Ann Rehabil Med.
2023 Aug;47(4):237-260. 10.5535/arm.23071.
Disaster Response and Management: The Integral Role of Rehabilitation
- Affiliations
-
- 1Department of Rehabilitation Medicine, Royal Melbourne Hospital, Parkville, Australia
- 2Department of Medicine (Royal Melbourne Hospital), University of Melbourne, Parkville, Australia
- 3Australian Rehabilitation Research Centre, Royal Melbourne Hospital, Parkville, Australia
- KMID: 2545321
- DOI: http://doi.org/10.5535/arm.23071
Abstract
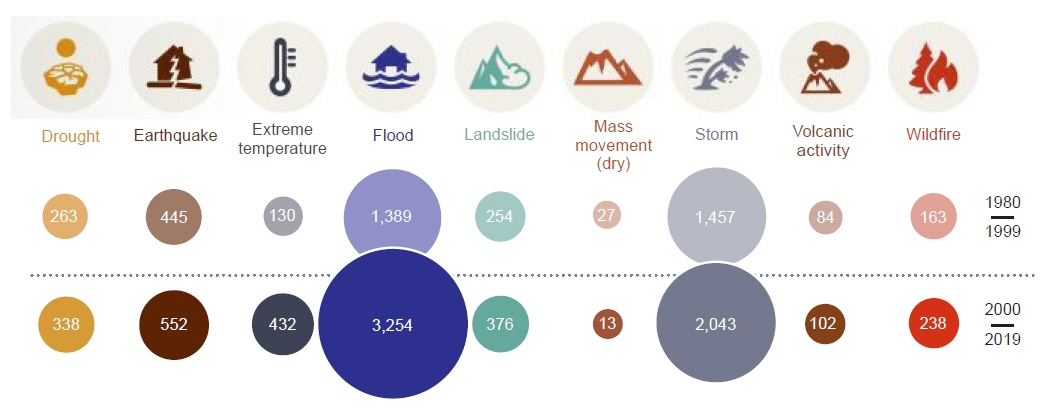
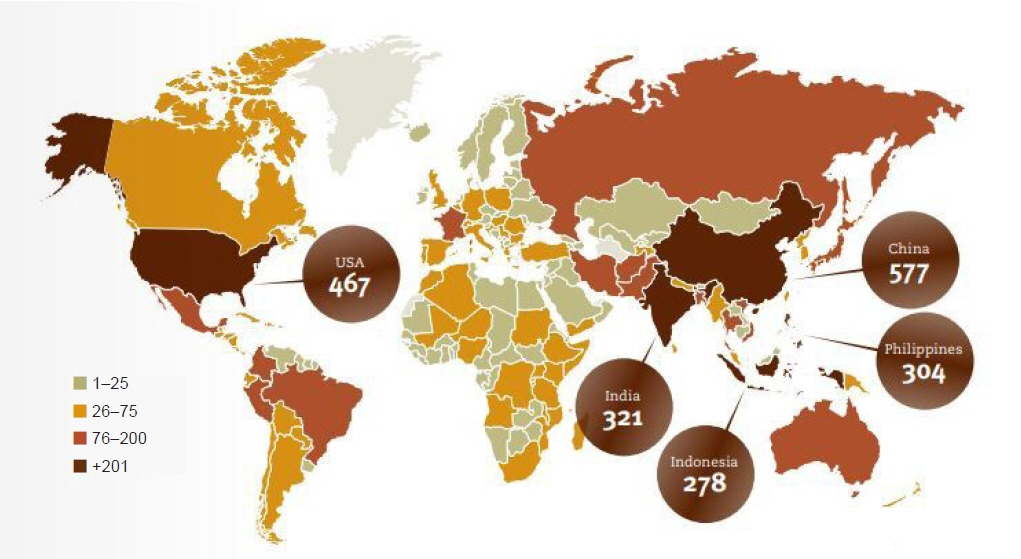
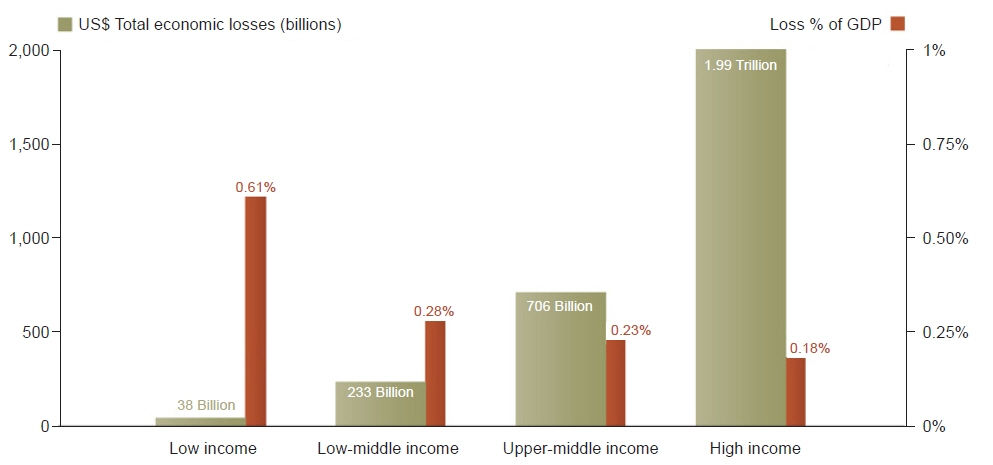
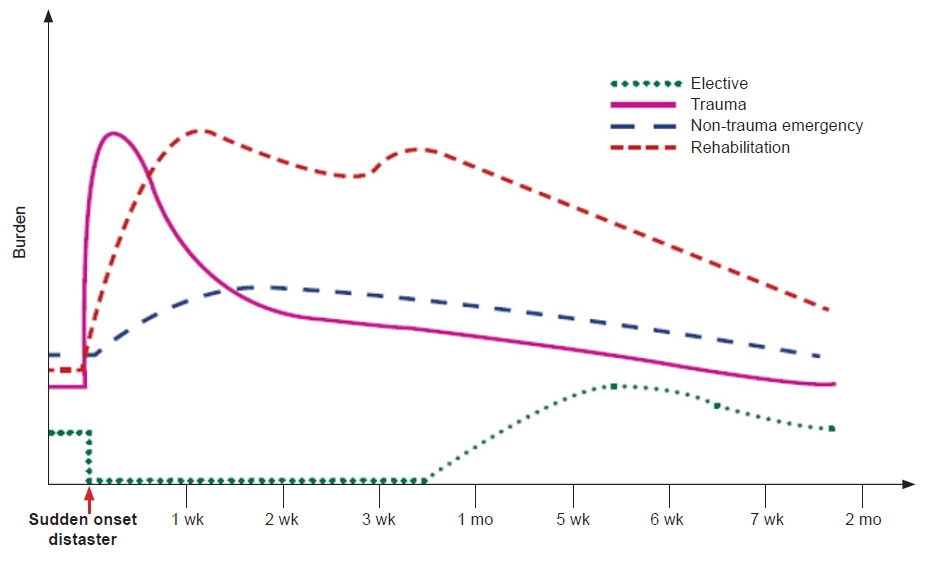
- With the increasing frequency of disasters and the significant upsurge of survivors with severe impairments and long-term disabling conditions, there is a greater focus on the importance of rehabilitation in disaster management. During disasters, rehabilitation services confront a greater load due to the influx of victims, management of persons with pre-existing disabilities and chronic conditions, and longer-term care continuum. Despite robust consensus amongst the international disaster response and management community for the rehabilitation-inclusive disaster management process, rehabilitation is still less prioritised. Evidence supports the early involvement of rehabilitation professionals in disaster response and management for minimising mortality and disability, and improving clinical outcomes and participation in disaster survivors. In the last two decades, there have been substantial developments in disaster response/management processes including the World Health Organization Emergency Medical Team (EMT) initiative, which provides a standardized structured plan to provide effective and coordinated care during disasters. However, rehabilitation-inclusive disaster management plans are yet to be developed and/or implemented in many disaster-prone countries. Strong leadership and effective action from national and international bodies are required to strengthen national rehabilitation capacity (services and skilled workforce) and empower international and local EMTs and health services for comprehensive disaster management in future calamities. This narrative review highlights the role of rehabilitation and current developments in disaster rehabilitation; challenges and key future perspectives in this area.
Keyword
Figure
Reference
-
1. United Nations Office for Disaster Risk Reduction (UNISDR). 2009 UNISDR terminology on disaster risk reduction. UNISDR;2009.2. Guha-Sapir D, Hoyois P, Below R. Annual disaster statistical review 2015: the numbers and trends. Centre for Research on the Epidemiology of Disasters (CRED);2016.3. Below R, Wirtz A, Guha-Sapir D. Disaster category classification and peril terminology for operational purposes. Centre for Research on the Epidemiology of Disasters (CRED); Munich Reinsurance Company;2009.4. Centre for Research on the Epidemiology of Disasters (CRED); United Nations Office for Disaster Risk Reduction (UNISDR). Human cost of disasters. An overview of the last 20 years 2000-2019 [Internet]. UNISDR;2020. [cited 2023 Feb 24]. Available from: https://cred.be/sites/default/files/CRED-Disaster-Report-Human-Cost2000-2019.pdf.5. Brassard C, Howitt AM, Giles DW. Natural disaster management in the Asia-Pacific: policy and governance. Book series: disaster risk reduction methods, approaches and practices. Springer Japan;2015.6. Khan F, Amatya B, Rathore FA, Galea MP. Medical rehabilitation in natural disasters in the Asia-Pacific region: the way forward. Int J Natural Disaster Health Secur. 2015; 2:6–12.7. Amatya B, Khan F. Overview of medical rehabilitation in natural disasters in the Pacific Island countries. Phys Med Rehabil Int. 2016; 3:1090.8. Guha-Sapir D, Vanderveken A. CRED CRUNCH: 2016 preliminary data: Human impact of natural disasters (Issue No. 45). Centre for Research on the Epidemiology of Disasters (CRED), December 2016.9. Centre for Research on the Epidemiology of Disasters (CRED). 2022 Disasters in numbers [Internet]. CRED;2023. [cited 2023 Mar 14]. Available from: https://cred.be/sites/default/files/2022_EMDAT_report.pdf.10. Okuyama Y, Sahin S. Impact estimation of disasters: a global aggregate for 1960 to 2007. World Bank;2009.11. de Goyet CDV, Sarmiento J, Grünewald F. Health response to the earthquake in Haiti January 2010: lessons to be learned for the next massive sudden-onset disaster. Pan American Health Organization (PAHO);2011.12. Amatya B, Galea M, Li J, Khan F. Medical rehabilitation in disaster relief: towards a new perspective. J Rehabil Med. 2017; 49:620–8.
Article13. Ramirez M, Peek-Asa C. Epidemiology of traumatic injuries from earthquakes. Epidemiol Rev. 2005; 27:47–55.
Article14. Bortolin M, Morelli I, Voskanyan A, Joyce NR, Ciottone GR. Earthquake-related orthopedic injuries in adult population: a systematic review. Prehosp Disaster Med. 2017; 32:201–8.
Article15. MacKenzie JS, Banskota B, Sirisreetreerux N, Shafiq B, Hasenboehler EA. A review of the epidemiology and treatment of orthopaedic injuries after earthquakes in developing countries. World J Emerg Surg. 2017; 12:9.
Article16. Ngaruiya C, Bernstein R, Leff R, Wallace L, Agrawal P, Selvam A, et al. Systematic review on chronic non-communicable disease in disaster settings. BMC Public Health. 2022; 22:1234.
Article17. Tsuji T, Sasaki Y, Matsuyama Y, Sato Y, Aida J, Kondo K, et al. Reducing depressive symptoms after the Great East Japan Earthquake in older survivors through group exercise participation and regular walking: a prospective observational study. BMJ Open. 2017; 7:e013706.
Article18. Huang KS, He DX, Huang DJ, Tao QL, Deng XJ, Zhang B, et al. Changes in ischemic heart disease mortality at the global level and their associations with natural disasters: a 28-year ecological trend study in 193 countries. PLoS One. 2021; 16:e0254459.
Article19. World Health Organization (WHO). Classification and minimum standards for emergency medical teams. WHO;2021. p. 1–147.20. World Health Organization (WHO). Emergency medical teams: minimum technical standards and recommendations for rehabilitation. WHO;2016.21. von Schreeb J, Riddez L, Samnegård H, Rosling H. Foreign field hospitals in the recent sudden-onset disasters in Iran, Haiti, Indonesia, and Pakistan. Prehosp Disaster Med. 2008; 23:144–51. discussion 152-3.
Article22. Rathore FA, Gosney JE, Reinhardt JD, Haig AJ, Li J, DeLisa JA. Medical rehabilitation after natural disasters: why, when, and how? Arch Phys Med Rehabil. 2012; 93:1875–81.
Article23. Khan F, Amatya B, Gosney J, Rathore FA, Burkle FM Jr. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil. 2015; 96:1709–27.
Article24. Landry MD, McGlynn M, Ng E, Andreoli A, Devji T, Bower C, et al. Humanitarian response following the earthquake in Haiti: reflections on unprecedented need for rehabilitation. World Health Popul. 2010; 12:18–22.25. World Health Organization (WHO); World Bank. World report on disability. WHO;2011.26. Greaney P, Pfiffner S, Wilson D. The Sphere Project: humanitarian charter and minimum standards in humanitarian response. Practical Action Publishing;2011.27. Gosney JE Jr. Physical medicine and rehabilitation: critical role in disaster response. Disaster Med Public Health Prep. 2010; 4:110–2.
Article28. World Health Organization (WHO). Rehabilitation in health systems: guide for action. WHO;2019.29. Ganchoon F, Bugho R, Calina L, Dy R, Gosney J. Philippine Academy of Rehabilitation Medicine emergency basic relief and medical aid mission project (November 2013-February 2014): the role of physiatrists in Super Typhoon Haiyan. Disabil Rehabil. 2018; 40:2217–25.
Article30. World Health Organization (WHO); International Federation of Red Cross and Red Crescent Societies (IFRC). The regulation and management of international emergency medical teams. WHO; IFRC;2017.31. Amatya B, Lee SY, Galea MP, Khan F. Disaster rehabilitation response plan: now or never. Am J Phys Med Rehabil. 2020; 99:170–7.32. Li Y, Reinhardt JD, Gosney JE, Zhang X, Hu X, Chen S, et al. Evaluation of functional outcomes of physical rehabilitation and medical complications in spinal cord injury victims of the Sichuan earthquake. J Rehabil Med. 2012; 44:534–40.
Article33. Rathore FA, Farooq F, Muzammil S, New PW, Ahmad N, Haig AJ. Spinal cord injury management and rehabilitation: highlights and shortcomings from the 2005 earthquake in Pakistan. Arch Phys Med Rehabil. 2008; 89:579–85.
Article34. Mallick M, Aurakzai JK, Bile KM, Ahmed N. Large-scale physical disabilities and their management in the aftermath of the 2005 earthquake in Pakistan. East Mediterr Health J. 2010; 16 Suppl:S98–105.
Article35. Hu X, Zhang X, Gosney JE, Reinhardt JD, Chen S, Jin H, et al. Analysis of functional status, quality of life and community integration in earthquake survivors with spinal cord injury at hospital discharge and one-year follow-up in the community. J Rehabil Med. 2012; 44:200–5.
Article36. Jiang RF, Tong HQ, Delucchi KL, Neylan TC, Shi Q, Meffert SM. Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors: a randomized clinical trial. Confl Health. 2014; 8:14.
Article37. Li L, Reinhardt JD, Zhang X, Pennycott A, Zhao Z, Zeng X, et al. Physical function, pain, quality of life and life satisfaction of amputees from the 2008 Sichuan earthquake: a prospective cohort study. J Rehabil Med. 2015; 47:466–71.
Article38. Li WS, Chan SY, Chau WW, Law SW, Chan KM. Mobility, prosthesis use and health-related quality of life of bilateral lower limb amputees from the 2008 Sichuan earthquake. Prosthet Orthot Int. 2019; 43:104–11.
Article39. Ni J, Reinhardt JD, Zhang X, Xiao M, Li L, Jin H, et al. Dysfunction and post-traumatic stress disorder in fracture victims 50 months after the Sichuan earthquake. PLoS One. 2013; 8:e77535.
Article40. Xiao M, Li J, Zhang X, Zhao Z. Factors affecting functional outcome of Sichuan-earthquake survivors with tibial shaft fractures: a follow-up study. J Rehabil Med. 2011; 43:515–20.
Article41. Zang Y, Hunt N, Cox T. A randomised controlled pilot study: the effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry. 2013; 13:41.
Article42. Zhang X, Hu XR, Reinhardt JD, Zhu HJ, Gosney JE, Liu SG, et al. Functional outcomes and health-related quality of life in fracture victims 27 months after the Sichuan earthquake. J Rehabil Med. 2012; 44:206–9.
Article43. Zhang X, Reinhardt JD, Gosney JE, Li J. The NHV rehabilitation services program improves long-term physical functioning in survivors of the 2008 Sichuan earthquake: a longitudinal quasi experiment. PLoS One. 2013; 8:e53995.
Article44. Becker SM. Psychosocial care for women survivors of the tsunami disaster in India. Am J Public Health. 2009; 99:654–8.
Article45. Berger R, Gelkopf M. School-based intervention for the treatment of tsunami-related distress in children: a quasi-randomized controlled trial. Psychother Psychosom. 2009; 78:364–71.
Article46. Akiyama T, Gregorio ER Jr, Kobayashi J. Youth sports activity and young people's well-being after a disaster: a trial with the Mastery Approach to Coaching (MAC) in the Philippines. BMC Res Notes. 2018; 11:747.
Article47. Huang Y, Wong H. Effects of social group work with survivors of the Wenchuan earthquake in a transitional community. Health Soc Care Community. 2013; 21:327–37.
Article48. Kuroda Y, Iwasa H, Orui M, Moriyama N, Suemoto CK, Yashiro C, et al. Risk factor for incident functional disability and the effect of a preventive exercise program: a 4-year prospective cohort study of older survivors from the Great East Japan Earthquake and nuclear disaster. Int J Environ Res Public Health. 2018; 15:1430.
Article49. Wu YT, Chen KH, Ban SL, Tung KY, Chen LR. Evaluation of leap motion control for hand rehabilitation in burn patients: an experience in the dust explosion disaster in Formosa Fun Coast. Burns. 2019; 45:157–64.
Article50. Fahmida U, Hidayat AT, Oka AASI, Suciyanti D, Pathurrahman P, Wangge G. Effectiveness of an integrated nutrition rehabilitation on growth and development of children under five post 2018 earthquake in East Lombok, Indonesia. Int J Environ Res Public Health. 2022; 19:2814.
Article51. World Health Organization (WHO). Emergency Medical Teams Initiative. WHO; 2016 [cited 2023 Mar 14]. Available from: https://extranet.who.int/emt/.52. World Health Organization (WHO). Emergency medical team initiative. Guidelines and publications [Internet]. WHO;2023. [cited 2023 Mar 15]. Available from: https://extranet.who.int/emt/guidelines-and-publications.53. Lathia C, Skelton P, Clift Z. Early rehabilitation in conflicts and disasters [Internet]. Humanity & Inclusion UK;2020. [cited 2023 Mar 14]. Available from: https://www.hi.org/sn_uploads/document/36199-Humanity--Inclusion-Clinical-Handbook-web_1.pdf.54. Humanity & Inclusion UK. Responding internationally to disasters: a do’s and don’ts guide for rehabilitation professionals [Internet]. Humanity & Inclusion UK;2016. [cited 2023 Mar 14]. Available from: https://www.humanity-inclusion.org.uk/sn_uploads/uk/document/responding-disasters-dos-and-donts-guide-rehabilitation-professionals-april-2016.pdf.55. DisasterReady. Develop your skills, maximize your impact [Internet]. DisasterReady;2023; [cited 2023 Mar 10]. Available from: https://www.disasterready.org/.56. United Nations Office for Disaster Risk Reduction. Hyogo Framework for Action 2005-2015: Building the resilience of nations and communities to disasters. UNDRR; 2005.57. Global Facility for Disaster Reduction and Recovery (GFDRR). Bringing resilience to scale. GFDRR;2016.58. United Nations Office for Disaster Risk Reduction (UNISDR). Sendai framework for disaster risk reduction 2015-2030. UNISDR;2015.59. International Society for Physical Rehabilitation Medicine (ISPRM). Disaster Rehabilitation Committee (DRC) [Internet]. ISPRM;2021. [cited 2023 Feb 25]. Available from: https://www.isprm.org/collaborate/drc/.60. United Nations. Sustainable Development Goals: knowledge platform [Internet]. United Nations;2017; [cited 2023 Feb 25]. Available from: https://www.un.org/sustainabledevelopment/.61. World Health Organization (WHO). Rehabilitation in health systems. WHO;2017.62. World Health Organization (WHO). Rehabilitation: key for health in the 21st century. WHO;2017.63. World Health Organization (WHO). Global Cooperation on Assistive Technology (GATE) [Internet]. WHO;2018. [cited 2023 Feb 14]. Available from: https://www.who.int/initiatives/global-cooperation-on-assistive-technology-(gate).64. World Health Organization (WHO). Health emergency and disaster risk management framework. WHO;2019.65. World Health Organization (WHO). Emergency medical team strategy 2030 [Internet]. WHO;2022. [cited 2023 Feb 10]. Available from: https://www.who.int/news/item/04-10-2022-who-launches-the-emergency-medical-teams-2030-strategy-at-global-meeting-to-strengthen-rapid-response-amid-emergencies-worldwide.66. World Health Organization (WHO). World Rehabilitation Alliance (WRA) [Internet]. WHO;2023. [cited 2023 Jul 4]. Available from: https://www.who.int/initiatives/world-rehabilitation-alliance.67. World Health Organization (WHO). Strengthening rehabilitation in health systems [Internet]. WHO;2023. [cited 2023 Jul 4]. Available from: https://apps.who.int/gb/ebwha/pdf_files/EB152/B152%2810%29-en.pdf.68. United Nations Office for Disaster Risk Reduction (UNISDR). UN 2013 global survey explains why so many people living with disabilities die in disasters [Internet]. UNISDR;2013. [cited 2023 Feb 25]. Available from: https://www.undrr.org/news/un-2013-global-survey-explains-why-so-many-people-living-disabilities-die-disasters.69. Economic and Social Commission for Asia and the Pacific (ESCAP). Disasters in Asia and the Pacific: 2014 year in review. United Nations;2015.70. World Health Organization (WHO). The need to scale up rehabilitation. WHO;2017.71. Amatya B, Khan F. COVID-19 in developing countries: a rehabilitation perspective. J Int Soc Phys Rehabil Med. 2020; 3:69–74.72. Khan F, Amatya B, Lee SY, Vasudevan V. Rehabilitation in disaster relief. Phys Med Rehabil Clin N Am. 2019; 30:723–47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disaster Basic Physics and Disaster Paradigm
- Development of a Comprehensive Model of Disaster Management in Korea Based on the Result of Response to Sampung Building Collapse (1995): Disaster Law, and 98 Disaster Preparedness Plan of Seoul City
- Emergency Medicine in Disasters
- Principles and system of disaster medicine
- Disasters and the disaster medicine