Obstet Gynecol Sci.
2023 Sep;66(5):459-461. 10.5468/ogs.23029.
The application of pringle manoeuvre, type three liver mobilisation, full thickness diaphragmatic resection with primary closure technique and peritonectomy in the management of advanced ovarian malignancy
- Affiliations
-
- 1Department of Gynaecological Oncology, Churchill Cancer Centre, Oxford University Hospitals NHS Foundation Trust, Oxford, UK
- KMID: 2545894
- DOI: http://doi.org/10.5468/ogs.23029
Abstract
Objective
We present an educational technique for the safe completion of complete cytoreduction of diaphragmatic disease for the management of advanced ovarian malignancy.
Methods
We demonstrated these steps with attention to anatomical landmarks and surgical approaches, considering intraoperative and postoperative morbidity and mortality.
Results
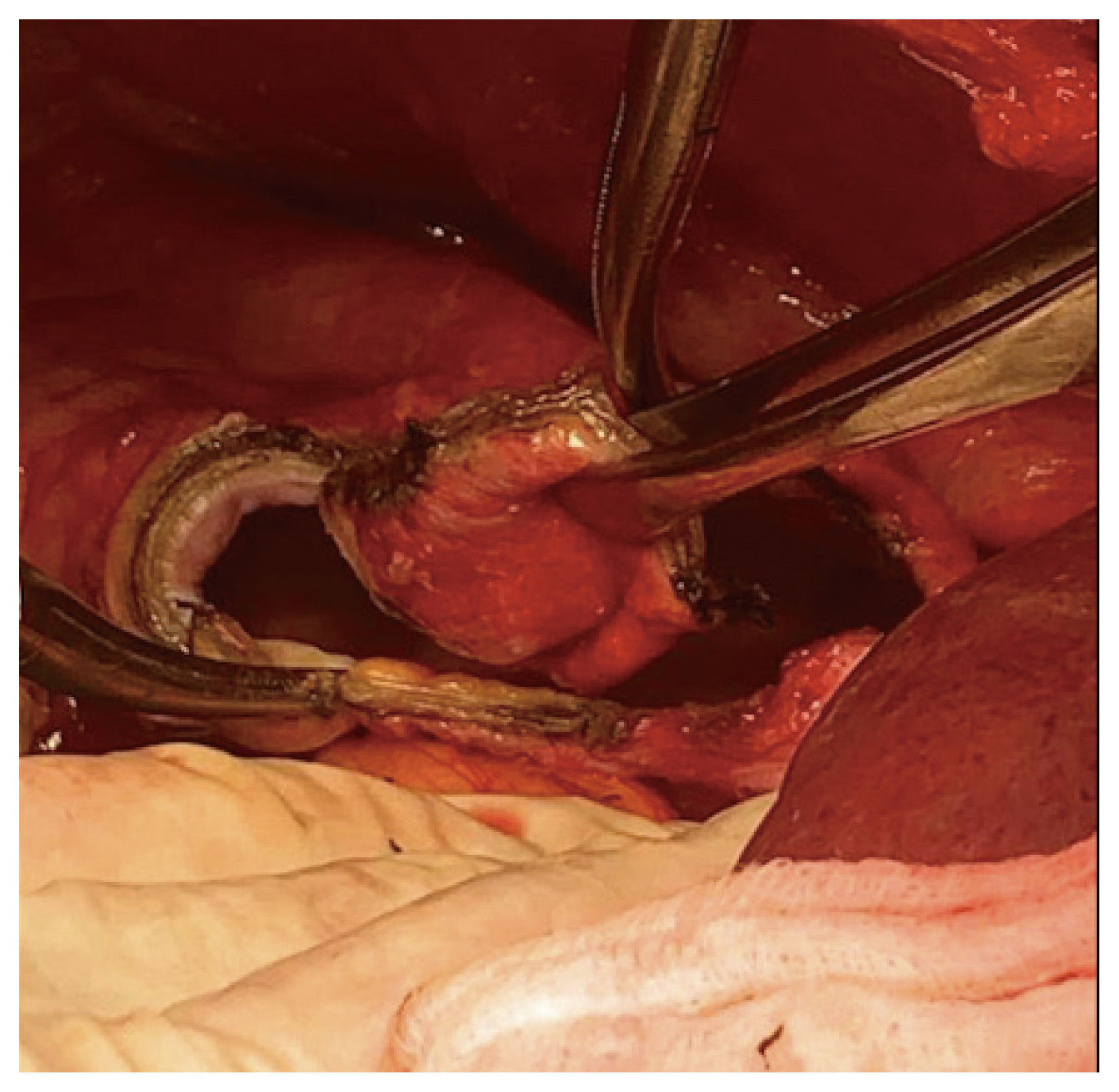
We present the case of a 49-year-old female patient diagnosed with suspected stage 3C ovarian malignancy following diagnostic laparoscopy. We demonstrate the surgical application of the Pringle manoeuvre, type 3 liver mobilisation, and full-thickness diaphragmatic resection. This was completed with a primary closure technique, with integrity ensured through the performance of an air test and Valsalva manoeuvre. Final histology confirmed a serous borderline tumour with invasive implants within a port site nodule (stage 4A).
Conclusion
This technique affirms the essential skills in gynaecological oncology training and details a challenging case requiring advanced surgical skills and knowledge, with specific consideration for intraoperative multidisciplinary decision-making.
Keyword
Figure
Reference
-
References
1. Buruiana FE, Ismail L, Ferrari F, Majd HS. The role of ultra-radical surgery in the management of advanced ovarian cancer: state of the art [Internet]. London: IntechOpen;c2021. [cited 2022 Aug 3]. Available from: https://www.intechopen.com/chapters/78061 .2. Tozzi R, Traill Z, Garruto Campanile R, Ferrari F, Soleymani Majd H, Nieuwstad J, et al. Porta hepatis peritonectomy and hepato-celiac lymphadenectomy in patients with stage IIIC-IV ovarian cancer: diagnostic pathway, surgical technique and outcomes. Gynecol Oncol. 2016; 143:35–9.3. Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N Engl J Med. 2019; 380:822–32.4. Soleymani Majd H, Ferrari F, Manek S, Gubbala K, Campanile RG, Hardern K, et al. Diaphragmatic peritonectomy vs. full thickness resection with pleurectomy during visceral-peritoneal debulking (VPD) in 100 consecutive patients with stage IIIC-IV ovarian cancer: a surgical-histological analysis. Gynecol Oncol. 2016; 140:430–5.5. Addley S, Yao DS, Soleymani Majd H. Primary diaphragmatic closure following diaphragmatic resection and cardiophrenic lymph node dissection during interval debulking surgery for advanced ovarian malignancy. Gynecol Oncol Rep. 2021; 36:100744.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feasibility of laparoscopic diaphragmatic peritonectomy during Visceral-Peritoneal Debulking (VPD) in patients with stage IIIC-IV ovarian cancer
- Tozzi classification of diaphragmatic surgery in patients with stage IIIC–IV ovarian cancer based on surgical findings and complexity
- Reconstruction of the diaphragm with autologous fascia lata during cytoreduction in patients with advanced ovarian cancer
- Repair of diaphragmatic injury and placement of tube thoracostomy during right upper quadrant peritonectomy
- Maximal cytoreductive effort in epithelial ovarian cancer surgery