Ann Surg Treat Res.
2023 Sep;105(3):141-147. 10.4174/astr.2023.105.3.141.
Ventilator support in the pretransplant period predisposes early graft failure after deceased donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Veterans Health Service Medical Center, Seoul, Korea
- 2Organ Transplant Center, Samsung Medical Center, Seoul, Korea
- 3Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- KMID: 2545905
- DOI: http://doi.org/10.4174/astr.2023.105.3.141
Abstract
- Purpose
Deceased donor liver transplantation (DDLT) recipients in Korea are generally sicker due to an increasing organ shortage. In the present study, the risk factors for early 30-day liver graft failure after DDLT were identified.
Methods
From August 2017 to February 2021, 265 adult DDLTs were performed. The characteristics of patients with and without 30-day graft failure were compared.
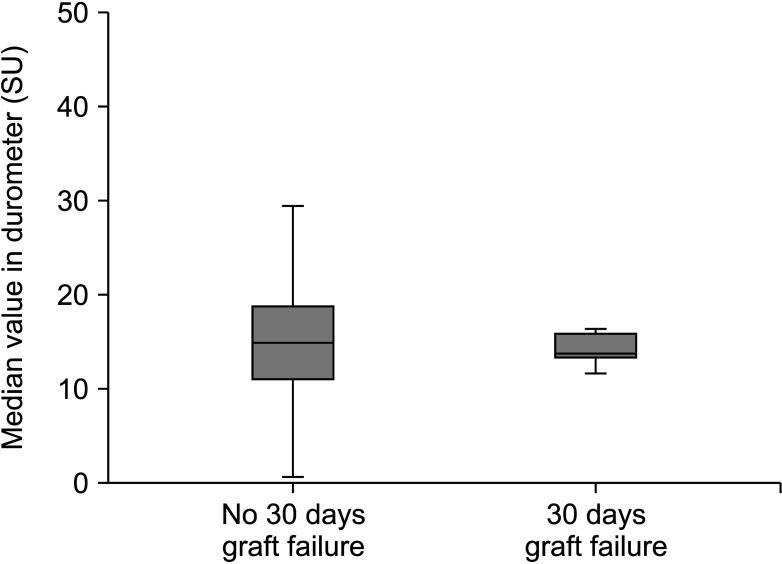
Results
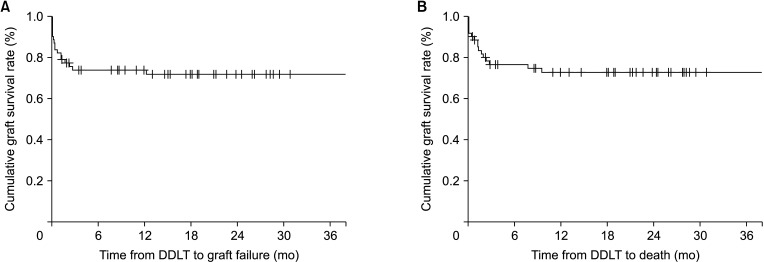
Liver graft failure occurred in 11 patients (17.7%) after DDLT. Baseline and perioperative characteristics of donors and recipients were not statistically significantly different between the 2 groups. The cumulative graft and overall survival rates at 6 months were 83.9% and 88.7%, respectively. Multivariate analysis showed ventilator support in the pretransplant period was a predisposing factor for 30-day graft failure after DDLT.
Conclusion
Present study indicates that cautious decision is required when allocating DDLT in critically ill patients on mechanical ventilatory support.
Keyword
Figure
Reference
-
1. Findlay JY, Fix OK, Paugam-Burtz C, Liu L, Sood P, Tomlanovich SJ, et al. Critical care of the end-stage liver disease patient awaiting liver transplantation. Liver Transpl. 2011; 17:496–510. PMID: 21506240.
Article2. Dirchwolf M, Becchetti C, Stampf S, Haldimann C, Immer F, Beyeler F, et al. The impact of perceived donor liver quality on post-transplant outcome. ANZ J Surg. 2023; 93:918–925. PMID: 36708059.
Article3. Chung YK, Park CS, Kang SH. Association between institutional liver transplantation cases volume and mortality: a meta-analysis of Korea-nationwide cohort studies using Korean National Healthcare Insurance Service database. Ann Liver Transplant. 2022; 2:8–14.
Article4. Flores A, Asrani SK. The donor risk index: A decade of experience. Liver Transpl. 2017; 23:1216–1225. PMID: 28590542.
Article5. Kim MS. Modification of emergency status in deceased donor liver allocation: evidence for Korean model of end-stage liver disease (MELD) system. J Korean Soc Transplant. 2016; 30:51–58.
Article6. Ha HS, Hong JJ, Kim IO, Lee SR, Lee AY, Ha TY, et al. Deceased donor liver transplantation under the Korean model for end-stage liver disease score-based liver allocation system: 2-year allocation results at a high-volume transplantation center. Korean J Transplant. 2019; 33:112–117. PMID: 35769978.
Article7. Gil E, Kim JM, Jeon K, Park H, Kang D, Cho J, et al. Recipient age and mortality after liver transplantation: a population-based cohort study. Transplantation. 2018; 102:2025–2032. PMID: 30153223.
Article8. Diaz-Nieto R, Lykoudis P, Robertson F, Sharma D, Moore K, Malago M, et al. A simple scoring model for predicting early graft failure and postoperative mortality after liver transplantation. Ann Hepatol. 2019; 18:902–912. PMID: 31405576.
Article9. Masior Ł, Grąt M. Primary nonfunction and early allograft dysfunction after liver transplantation. Dig Dis. 2022; 40:766–776. PMID: 35114676.
Article10. Bolondi G, Mocchegiani F, Montalti R, Nicolini D, Vivarelli M, De Pietri L. Predictive factors of short term outcome after liver transplantation: a review. World J Gastroenterol. 2016; 22:5936–5949. PMID: 27468188.
Article11. Markmann JF, Markmann JW, Markmann DA, Bacquerizo A, Singer J, Holt CD, et al. Preoperative factors associated with outcome and their impact on resource use in 1148 consecutive primary liver transplants. Transplantation. 2001; 72:1113–1122. PMID: 11579310.
Article12. Asrani SK, Saracino G, O'Leary JG, Gonzalez S, Kim PT, McKenna GJ, et al. Recipient characteristics and morbidity and mortality after liver transplantation. J Hepatol. 2018; 69:43–50. PMID: 29454069.
Article13. Huang CT, Lin HC, Chang SC, Lee WC. Pre-operative risk factors predict post-operative respiratory failure after liver transplantation. PLoS One. 2011; 6:e22689. PMID: 21829646.
Article14. Smetana GW, Lawrence VA, Cornell JE. American College of Physicians. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006; 144:581–595. PMID: 16618956.
Article15. Neviere R, Edme JL, Montaigne D, Boleslawski E, Pruvot FR, Dharancy S. Prognostic implications of preoperative aerobic capacity and exercise oscillatory ventilation after liver transplantation. Am J Transplant. 2014; 14:88–95. PMID: 24354872.
Article16. Yoon YC, Lee JS, Park SU, Kwon JH, Hong TH, Kim DG. Quantitative assessment of liver fibrosis using shore durometer. Ann Surg Treat Res. 2017; 93:300–304. PMID: 29250508.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventilator support in pretransplant predisposes early graft failure after deceased donor liver transplantation
- Prognostic impact of MELD scores greater than 40 in deceased donor liver transplant recipients
- Liver retransplantation for adult recipients
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Experience of split liver transplantation from deceased marginal donor: eight adult recipients from four deceased donors