J Korean Assoc Oral Maxillofac Surg.
2023 Aug;49(4):192-197. 10.5125/jkaoms.2023.49.4.192.
Radiographic evaluation before surgical extraction of impacted third molar to reduce the maxillary sinus related complication
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- KMID: 2545584
- DOI: http://doi.org/10.5125/jkaoms.2023.49.4.192
Abstract
Objectives
Surgical extraction of maxillary third molars is routine in departments devoted to oral and maxillofacial surgery. Because maxillary third molars are anatomically adjacent to the maxillary sinus, complications such as oroantral fistula and maxillary sinusitis can occur. Here we explore the factors that can cause radiographic postoperative swelling of the maxillary sinus mucosa after surgical extraction.
Materials and Methods
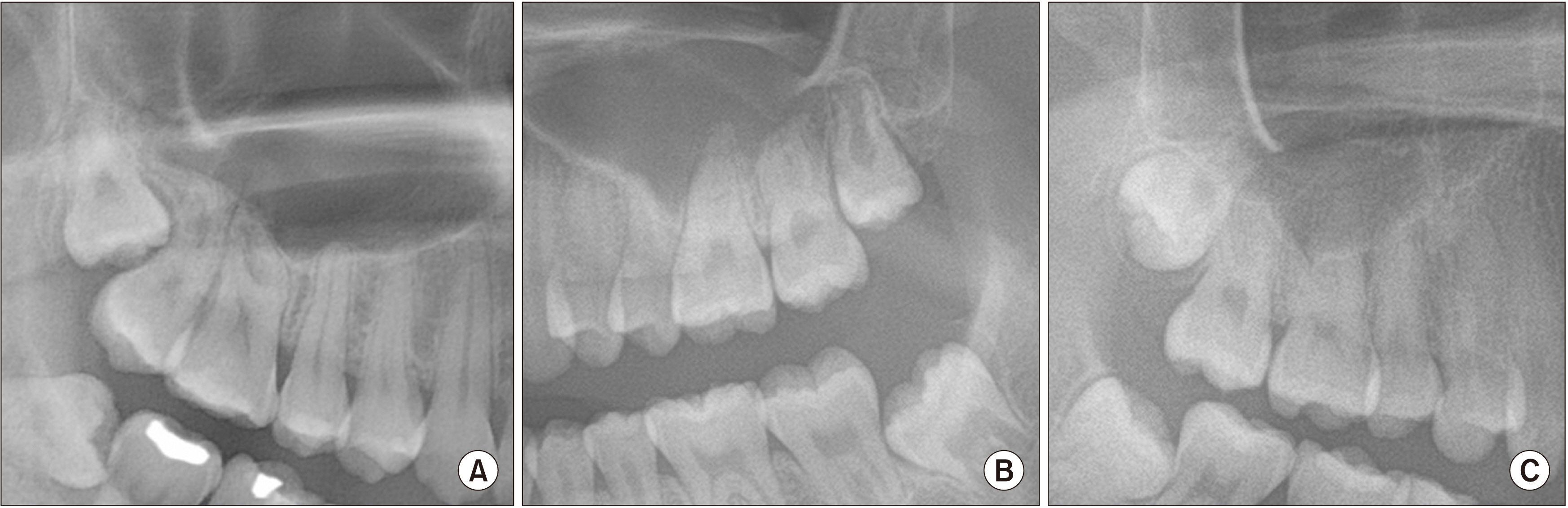
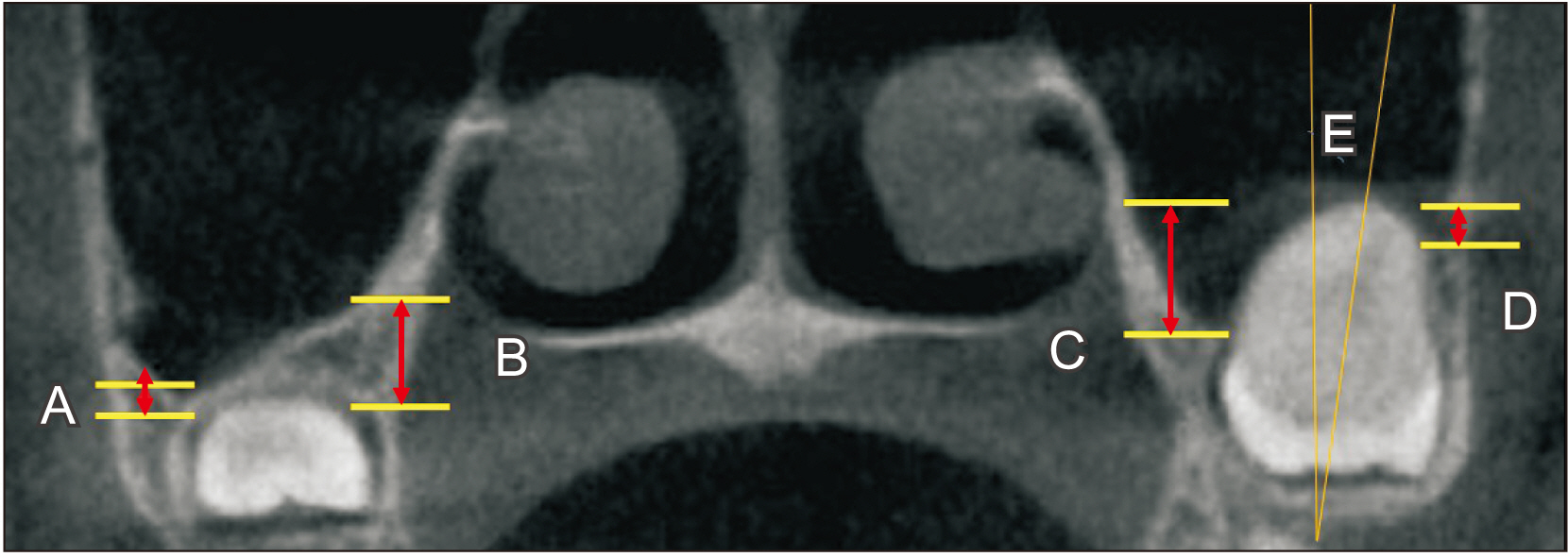
This retrospective study reviewed the clinical records and radiographs of patients who underwent maxillary third-molar extraction. Preoperative panoramas, Waters views, and cone-beam computed tomography were performed for all patients. The patients were divided into two groups; those with and those without swelling of the sinus mucosa swelling or air-fluid level in a postoperative Waters view. We analyzed the age and sex of patients, vertical position, angulation, number of roots, and relation to the maxillary sinus between groups. Statistical analysis used logistic regression and P<0.05 was considered statistically significant.
Results
A total of 91 patients with 153 maxillary third molars were enrolled in the study. Variables significantly related to swelling of the maxillary sinus mucosa after surgical extraction were the age and the distance between the palatal cementoenamel junction (CEJ) and the maxillary sinus floor (P<0.05). Results of the analysis show that the relationship between the CEJ and sinus floor was likely to affect postoperative swelling of the maxillary sinus mucosa.
Conclusion
Maxillary third molars are anatomically adjacent to the maxillary sinus and require careful handling when the maxillary sinus is pneumatized to the CEJ of teeth.
Figure
Reference
-
References
1. Rothamel D, Wahl G, d'Hoedt B, Nentwig GH, Schwarz F, Becker J. 2007; Incidence and predictive factors for perforation of the maxillary antrum in operations to remove upper wisdom teeth: prospective multicentre study. Br J Oral Maxillofac Surg. 45:387–91. https://doi.org/10.1016/j.bjoms.2006.10.013. DOI: 10.1016/j.bjoms.2006.10.013. PMID: 17161510.
Article2. Yurdabakan ZZ, Okumus O, Pekiner FN. 2018; Evaluation of the maxillary third molars and maxillary sinus using cone-beam computed tomography. Niger J Clin Pract. 21:1050–8. https://doi.org/10.4103/njcp.njcp_420_17. DOI: 10.4103/njcp.njcp_420_17. PMID: 30074010.
Article3. Lee D, Ishii S, Yakushiji N. 2013; Displacement of maxillary third molar into the lateral pharyngeal space. J Oral Maxillofac Surg. 71:1653–7. https://doi.org/10.1016/j.joms.2013.05.018. DOI: 10.1016/j.joms.2013.05.018. PMID: 23890786.
Article4. Kocaelli H, Balcioglu HA, Erdem TL. 2011; Displacement of a maxillary third molar into the buccal space: anatomical implications apropos of a case. Int J Oral Maxillofac Surg. 40:650–3. https://doi.org/10.1016/j.ijom.2010.11.021. DOI: 10.1016/j.ijom.2010.11.021. PMID: 21211942.
Article5. Bilginaylar K. 2018; The use of platelet-rich fibrin for immediate closure of acute oroantral communications: an alternative approach. J Oral Maxillofac Surg. 76:278–86. https://doi.org/10.1016/j.joms.2017.07.168. DOI: 10.1016/j.joms.2017.07.168. PMID: 28859924.
Article6. Susarla SM, Dodson TB. 2013; Predicting third molar surgery operative time: a validated model. J Oral Maxillofac Surg. 71:5–13. https://doi.org/10.1016/j.joms.2012.08.004. DOI: 10.1016/j.joms.2012.08.004. PMID: 23010375.
Article7. de Carvalho RW, de Araújo Filho RC, do Egito Vasconcelos BC. 2013; Assessment of factors associated with surgical difficulty during removal of impacted maxillary third molars. J Oral Maxillofac Surg. 71:839–45. https://doi.org/10.1016/j.joms.2013.01.001. DOI: 10.1016/j.joms.2013.01.001. PMID: 23598549.
Article8. Bisla S, Gupta A, Singh H, Sehrawat A, Shukla S. 2022; Evaluation of relationship between odontogenic infections and maxillary sinus changes: a cone beam computed tomography-based study. J Oral Biol Craniofac Res. 12:645–50. https://doi.org/10.1016/j.jobcr.2022.08.001. DOI: 10.1016/j.jobcr.2022.08.001. PMID: 36045940. PMCID: PMC9421310.
Article9. Asaumi R, Sato I, Miwa Y, Imura K, Sunohara M, Kawai T, et al. 2010; Understanding the formation of maxillary sinus in Japanese human foetuses using cone beam CT. Surg Radiol Anat. 32:745–51. https://doi.org/10.1007/s00276-010-0678-5. DOI: 10.1007/s00276-010-0678-5. PMCID: PMC2945628. PMID: 20490493.
Article10. Bui CH, Seldin EB, Dodson TB. 2003; Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 61:1379–89. https://doi.org/10.1016/j.joms.2003.04.001. DOI: 10.1016/j.joms.2003.04.001. PMID: 14663801.
Article11. de Andrade PF, Silva JNN, Sotto-Maior BS, Ribeiro CG, Devito KL, Assis NMSP. 2017; Three-dimensional analysis of impacted maxillary third molars: a cone-beam computed tomographic study of the position and depth of impaction. Imaging Sci Dent. 47:149–55. https://doi.org/10.5624/isd.2017.47.3.149. DOI: 10.5624/isd.2017.47.3.149. PMID: 28989897. PMCID: PMC5620459.
Article12. Lim AA, Wong CW, Allen JC Jr. 2012; Maxillary third molar: patterns of impaction and their relation to oroantral perforation. J Oral Maxillofac Surg. 70:1035–9. https://doi.org/10.1016/j.joms.2012.01.032. DOI: 10.1016/j.joms.2012.01.032. PMID: 22494509.
Article13. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. 2010; An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 4:462–7. DOI: 10.1055/s-0039-1697866. PMID: 20922167. PMCID: PMC2948741.
Article14. Sharan A, Madjar D. 2006; Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 102:375–81. https://doi.org/10.1016/j.tripleo.2005.09.031. DOI: 10.1016/j.tripleo.2005.09.031. PMID: 16920546.
Article15. Shmuly T, Winocur-Arias O, Kahn A, Findler M, Adam I. 2022; Maxillary tuberosity fractures following third molar extraction, prevalence, and risk factors. J Craniofac Surg. 33:e708–12. https://doi.org/10.1097/scs.0000000000008654. DOI: 10.1097/SCS.0000000000008654. PMID: 35765135.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maxillary sinus pneumatization after maxillary molar extraction assessed with cone beam computed tomography
- Which factors are associated with difficult surgical extraction of impacted lower third molars?
- Complications of impacted third molar extraction: retrospective study
- Closure of an oroantral fistula with a bone fragment during surgical extraction of an impacted maxillary second premolar: A case report
- Sinus floor augmentation at the time of tooth removal