Arch Hand Microsurg.
2023 Sep;28(3):125-136. 10.12790/ahm.22.0072.
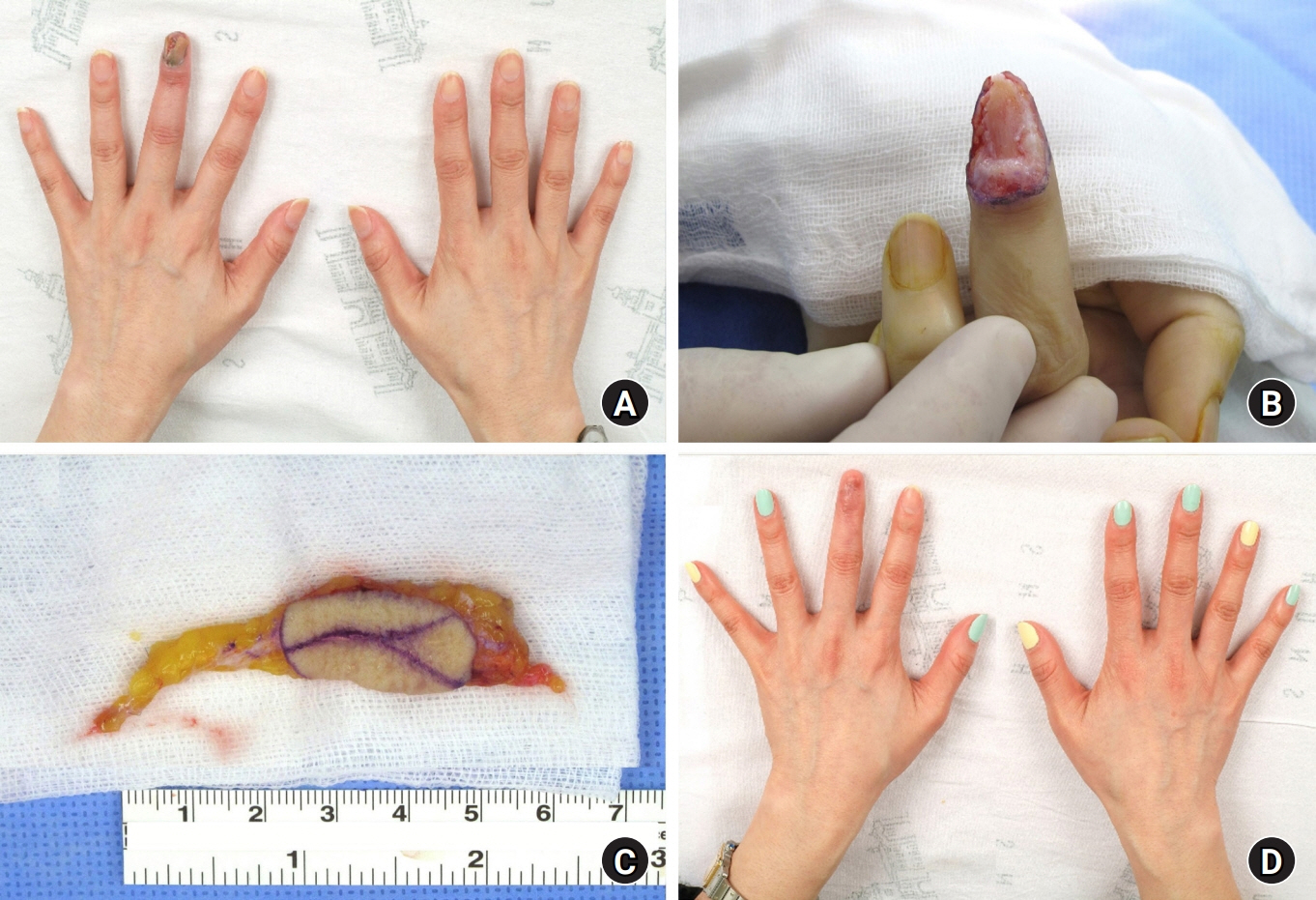
Diagnosis and treatment of subungual melanoma
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Korea
- KMID: 2545523
- DOI: http://doi.org/10.12790/ahm.22.0072
Abstract
- Subungual melanoma (SM) must be suspected in the initial workup of patients with pigmented nails. However, the differential diagnosis of SM from other nail disorders that involve nail pigmentation is challenging. Dermoscopic, clinical, and histopathological features are integrated for a definite diagnosis. The primary treatment of SM is surgery. Depending on the depth of invasion, amputation or functional surgery can be chosen. This article reviews the clinical, dermoscopic, and histopathological features of SM, as well as its diagnosis and treatment.
Keyword
Figure
Reference
-
References
1. De Giorgi V, Saggini A, Grazzini M, et al. Specific challenges in the management of subungual melanoma. Expert Rev Anticancer Ther. 2011; 11(5):749–61.
Article2. Nevares-Pomales OW, Sarriera-Lazaro CJ, Barrera-Llaurador J, et al. Pigmented lesions of the nail unit. Am J Dermatopathol. 2018; 40:793–804.
Article3. Dika E, Patrizi A, Fanti PA, et al. The prognosis of nail apparatus melanoma: 20 years of experience from a single institute. Dermatology. 2016; 232:177–84.
Article4. Banfield CC, Redburn JC, Dawber RP. The incidence and prognosis of nail apparatus melanoma: a retrospective study of 105 patients in four English regions. Br J Dermatol. 1998; 139:276–9.
Article5. Möhrle M, Häfner HM. Is subungual melanoma related to trauma? Dermatology. 2002; 204:259–61.
Article6. Chakera AH, Thompson JF. ASO author reflections: subungual melanomas of the hand present diagnostic and therapeutic challenges. Ann Surg Oncol. 2019; 26:1044–5.
Article7. Newell F, Wilmott JS, Johansson PA, et al. Whole-genome sequencing of acral melanoma reveals genomic complexity and diversity. Nat Commun. 2020; 11:5259.
Article8. Hayward NK, Wilmott JS, Waddell N, et al. Whole-genome landscapes of major melanoma subtypes. Nature. 2017; 545:175–80.
Article9. Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol. 2007; 31:1902–12.10. Reilly DJ, Aksakal G, Gilmour RF, et al. Subungual melanoma: management in the modern era. J Plast Reconstr Aesthet Surg. 2017; 70:1746–52.
Article11. Ishihara Y, Matsumoto K, Kawachi S, Saida T. Detection of early lesions of “ungual” malignant melanoma. Int J Dermatol. 1993; 32:44–7.
Article12. Shukla VK, Hughes LE. Differential diagnosis of subungual melanoma from a surgical point of view. Br J Surg. 1989; 76:1156–60.
Article13. Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol. 2007; 56:835–47.
Article14. Gregorcyk S, Shelton RM, Ladaga LE, Perry RR. Pathologic fracture secondary to subungual melanoma. J Surg Oncol. 1996; 61:230–3.
Article15. Nguyen JT, Bakri K, Nguyen EC, Johnson CH, Moran SL. Surgical management of subungual melanoma: mayo clinic experience of 124 cases. Ann Plast Surg. 2013; 71:346–54.16. Moehrle M, Metzger S, Schippert W, Garbe C, Rassner G, Breuninger H. “Functional” surgery in subungual melanoma. Dermatol Surg. 2003; 29:366–74.
Article17. Lazar A, Abimelec P, Dumontier C. Full thickness skin graft for nail unit reconstruction. J Hand Surg Br. 2005; 30:194–8.
Article18. Pham F, Boespflug A, Duru G, et al. Dermatoscopic and clinical features of congenital or congenital-type nail matrix nevi: a multicenter prospective cohort study by the International Dermoscopy Society. J Am Acad Dermatol. 2022; 87:551–8.
Article19. Duarte AF, Correia O, Barros AM, Ventura F, Haneke E. Nail melanoma in situ: clinical, dermoscopic, pathologic clues, and steps for minimally invasive treatment. Dermatol Surg. 2015; 41:59–68.20. Goettmann S, Moulonguet I, Zaraa I. In situ nail unit melanoma: epidemiological and clinic-pathologic features with conservative treatment and long-term follow-up. J Eur Acad Dermatol Venereol. 2018; 32:2300–6.
Article21. Ronger S, Touzet S, Ligeron C, et al. Dermoscopic examination of nail pigmentation. Arch Dermatol. 2002; 138:1327–33.
Article22. Mun JH, Kim GW, Jwa SW, et al. Dermoscopy of subungual haemorrhage: its usefulness in differential diagnosis from nail-unit melanoma. Br J Dermatol. 2013; 168:1224–9.
Article23. Saida T, Ohshima Y. Clinical and histopathologic characteristics of early lesions of subungual malignant melanoma. Cancer. 1989; 63:556–60.
Article24. Yun SJ, Kim SJ. Images in clinical medicine: Hutchinson’s nail sign. N Engl J Med. 2011; 364:e38.25. Baran LR, Ruben BS, Kechijian P, Thomas L. Non-melanoma Hutchinson’s sign: a reappraisal of this important, remarkable melanoma simulant. J Eur Acad Dermatol Venereol. 2018; 32:495–501.
Article26. Cooper C, Arva NC, Lee C, et al. A clinical, histopathologic, and outcome study of melanonychia striata in childhood. J Am Acad Dermatol. 2015; 72:773–9.
Article27. Güneş P, Göktay F. Melanocytic lesions of the nail unit. Dermatopathology (Basel). 2018; 5:98–107.
Article28. Lee WJ, Lee JH, Won CH, et al. Nail apparatus melanoma: a comparative, clinicoprognostic study of the initial clinical and morphological characteristics of 49 patients. J Am Acad Dermatol. 2015; 73:213–20.
Article29. Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000; 42(2 Pt 1):269–74.30. Ko D, Oromendia C, Scher R, Lipner SR. Retrospective single-center study evaluating clinical and dermoscopic features of longitudinal melanonychia, ABCDEF criteria, and risk of malignancy. J Am Acad Dermatol. 2019; 80:1272–83.
Article31. Lee JH, Park JH, Lee JH, Lee DY. Early detection of subungual melanoma in situ: proposal of ABCD strategy in clinical practice based on case series. Ann Dermatol. 2018; 30:36–40.32. Zalaudek I, Argenziano G, Di Stefani A, et al. Dermoscopy in general dermatology. Dermatology. 2006; 212:7–18.33. Kittler H, Marghoob AA, Argenziano G, et al. Standardization of terminology in dermoscopy/dermatoscopy: results of the third consensus conference of the International Society of Dermoscopy. J Am Acad Dermatol. 2016; 74:1093–106.
Article34. Light RJ. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull. 1971; 76:365–77.
Article35. Di Chiacchio N, Hirata SH, Enokihara MY, Michalany NS, Fabbrocini G, Tosti A. Dermatologists’ accuracy in early diagnosis of melanoma of the nail matrix. Arch Dermatol. 2010; 146:382–7.
Article36. Hirata SH, Yamada S, Enokihara MY, et al. Patterns of nail matrix and bed of longitudinal melanonychia by intraoperative dermatoscopy. J Am Acad Dermatol. 2011; 65:297–303.
Article37. Ohn J, Jo G, Cho Y, Sheu SL, Cho KH, Mun JH. Assessment of a predictive scoring model for dermoscopy of subungual melanoma in situ. JAMA Dermatol. 2018; 154:890–6.
Article38. Ohn J, Choe YS, Mun JH. Dermoscopic features of nail matrix nevus (NMN) in adults and children: a comparative analysis. J Am Acad Dermatol. 2016; 75:535–40.
Article39. Ohn J, Hur K, Cho Y, et al. Developing a predictive model for distinguishing invasive nail unit melanoma from nail unit melanoma in situ. J Eur Acad Dermatol Venereol. 2021; 35:906–11.40. Grover C, Bansal S. Nail biopsy: a user’s manual. Indian Dermatol Online J. 2018; 9:3–15.
Article41. Shin HT, Jang KT, Mun GH, Lee DY, Lee JB. Histopathological analysis of the progression pattern of subungual melanoma: late tendency of dermal invasion in the nail matrix area. Mod Pathol. 2014; 27:1461–7.
Article42. Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg. 2001; 27:580–4.
Article43. de Berker DA. Lateral longitudinal nail biopsy. Australas J Dermatol. 2001; 42:142–4.44. Richert B, Theunis A, Norrenberg S, André J. Tangential excision of pigmented nail matrix lesions responsible for longitudinal melanonychia: evaluation of the technique on a series of 30 patients. J Am Acad Dermatol. 2013; 69:96–104.
Article45. Zhou Y, Chen W, Liu ZR, Liu J, Huang FR, Wang DG. Modified shave surgery combined with nail window technique for the treatment of longitudinal melanonychia: evaluation of the method on a series of 67 cases. J Am Acad Dermatol. 2019; 81:717–22.
Article46. Park SW, Jang KT, Lee JH, et al. Scattered atypical melanocytes with hyperchromatic nuclei in the nail matrix: diagnostic clue for early subungual melanoma in situ. J Cutan Pathol. 2016; 43:41–52.
Article47. Amin B, Nehal KS, Jungbluth AA, et al. Histologic distinction between subungual lentigo and melanoma. Am J Surg Pathol. 2008; 32:835–43.
Article48. Husain S, Scher RK, Silvers DN, Ackerman AB. Melanotic macule of nail unit and its clinicopathologic spectrum. J Am Acad Dermatol. 2006; 54:664–7.
Article49. Chu A, André J, Rich P, Leachman S, Thompson CT. Immunohistochemical characterization of benign activation of junctional melanocytes and melanoma in situ of the nail unit. J Cutan Pathol. 2019; 46:479–83.
Article50. Darmawan CC, Jo G, Montenegro SE, et al. Early detection of acral melanoma: a review of clinical, dermoscopic, histopathologic, and molecular characteristics. J Am Acad Dermatol. 2019; 81:805–12.51. Ren M, Ren J, Cai X, et al. Clinicopathological, immunohistochemical and fluorescence in-situ hybridisation features of early subungual melanoma: an analysis of 65 cases. Histopathology. 2021; 78:717–26.
Article52. Ohn J, Bae JM, Lim JS, et al. Acral lentiginous melanoma, indolent subtype diagnosed by en bloc excision: a case report. Ann Dermatol. 2017; 29:327–30.
Article53. Romano RC, Shon W, Sukov WR. Malignant melanoma of the nail apparatus: a fluorescence in situ hybridization analysis of 7 cases. Int J Surg Pathol. 2016; 24:512–8.54. Dasgupta T, Brasfield R. Subungual melanoma: 25-year review of cases. Ann Surg. 1965; 161:545–52.
Article55. Rondinelli RD. Changes for the new AMA Guides to impairment ratings, 6th edition: implications and applications for physician disability evaluations. PM R. 2009; 1:643–56.56. Chow WT, Bhat W, Magdub S, Orlando A. In situ subungual melanoma: digit salvaging clearance. J Plast Reconstr Aesthet Surg. 2013; 66:274–6.
Article57. Cochran AM, Buchanan PJ, Bueno RA Jr, Neumeister MW. Subungual melanoma: a review of current treatment. Plast Reconstr Surg. 2014; 134:259–73.58. Jo G, Cho SI, Choi S, Mun JH. Functional surgery versus amputation for in situ or minimally invasive nail melanoma: a meta-analysis. J Am Acad Dermatol. 2019; 81:917–22.
Article59. Flores-Terry M, Romero-Aguilera G, Mendoza C, et al. Functional surgery for malignant subungual tumors: a case series and literature review. Actas Dermosifiliogr (Engl Ed). 2018; 109:712–21.
Article60. Sureda N, Phan A, Poulalhon N, Balme B, Dalle S, Thomas L. Conservative surgical management of subungual (matrix derived) melanoma: report of seven cases and literature review. Br J Dermatol. 2011; 165:852–8.
Article61. Jo G, Hur K, Cho SI, Mun JH. Secondary intention healing after functional surgery for in situ or minimally invasive nail melanoma. Acta Derm Venereol. 2020; 100:adv00179.
Article62. Kim BJ, Kim J, Hu J, Kwak Y, Kwon ST. Functional surgery for subungual melanoma: surgical tips based on histological analysis of 21 cadavers. Dermatol Surg. 2022; 48:7–11.
Article63. Yoo H, Kim H, Kwon ST, et al. Tumor invasion in the hyponychium is associated with distant metastasis and poor prognosis in subungual melanoma: a histologic landscape of 44 cases. J Am Acad Dermatol. 2022; 86:1027–34.
Article64. Brodland DG. The treatment of nail apparatus melanoma with Mohs micrographic surgery. Dermatol Surg. 2001; 27:269–73.
Article65. Matsumoto A, Strickland N, Nijhawan RI, Srivastava D. Nail unit melanoma in situ treated with mohs micrographic surgery. Dermatol Surg. 2021; 47:98–103.
Article66. Finley RK 3rd, Driscoll DL, Blumenson LE, Karakousis CP. Subungual melanoma: an eighteen-year review. Surgery. 1994; 116:96–100.67. Lee KT, Park BY, Kim EJ, et al. Superthin SCIP flap for reconstruction of subungual melanoma: aesthetic functional surgery. Plast Reconstr Surg. 2017; 140:1278–89.
Article68. Park JU, Kim K, Kwon ST. Venous free flaps for the treatment of skin cancers of the digits. Ann Plast Surg. 2015; 74:536–42.
Article69. Yun MJ, Park JU, Kwon ST. Surgical options for malignant skin tumors of the hand. Arch Plast Surg. 2013; 40:238–43.
Article70. Woo SJ, Ma IZ, Kwon ST, Park SO, Kim BJ, Hong KY. Long-term results of wide local excision with concurrent venous free flap reconstruction in subungual melanoma. Arch Hand Microsurg. 2022; 27:240–6.
Article71. Morton DL, Thompson JF, Cochran AJ, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014; 370:599–609.
Article72. Martin DE, English JC, Goitz RJ. Subungual malignant melanoma. J Hand Surg Am. 2011; 36:704–7.
Article73. Hinchcliff KM, Pereira C. Subungual tumors: an algorithmic approach. J Hand Surg Am. 2019; 44:588–98.
Article74. Bormann G, Marsch WC, Haerting J, Helmbold P. Concomitant traumas influence prognosis in melanomas of the nail apparatus. Br J Dermatol. 2006; 155:76–80.
Article75. Sinno S, Wilson S, Billig J, Shapiro R, Choi M. Primary melanoma of the hand: an algorithmic approach to surgical management. J Plast Surg Hand Surg. 2015; 49:339–45.
Article76. Pasquali S, Hadjinicolaou AV, Chiarion Sileni V, Rossi CR, Mocellin S. Systemic treatments for metastatic cutaneous melanoma. Cochrane Database Syst Rev. 2018; 2:CD011123.
Article77. Chen YA, Teer JK, Eroglu Z, et al. Translational pathology, genomics and the development of systemic therapies for acral melanoma. Semin Cancer Biol. 2020; 61:149–57.
Article78. Swetter SM, Tsao H, Bichakjian CK, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2019; 80:208–50.
Article79. Curti BD, Faries MB. Recent advances in the treatment of melanoma. N Engl J Med. 2021; 384:2229–40.
Article80. Pavri SN, Clune J, Ariyan S, Narayan D. Malignant melanoma: beyond the basics. Plast Reconstr Surg. 2016; 138:330e–340e.
Article81. Guo J, Carvajal RD, Dummer R, et al. Efficacy and safety of nilotinib in patients with KIT-mutated metastatic or inoperable melanoma: final results from the global, single-arm, phase II TEAM trial. Ann Oncol. 2017; 28:1380–7.
Article82. Woodman SE, Davies MA. Targeting KIT in melanoma: a paradigm of molecular medicine and targeted therapeutics. Biochem Pharmacol. 2010; 80:568–74.
Article83. Zaremba A, Murali R, Jansen P, et al. Clinical and genetic analysis of melanomas arising in acral sites. Eur J Cancer. 2019; 119:66–76.
Article84. Nakamura Y, Namikawa K, Yoshino K, et al. Anti-PD1 checkpoint inhibitor therapy in acral melanoma: a multicenter study of 193 Japanese patients. Ann Oncol. 2020; 31:1198–206.
Article