Clin Endosc.
2023 Sep;56(5):613-622. 10.5946/ce.2022.245.
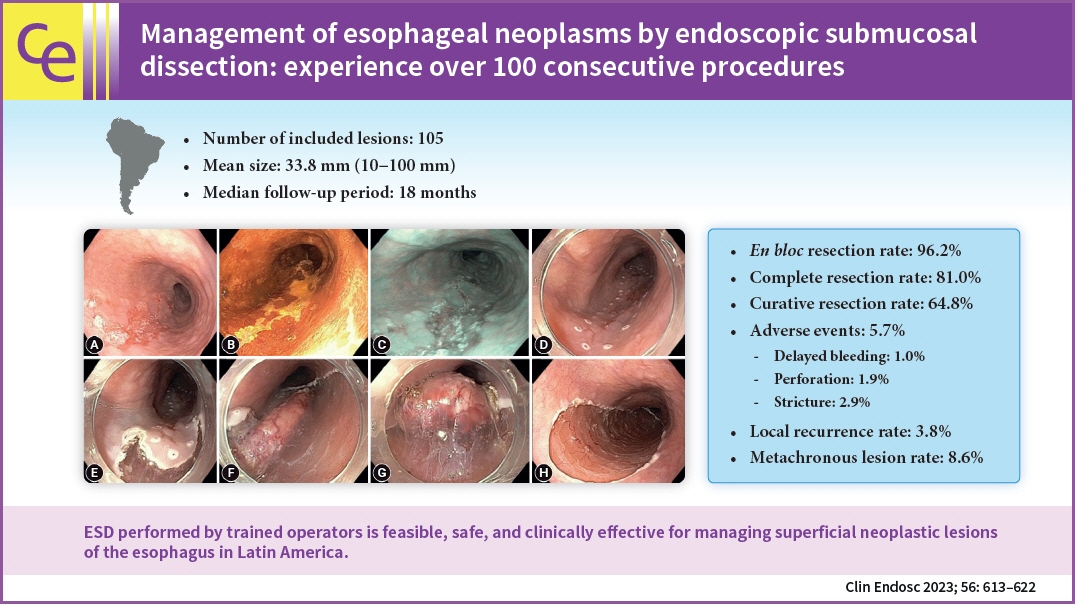
Management of esophageal neoplasms by endoscopic submucosal dissection: experience over 100 consecutive procedures
- Affiliations
-
- 1Department of Gastroenterology, “Jose Agurto Tello-Chosica” Hospital, Lima, Perú
- 2Digestive Endoscopy Unit of San Pablo Clinic, Lima, Perú
- 3Faculty of Medicine, Cayetano Heredia Peruvian University, Lima, Perú
- 4Department of Gastroenterology, Kobe University International Clinical Cancer Reserch Center, Kobe, Japan
- 5Endoscopy Unit, Alfa Institute of Gastroenterology, Belo Horizonte, Brazil
- 6Pathology Department, Alfa Institute of Gastroenterology, School of Medicine, Federal University of Minas Gerais, Laboratório CEAP, Belo Horizonte, Brazil
- 7Endoscopy Unit, Alfa Institute of Gastroenterology, School of Medicine, Federal University of Minas Gerais, Hospital Mater Dei Contorno, Belo Horizonte, Brazil
- KMID: 2546140
- DOI: http://doi.org/10.5946/ce.2022.245
Abstract
- Background/Aims
Endoscopic submucosal dissection (ESD) is currently considered the first-line treatment for the eradication of superficial neoplasms of the esophagus in Eastern countries. However, in the West, particularly in Latin America, the experience with esophageal ESD is still limited because of the high technical complexity required for its execution. This study aimed to present the results of the clinical application of ESD to manage superficial esophageal neoplasms in a Latin American center in over 100 consecutive cases.
Methods
This retrospective study included consecutive patients who underwent endoscopic ESD for superficial esophageal neoplasms between 2009 and 2022. The following clinical outcomes were assessed: en bloc, complete, and curative resection rates, local recurrence, adverse events, and procedure-related mortality.
Results
Esophageal ESD was performed mainly for squamous cell carcinoma (66.6%), high-grade intraepithelial neoplasia (17.1%), and adenocarcinoma (11.4%). En bloc and complete resection rates were 96.2% and 81.0%, respectively. The curative resection rate was 64.8%. Adverse events occurred in six cases (5.7%). Endoscopic follow-up was performed for an average period of 29.7 months.
Conclusions
ESD performed by trained operators is feasible, safe, and clinically effective for managing superficial neoplastic lesions of the esophagus in Latin America.
Figure
Reference
-
1. Arnold M, Soerjomataram I, Ferlay J, et al. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015; 64:381–387.2. Pimentel-Nunes P, Libânio D, Bastiaansen BA, et al. Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline: update 2022. Endoscopy. 2022; 54:591–622.3. Matsueda K, Ishihara R. Preoperative diagnosis and indications for endoscopic resection of superficial esophageal squamous cell carcinoma. J Clin Med. 2020; 10:13.4. Aliaga Ramos J, Arantes V, Abdul Rani R, et al. Off-label use of 0.4 % sodium hyaluronate teardrops: a safe and effective solution for submucosal injection in gastric endoscopic submucosal dissection. Endosc Int Open. 2020; 8:E1741–E1747.5. Kawata N, Tanaka M, Kakushima N, et al. The low incidence of bacteremia after esophageal endoscopic submucosal dissection (ESD) obviates the need for prophylactic antibiotics in esophageal ESD. Surg Endosc. 2016; 30:5084–5090.6. Arantes V, Aliaga Ramos J, Richard White J, Parra-Blanco A. Clinical effectiveness of short course oral prednisone for stricture prevention after semi circumferential esophageal endoscopic submucosal dissection. Endosc Int Open. 2022; 10:E753–E761.7. Kim SJ, Kim GH, Lee MW, et al. New magnifying endoscopic classification for superficial esophageal squamous cell carcinoma. World J Gastroenterol. 2017; 23:4416–4421.8. Ishihara R, Arima M, Iizuka T, et al. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig Endosc. 2020; 32:452–493.9. Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 1. Esophagus. 2019; 16:1–24.10. Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 2. Esophagus. 2019; 16:25–43.11. Suzuki T, Furukawa K, Funasaka K, et al. Long-term prognostic predictors of esophageal squamous cell carcinoma potentially indicated for endoscopic submucosal dissection. Digestion. 2021; 102:563–571.12. Mizumoto T, Hiyama T, Oka S, et al. Diagnosis of superficial esophageal squamous cell carcinoma invasion depth before endoscopic submucosal dissection. Dis Esophagus. 2018; 31:dox142.13. Oyama T, Inoue H, Arima M, et al. Prediction of the invasion depth of superficial squamous cell carcinoma based on microvessel morphology: magnifying endoscopic classification of the Japan Esophageal Society. Esophagus. 2017; 14:105–112.14. Sgourakis G, Gockel I, Lang H. Endoscopic and surgical resection of T1a/T1b esophageal neoplasms: a systematic review. World J Gastroenterol. 2013; 19:1424–1437.15. Kawashima K, Abe S, Koga M, et al. Optimal selection of endoscopic resection in patients with esophageal squamous cell carcinoma: endoscopic mucosal resection versus endoscopic submucosal dissection according to lesion size. Dis Esophagus. 2021; 34:doaa096.16. Min YW, Lee H, Song BG, et al. Comparison of endoscopic submucosal dissection and surgery for superficial esophageal squamous cell carcinoma: a propensity score-matched analysis. Gastrointest Endosc. 2018; 88:624–633.17. Tsou YK, Chuang WY, Liu CY, et al. Learning curve for endoscopic submucosal dissection of esophageal neoplasms. Dis Esophagus. 2016; 29:544–550.18. Berger A, Rahmi G, Perrod G, et al. Long-term follow-up after endoscopic resection for superficial esophageal squamous cell carcinoma: a multicenter Western study. Endoscopy. 2019; 51:298–306.19. Lorenzo D, Barret M, Leblanc S, et al. Outcomes of endoscopic submucosal dissection for early oesophageal squamous cell neoplasia at a Western centre. United European Gastroenterol J. 2019; 7:1084–1092.20. Repici A, Hassan C, Carlino A, et al. Endoscopic submucosal dissection in patients with early esophageal squamous cell carcinoma: results from a prospective Western series. Gastrointest Endosc. 2010; 71:715–721.21. Arantes V, Albuquerque W, Freitas Dias CA, et al. Standardized endoscopic submucosal tunnel dissection for management of early esophageal tumors (with video). Gastrointest Endosc. 2013; 78:946–952.22. Xu W, Liu XB, Li SB, et al. Prediction of lymph node metastasis in superficial esophageal squamous cell carcinoma in Asia: a systematic review and meta-analysis. Dis Esophagus. 2020; 33:doaa032.23. Ye B, Zhang X, Su Y, et al. The possibility of endoscopic treatment of cN0 submucosal esophageal cancer: results from a surgical cohort. Surg Endosc. 2021; 35:593–601.24. Manner H, Pech O, Heldmann Y, et al. The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc. 2015; 29:1888–1896.25. Ribeiro TM, Arantes VN, Ramos JA, et al. Endoscopic submucosal dissection with circumferential incision versus tunneling method for treatment of superficial esophageal cancer. Arq Gastroenterol. 2021; 58:195–201.26. Furue Y, Katada C, Tanabe S, et al. Effectiveness and safety of endoscopic aspiration mucosectomy and endoscopic submucosal dissection in patients with superficial esophageal squamous-cell carcinoma. Surg Endosc. 2019; 33:1433–1440.27. Tsujii Y, Nishida T, Nishiyama O, et al. Clinical outcomes of endoscopic submucosal dissection for superficial esophageal neoplasms: a multicenter retrospective cohort study. Endoscopy. 2015; 47:775–783.28. Yamashina T, Ishihara R, Uedo N, et al. Safety and curative ability of endoscopic submucosal dissection for superficial esophageal cancers at least 50 mm in diameter. Dig Endosc. 2012; 24:220–225.29. Park JS, Youn YH, Park JJ, et al. Clinical outcomes of endoscopic submucosal dissection for superficial esophageal squamous neoplasms. Clin Endosc. 2016; 49:168–175.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Endoscopic Treatment for Esophageal Cancer
- Endoscopic Submucosal Dissection for Esophageal Squamous Cell Carcinoma
- Endoscopic Submucosal Dissection Followed by Concurrent Chemoradiotherapy in Patients with Early Esophageal Cancer with a High Risk of Lymph Node Metastasis
- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia