Clin Exp Otorhinolaryngol.
2023 Aug;16(3):244-250. 10.21053/ceo.2023.00388.
Surgical Outcomes of Sigmoid Sinus Resurfacing for Pulsatile Tinnitus: The Predictive Value of the Water Occlusion Test and Imaging Studies
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Private Körfez Hospital, Edremit, Türkiye
- KMID: 2545263
- DOI: http://doi.org/10.21053/ceo.2023.00388
Abstract
Objectives
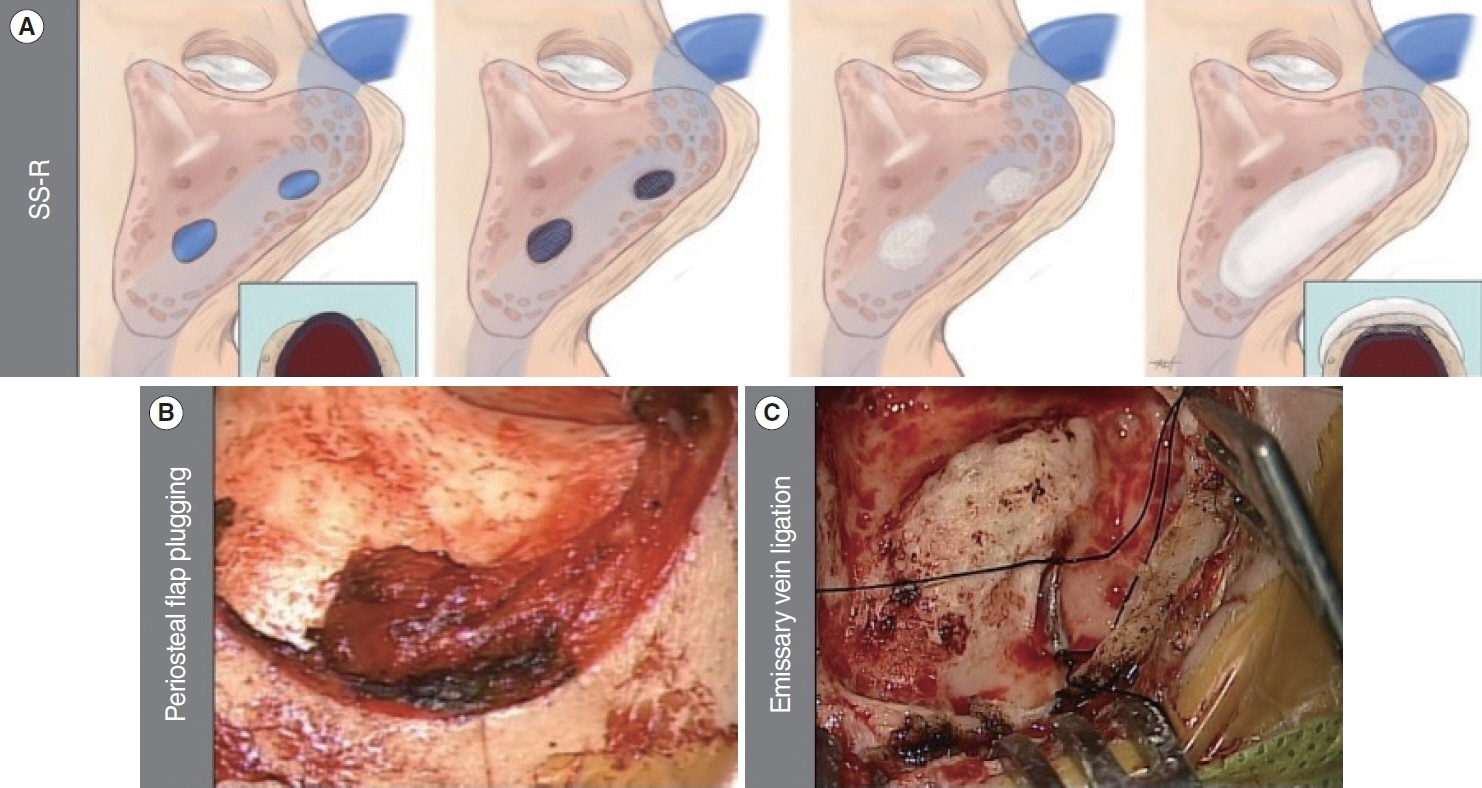
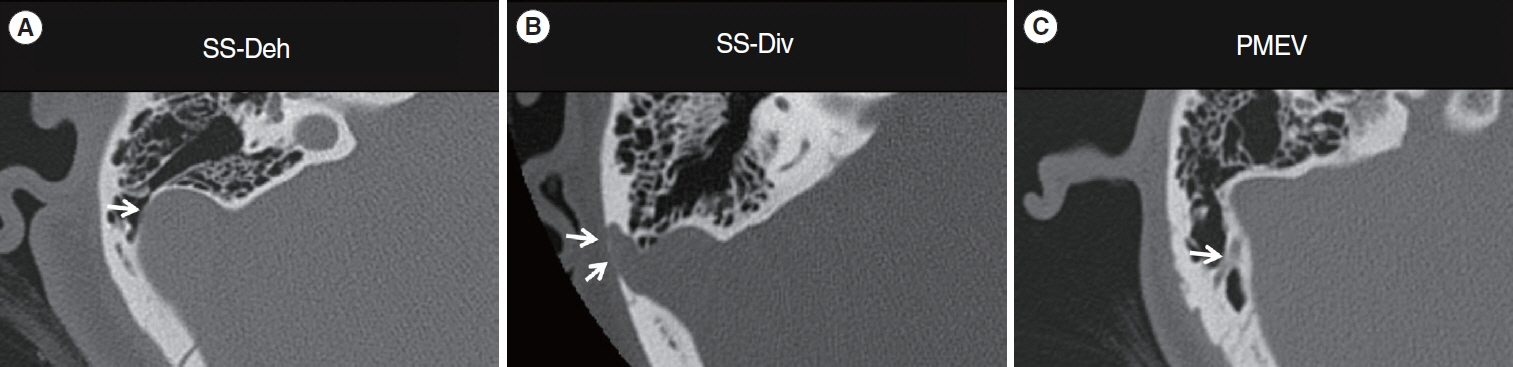
. Sigmoid sinus resurfacing (SS-R) is one of the most effective surgical treatments for patients with pulsatile tinnitus (PT) originating from anatomical variants of the vascular walls in the temporal bone. This study aimed to provide updated information on the clinical outcomes of SS-R and evaluate the efficacy of the water occlusion test (WOT) as an additional diagnostic modality.
Methods
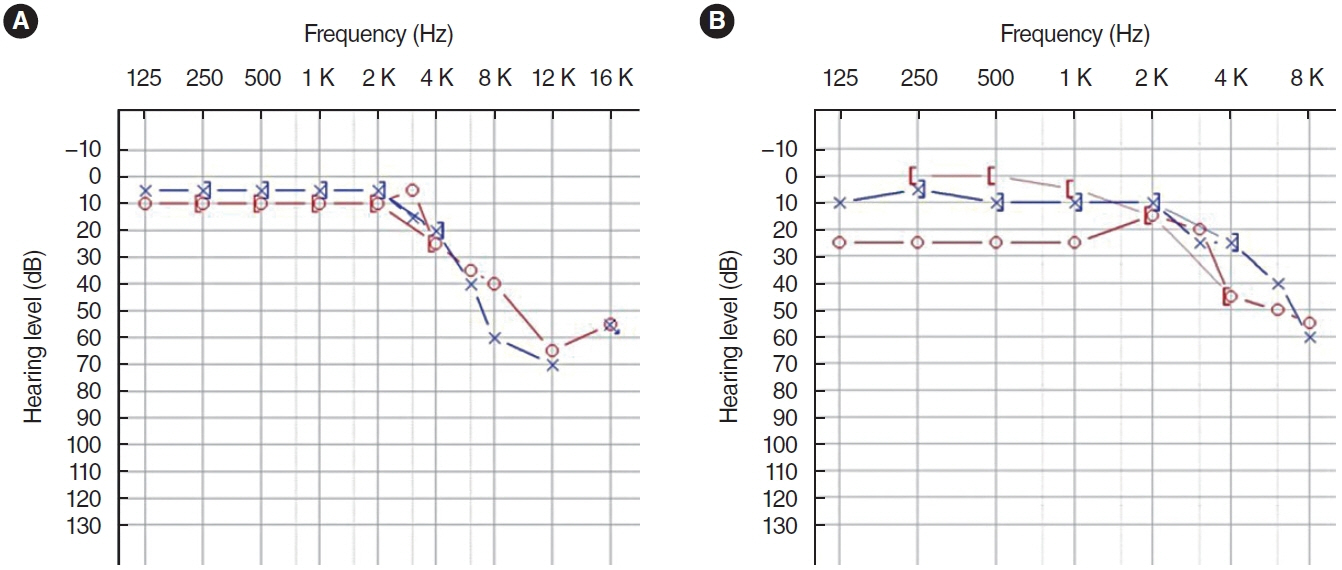
. We retrospectively reviewed medical records including tinnitus questionnaires, temporal bone computed tomography (TBCT) scans, audiologic tests, and preoperative WOT results from patients who underwent SS-R.
Results
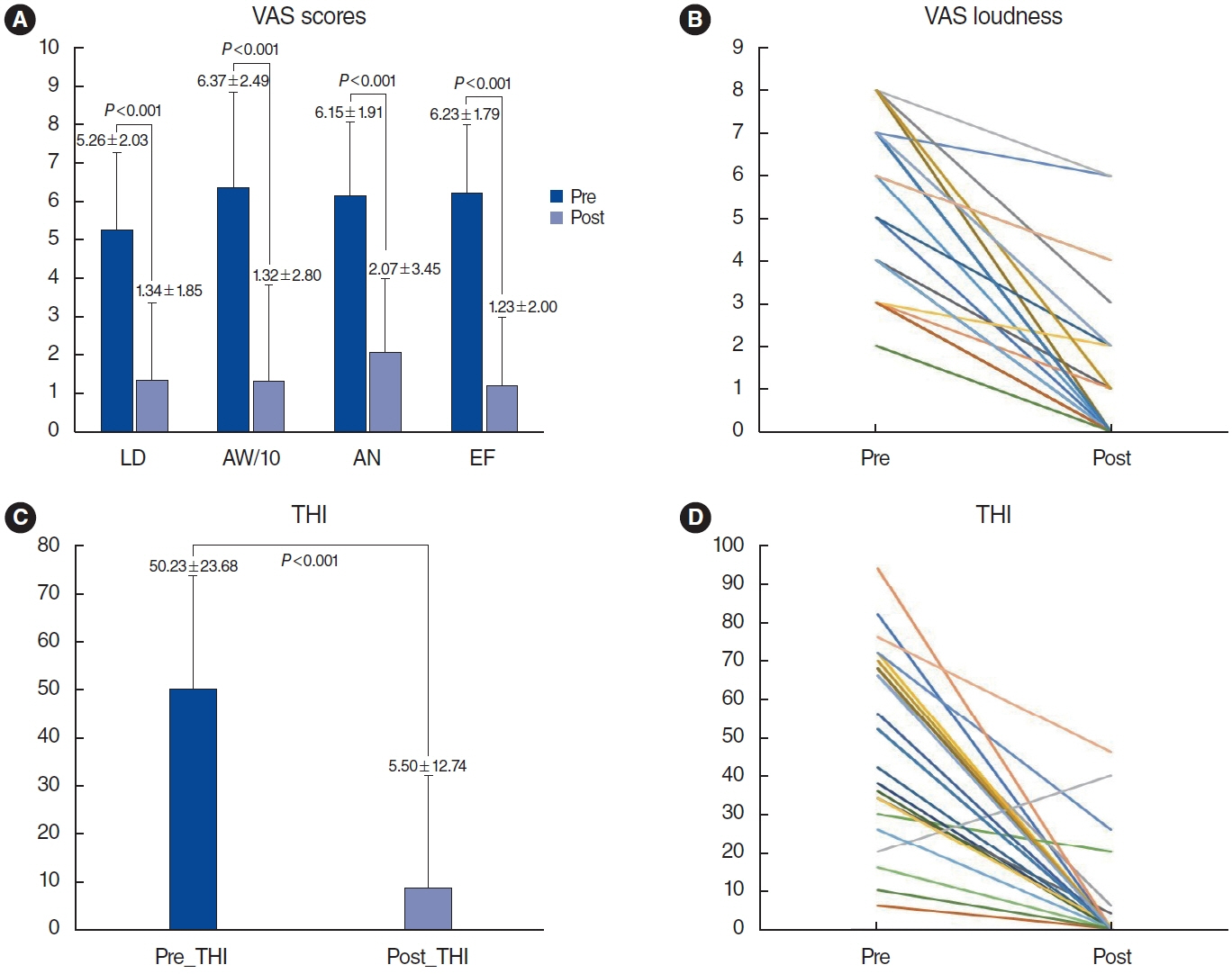
. In total, 26 patients were included in the study. The mean age was 44 years, and the mean symptom duration was 3 months. Fourteen patients (53.8%) were completely cured, seven (26.9%) significantly improved, and five (19.2%) remained stable. The mean visual analog scale loudness score decreased from 5.26 to 1.34 (P<0.001) and the mean Tinnitus Handicap Inventory score also improved from 50.23 to 5.5 (P<0.001) after SS-R surgery. In 10 patients with discrepancies between the preoperative TBCT and intraoperative findings, WOT showed a significant additive effect in predicting surgical outcomes. No patients experienced severe intraoperative or postoperative complications during the entire follow-up period.
Conclusion
. SS-R provides significant symptom improvement in patients with sigmoid sinus dehiscence who had a positive WOT without other sigmoid sinus variants. A combined diagnostic approach with TBCT, WOT, and intraoperative findings is crucial for achieving better surgical outcomes in patients with PT caused by sigmoid sinus variants.
Figure
Reference
-
1. Liyanage SH, Singh A, Savundra P, Kalan A. Pulsatile tinnitus. J Laryngol Otol. 2006; Feb. 120(2):93–7.2. Aggarwal R, Lloyd S. Pulsatile tinnitus. Otorhinolaryngology. 2012; 5(1):7–14.3. Kim CS, Kim SY, Choi H, Koo JW, Yoo SY, An GS, et al. Transmastoid reshaping of the sigmoid sinus: preliminary study of a novel surgical method to quiet pulsatile tinnitus of an unrecognized vascular origin. J Neurosurg. 2016; Aug. 125(2):441–9.4. An YH, Han S, Lee M, Rhee J, Kwon OK, Hwang G, et al. Dural arteriovenous fistula masquerading as pulsatile tinnitus: radiologic assessment and clinical implications. Sci Rep. 2016; Nov. 6:36601.5. Sanchez TG, Murao M, de Medeiros IR, Kii M, Bento RF, Caldas JG, et al. A new therapeutic procedure for treatment of objective venous pulsatile tinnitus. Int Tinnitus J. 2002; 8(1):54–7.6. Kao E, Kefayati S, Amans MR, Faraji F, Ballweber M, Halbach V, et al. Flow patterns in the jugular veins of pulsatile tinnitus patients. J Biomech. 2017; Feb. 52:61–7.7. Eisenman DJ. Sinus wall reconstruction for sigmoid sinus diverticulum and dehiscence: a standardized surgical procedure for a range of radiographic findings. Otol Neurotol. 2011; Sep. 32(7):1116–9.8. Mattox DE, Hudgins P. Algorithm for evaluation of pulsatile tinnitus. Acta Otolaryngol. 2008; Apr. 128(4):427–31.9. Friedmann DR, Le BT, Pramanik BK, Lalwani AK. Clinical spectrum of patients with erosion of the inner ear by jugular bulb abnormalities. Laryngoscope. 2010; Feb. 120(2):365–72.10. Wang JR, Parnes LS. Superior semicircular canal dehiscence associated with external, middle, and inner ear abnormalities. Laryngoscope. 2010; Feb. 120(2):390–3.11. Zeng R, Wang GP, Liu ZH, Liang XH, Zhao PF, Wang ZC, et al. Sigmoid sinus wall reconstruction for pulsatile tinnitus caused by sigmoid sinus wall dehiscence: a single-center experience. PLoS One. 2016; Oct. 11(10):e0164728.12. Grewal AK, Kim HY, Comstock RH, Berkowitz F, Kim HJ, Jay AK. Clinical presentation and imaging findings in patients with pulsatile tinnitus and sigmoid sinus diverticulum/dehiscence. Otol Neurotol. 2014; Jan. 35(1):16–21.13. Park SN, Han JS, Park JM, Jin HJ, Joo HA, Park JT, et al. A novel water occlusion test for disorders causing pulsatile tinnitus: our experience in 32 patients. Clin Otolaryngol. 2020; Mar. 45(2):280–5.14. Sunwoo W, Jeon YJ, Bae YJ, Jang JH, Koo JW, Song JJ. Typewriter tinnitus revisited: the typical symptoms and the initial response to carbamazepine are the most reliable diagnostic clues. Sci Rep. 2017; Sep. 7(1):10615.15. Jeon HW, Kim SY, Choi BS, Bae YJ, Koo JW, Song JJ. Pseudo-low frequency hearing loss and its improvement after treatment may be objective signs of significant vascular pathology in patients with pulsatile tinnitus. Otol Neurotol. 2016; Oct. 37(9):1344–9.16. Chua CA, Han JS, Kim Y, Seo JH, Park SN. Silencing pulsatile tinnitus: a novel technique of periosteal flap obliteration for sigmoid sinus diverticulum variants. Otol Neurotol. 2023; Mar. 44(3):246–51.17. San Millan Ruiz D, Gailloud P, Rufenacht DA, Delavelle J, Henry F, Fasel JH. The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol. 2002; Oct. 23(9):1500–8.18. Louis RG, Loukas M, Wartmann CT, Tubbs RS, Apaydin N, Gupta AA, et al. Clinical anatomy of the mastoid and occipital emissary veins in a large series. Surg Radiol Anat. 2009; Feb. 31(2):139–44.19. Kim LK, Ahn CS, Fernandes AE. Mastoid emissary vein: anatomy and clinical relevance in plastic & reconstructive surgery. J Plast Reconstr Aesthet Surg. 2014; Jun. 67(6):775–80.20. Forte V, Turner A, Liu P. Objective tinnitus associated with abnormal mastoid emissary vein. J Otolaryngol. 1989; Aug. 18(5):232–5.21. Lee SY, Kim MK, Bae YJ, An GS, Lee K, Choi BY, et al. Longitudinal analysis of surgical outcome in subjects with pulsatile tinnitus orignating from the sigmoid sinus. Sci Rep. 2020; Oct. 10(1):18194.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulsatile Tinnitus by Sigmoid Sinus Diverticulum
- Degree of Sigmoid Sinus Compression and the Symptom Relief Using Magnetic Resonance Angiography in Venous Pulsating Tinnitus
- A Case of Surgically Treated Pulsatile Tinnitus by Sigmoid Sinus Diverticulum and/or Dehiscence (SSDD)
- Pulsatile Tinnitus with a Dural Arterio-Venous Fistula Diagnosed by Computed Tomography-Angiography
- Embolization of Dural Arteriovenous Malformation of the Jugular Bulb