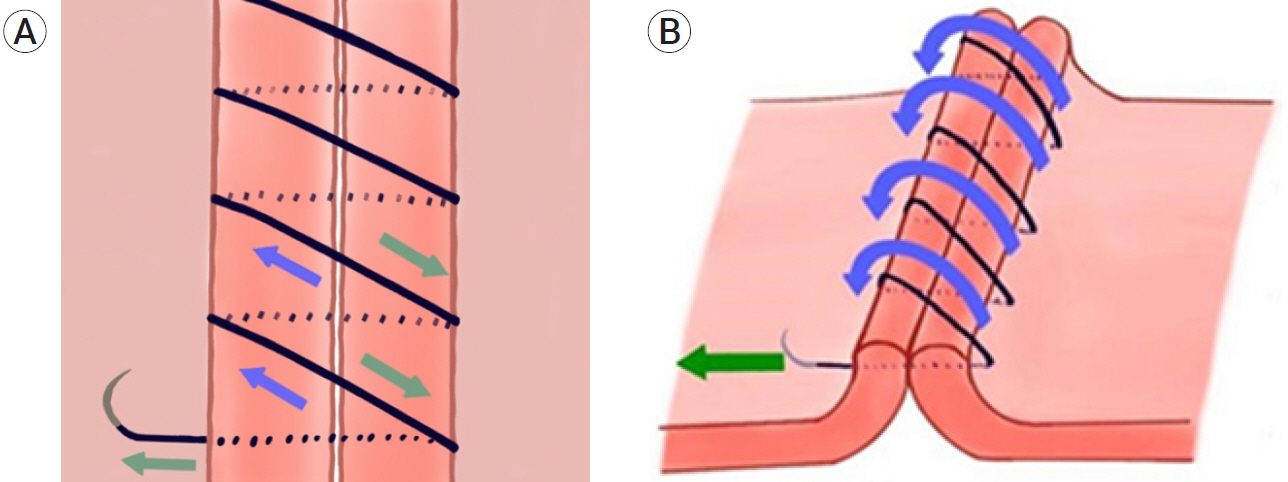
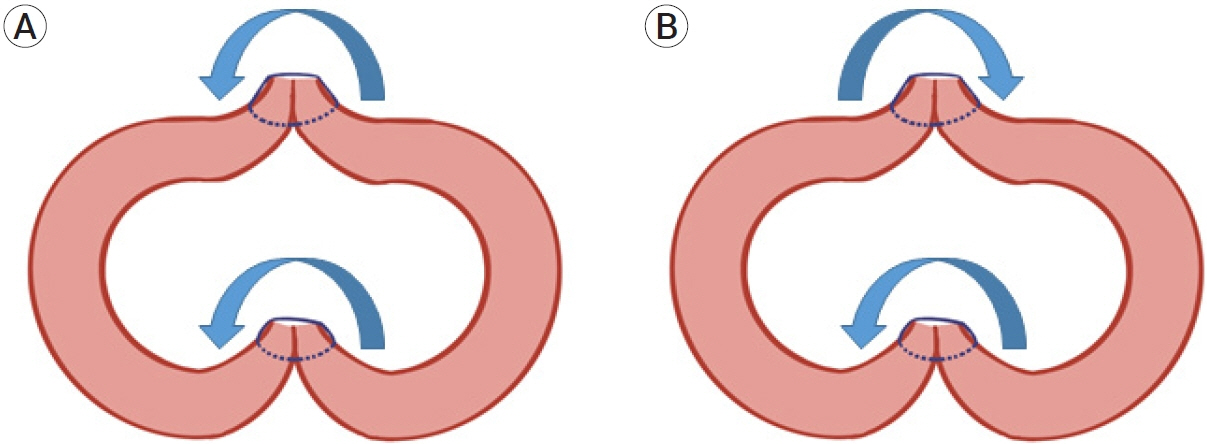
Three suture techniques were compared over an anterior wall suture procedure. The unidirectional continuous suture (UCS) group used a downward “right-to-left” continuous suture. The reverse continuous suture (RCS) group used a downward “left-to-right” continuous suture. The interrupted suture (IS) group used the standard interrupted suture. The number of samples in each of the three groups was 30 (n=90). We compared the incidence of vessel twisting and rotation angles across groups.
Results
Vessel twisting occurred in 96.7%, 56.7%, and 0% of the cases in the UCS, IS, and RCS groups, respectively. The incidence of vessel twisting differed significantly in all 3 groups (p<0.001), with an apparent trend (p=0.002). The mean rotation angles were 201˚±90.6˚, 102˚±107.6˚, and 0˚ in the UCS, IS, and RCS groups, respectively, which were significantly different (p<0.001). On excluding cases without twisting, the rotation angles of twisted vessels in the UCS and IS groups were 207.9˚±83.7˚ and 180˚±77.9˚, respectively, which yielded a significant difference between these groups (p<0.001).
Conclusions
We found that the incidence and trend of vessel twisting differed significantly across suture techniques. The RCS technique may aid in preventing vessel twisting in the STS bypass procedure.
Figure
Reference
-
1. Abla AA, Lawton MT. Anterior cerebral artery bypass for complex aneurysms: An experience with intracranial-intracranial reconstruction and review of bypass options. J Neurosurg. 2014; Jun. 120(6):1364–77.2. Au YK, Mahjoub SB, Hart JC. Suture patterns and corneal graft rotation in the cadaver eye. Ophthalmic Surg. 1990; Jul. 21(7):472–4.3. Bot GM, Zhao X, McElenney BK, Tayebi Meybodi A, Belykh E, Lawton MT, et al. Comparative analysis of continuous suturing, interrupted suturing, and cyanoacrylate-based lid techniques for end-to-end microvascular anastomosis: Laboratory investigation. World Neurosurg. 2020; Feb. 134:465–71.4. Chen YX, Chen LE, Seaber AV, Urbaniak JR. Comparison of continuous and interrupted suture techniques in microvascular anastomosis. J Hand Surg Am. 2001; May. 26(3):530–9.5. Grigore FN, Amin-Hanjani S. A3-A3 bypass surgery for aneurysm: Technical nuances. Oper Neurosurg (Hagerstown). 2019; Sep. 17(3):277–85.6. Hafez A, Huhtakangas J, Muhammad S, Lawton MT, Tanikawa R, Niemela M. The identification of factors that influence the quality of bypass anastomosis and an evaluation of the usefulness of an experimental practical scale in this regard. World Neurosurg. 2019; Jan. 121:e119–28.7. Hino A. Training in microvascular surgery using a chicken wing artery. Neurosurgery. 2003; Jun. 52(6):1495–7. discussion 1497.8. Kalani MY, Zabramski JM, Hu YC, Spetzler RF. Extracranial-intracranial bypass and vessel occlusion for the treatment of unclippable giant middle cerebral artery aneurysms. Neurosurgery. 2013; Mar. 72(3):428–35. discussion 435.9. Kalani MY, Zabramski JM, Nakaji P, Spetzler RF. Bypass and flow reduction for complex basilar and vertebrobasilar junction aneurysms. Neurosurgery. 2013; May. 72(5):763–75. discussion 775.10. Kawashima M, Rhoton AL Jr, Tanriover N, Ulm AJ, Yasuda A, Fujii K. Microsurgical anatomy of cerebral revascularization. Part I: Anterior circulation. J Neurosurg. 2005; Jan. 102(1):116–31.11. Kawashima M, Rhoton AL Jr, Tanriover N, Ulm AJ, Yasuda A, Fujii K. Microsurgical anatomy of cerebral revascularization. Part II: Posterior circulation. J Neurosurg. 2005; Jan. 102(1):132–47.12. Klein SR, Goldberg L, Miranda RM, Bosco P, Nelson RJ, White RA. Effect of suture technique on arterial anastomotic compliance. Arch Surg. 1982; Jan. 117(1):45–7.13. Lawton MT, Abla AA, Rutledge WC, Benet A, Zador Z, Rayz VL, et al. Bypass surgery for the treatment of dolichoectatic basilar trunk aneurysms: A work in progress. Neurosurgery. 2016; Jul. 79(1):83–99.14. Levi MA, Harb AA, Nicolas CF, Corvi JJ, Kozato A, Akelina Y, et al. Torsion is tolerated in arterial end to venous side anastomoses in the rat model. J Reconstr Microsurg. 2020; Sep. 36(7):501–6.15. Olabe J, Olabe J. Microsurgical training on an in vitro chicken wing infusion model. Surg Neurol. 2009; Dec. 72(6):695–9.16. Quinones-Hinojosa A, Lawton MT. In situ bypass in the management of complex intracranial aneurysms: Technique application in 13 patients. Neurosurgery. 2008; Jun. 62(6 Suppl 3):1442–9.17. Ramanathan D, Hegazy A, Mukherjee SK, Sekhar LN. Intracranial in situ side-to-side microvascular anastomosis: Principles, operative technique, and applications. World Neurosurg. 2010; Apr. 73(4):317–25.18. Rennert RC, Strickland BA, Radwanski RE, Ravina K, Chien M, Russin JJ. Running-to-interrupted microsuture technique for vascular bypass. Oper Neurosurg (Hagerstown). 2018; Oct. 15(4):412–7.19. Ryu J, Chung Y, Lee SH, Cho WS, Choi SK. In situ side-toside anastomosis: Surgical technique and complication avoidance. World Neurosurg. 2018; Feb. 110:336–44.20. Sanai N, Zador Z, Lawton MT. Bypass surgery for complex brain aneurysms: An assessment of intracranial-intracranial bypass. Neurosurgery. 2009; Oct. 65(4):670–83. discussion 683.21. Tayebi Meybodi A, Huang W, Benet A, Kola O, Lawton MT. Bypass surgery for complex middle cerebral artery aneurysms: An algorithmic approach to revascularization. J Neurosurg. 2017; Sep. 127(3):463–79.22. Terry MA, Li J, Goshe J, Davis-Boozer D. Endothelial keratoplasty: The relationship between donor tissue size and donor endothelial survival. Ophthalmology. 2011; Oct. 118(10):1944–9.23. Tiwari A, Cheng KS, Salacinski H, Hamilton G, Seifalian AM. Improving the patency of vascular bypass grafts: The role of suture materials and surgical techniques on reducing anastomotic compliance mismatch. Eur J Vasc Endovasc Surg. 2003; Apr. 25(4):287–95.24. Topalan M, Bilgin SS, Ip WY, Chow SP. Effect of torsion on microarterial anastomosis patency. Microsurgery. 2003; 23(1):56–9.25. Vajpayee RB, Sharma V, Sharma N, Panda A, Taylor HR. Evaluation of techniques of single continuous suturing in penetrating keratoplasty. Br J Ophthalmol. 2001; Feb. 85(2):134–8.26. Wang L, Cai L, Qian H, Lawton MT, Shi X. The in situ sideto-side bypass technique: A comprehensive review of the technical characteristics, current anastomosis approaches, and surgical experience. World Neurosurg. 2018; Jul. 115:357–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Training of Microanastomosis with Chicken Wing Brachial Artery
- An Efficient Microvascular Anastomosis Training Model Based on Chicken Wings and Simple Instruments
- Comparison of Different Microanastomosis Training Models : Model Accuracy and Practicality
- The Chicken Aorta as a Simulation-Training Model for Microvascular Surgery Training
- Simple Anastomotic Techniques for Coronary Artery Bypass Surgery in Patients with Small Coronary Arteries or a Marked Size Discrepancy Between the Coronary Artery and Graft