J Korean Med Sci.
2023 Aug;38(32):e248. 10.3346/jkms.2023.38.e248.
COVID-19 Vaccination Status Among Korean Pediatric Population With Comorbidities
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Information and Statistics, Department of Bio & Medical Big Data, Research Institute of Natural Science, Gyeongsang National University, Jinju, Korea
- 3Department of Big Data Strategy, National Health Insurance Service, Wonju, Korea
- 4Department of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- 5Artificial Intelligence and Big-Data Convergence Center, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 6Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Seoul, Korea
- KMID: 2545200
- DOI: http://doi.org/10.3346/jkms.2023.38.e248
Abstract
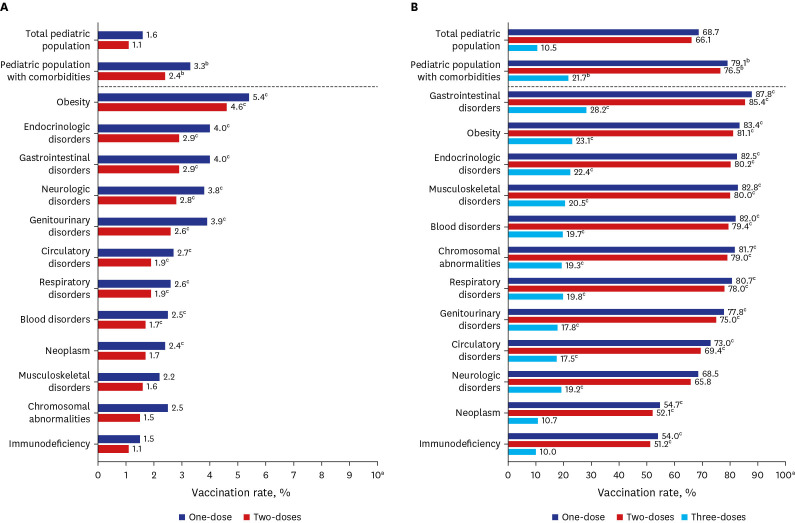
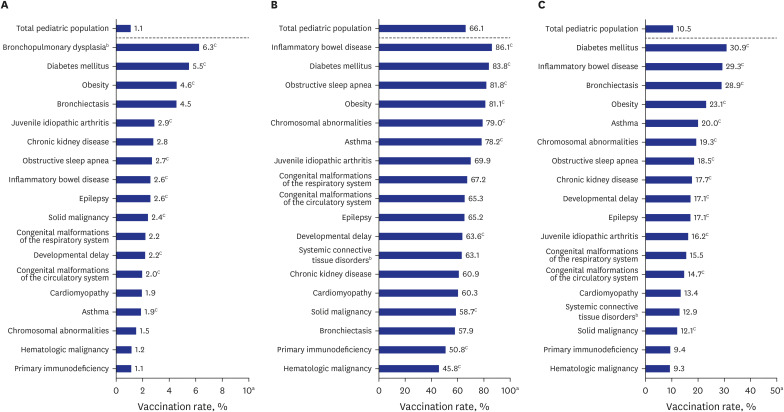
- The pediatric population with comorbidities is a high-risk group for severe coronavirus disease 2019 (COVID-19). As of January 2023, the COVID-19 vaccination rate for at least two doses among Korean children 5–11 years is low at 1.1%. We summarized the COVID-19 vaccination status for the pediatric population (5–17 years) with comorbidities through July 2022 using the National Health Insurance Service database. Pediatric patients with comorbidities had higher vaccination rates than the general pediatric population (2.4% vs. 1.1% in 5–11-year-olds [P < 0.001], 76.5% vs. 66.1% in 12–17-year-olds [P < 0.001]). However, there were substantial differences according to comorbidity category, and the 2-dose vaccination rate was lowest among children with immunodeficiency in all age groups (1.1% in 5–11-year-olds, 51.2% in 12–17-year-olds). The COVID-19 vaccination rate among Korean children has remained stagnant at a low proportion despite ongoing outreach. Thus, more proactive strategies are needed alongside continuous surveillance.
Keyword
Figure
Cited by 1 articles
-
Effective Vaccination and Education Strategies for Emerging Infectious Diseases Such as COVID-19
Seong-Heon Wie, Jaehun Jung, Woo Joo Kim
J Korean Med Sci. 2023;38(44):e371. doi: 10.3346/jkms.2023.38.e371.
Reference
-
1. Shi DS, Whitaker M, Marks KJ, Anglin O, Milucky J, Patel K, et al. Hospitalizations of children aged 5-11 years with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(16):574–581. PMID: 35446827.2. Choi SH, Choi JH, Lee JK, Eun BW, Song SH, Ahn B, et al. Clinical characteristics and outcomes of children with SARS-CoV-2 infection during the delta and omicron variant-dominant periods in Korea. J Korean Med Sci. 2023; 38(9):e65. PMID: 36880106.3. WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020; 20(8):e192–e197. PMID: 32539990.4. Bertran M, Amin-Chowdhury Z, Davies HG, Allen H, Clare T, Davison C, et al. COVID-19 deaths in children and young people in England, March 2020 to December 2021: an active prospective national surveillance study. PLoS Med. 2022; 19(11):e1004118. PMID: 36346784.5. Shin E, Choe YJ, Ryu B, Kim NY, Lee HJ, Kim DH, et al. Pediatric deaths associated with coronavirus disease 2019 (COVID-19) in Korea. J Korean Med Sci. 2023; 38(3):e21. PMID: 36647219.6. Choi YY, Choi SH, Choi JH, Kim DH, Lee JK, Eun BW, et al. SARS-CoV-2-naïve Korean children and adolescents hospitalized with COVID-19 in 2021. J Korean Med Sci. 2022; 37(42):e303. PMID: 36325607.7. Woodruff RC, Campbell AP, Taylor CA, Chai SJ, Kawasaki B, Meek J, et al. Risk factors for severe COVID-19 in children. Pediatrics. 2022; 149(1):e2021053418. PMID: 34935038.8. Korea Disease Control and Prevention Agency. COVID-19 vaccination for children (March 14, 2022). Updated 2023. Accessed May 22, 2023. https://ncov.kdca.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=6475&contSeq=6475&board_id=312&gubun=BDJ .9. Yomiuri Shimbun. Push to have children ages 5-11 get COVID-19 vaccines gains steam (August 16, 2022). Updated 2023. Accessed May 20, 2023. https://japannews.yomiuri.co.jp/society/coronavirus/20220816-51598/ .10. Prime Minister’s Office of Japan. COVID-19 vaccination rates by age group (January 7, 2023). Accessed January 7, 2023. https://www.kantei.go.jp/jp/headline/kansensho/vaccine.html .11. Korea Disease Control and Prevention Agency. COVID-19 vaccination rates by age group (January 7, 2023). Updated 2023. Accessed January 7, 2023. https://ncv.kdca.go.kr/allAgerateStatus.es?mid=a11718000000 .12. Valier MR, Elam-Evans LD, Mu Y, Santibanez TA, Yankey D, Zhou T, et al. Racial and ethnic differences in COVID-19 vaccination coverage among children and adolescents aged 5-17 years and parental intent to vaccinate their children - National Immunization Survey-Child COVID Module, United States, December 2020-September 2022. MMWR Morb Mortal Wkly Rep. 2023; 72(1):1–8. PMID: 36602930.13. Korea Disease Control and Prevention Agency. COVID-19 domestic outbreak and vaccination status (July 28, 2022). Updated 2022. Accessed February 10, 2023. https://ncov.kdca.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=6783&contSeq=6783&board_id=312&gubun=ALL .14. Singson JRC, Kirley PD, Pham H, Rothrock G, Armistead I, Meek J, et al. Factors associated with severe outcomes among immunocompromised adults hospitalized for COVID-19 - COVID-NET, 10 states, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(27):878–884. PMID: 35797216.15. Wang CS, Doma R, Westbrook AL, Johnson J, Anderson EJ, Greenbaum LA, et al. Vaccine attitudes and COVID-19 vaccine intention among parents of children with kidney disease or primary hypertension. Am J Kidney Dis. 2023; 81(1):25–35.e1. PMID: 35750280.16. Yu JH, Jeong HJ, Kim SJ, Lee JY, Choe YJ, Choi EH, et al. Sustained vaccination coverage during the coronavirus disease 2019 epidemic in the Republic of Korea. Vaccines (Basel). 2020; 9(1):2. PMID: 33375172.17. Korea Disease Control and Prevention Agency. High rate of National Immunization Program for Korean children even during the COVID-19 pandemic (July 28, 2022). Updated 2022. Accessed February 10, 2023. https://www.korea.kr/news/pressReleaseView.do?newsId=156518666 .18. Wiegand M, Eagan RL, Karimov R, Lin L, Larson HJ, de Figueiredo A, et al. Global declines in vaccine confidence from 2015 to 2022: a large-scale retrospective analysis. SSRN. Forthcoming. 2023; DOI: 10.2139/ssrn.4438003.19. Lee M, Seo S, Choi S, Park JH, Kim S, Choe YJ, et al. Parental acceptance of COVID-19 vaccination for children and its association with information sufficiency and credibility in South Korea. JAMA Netw Open. 2022; 5(12):e2246624. PMID: 36515950.20. Choi SH, Jo YH, Jo KJ, Park SE. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J Korean Med Sci. 2021; 36(31):e227. PMID: 34402237.21. Monin L, Laing AG, Muñoz-Ruiz M, McKenzie DR, Del Molino Del Barrio I, Alaguthurai T, et al. Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol. 2021; 22(6):765–778. PMID: 33930323.22. Day D, Grech L, Nguyen M, Bain N, Kwok A, Harris S, et al. Serious underlying medical conditions and COVID-19 vaccine hesitancy: a large cross-sectional analysis from Australia. Vaccines (Basel). 2022; 10(6):851. PMID: 35746458.23. Korea Disease Control and Prevention Agency. COVID-19 domestic outbreak and vaccination status (February 19, 2023). Updated 2023. Accessed February 19, 2023. https://ncov.kdca.go.kr/bdBoardList_Real.do?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun= .24. Korea Disease Control and Prevention Agency. Nationwide sample survey of COVID-19 seroprevalence, 2nd. Updated 2023. Accessed February 19, 2023. https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&act=view&list_no=721678 .25. Farrar DS, Drouin O, Moore Hepburn C, Baerg K, Chan K, Cyr C, et al. Risk factors for severe COVID-19 in hospitalized children in Canada: a national prospective study from March 2020-May 2021. Lancet Reg Health Am. 2022; 15:100337. PMID: 35936225.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immune Response to COVID-19 Vaccination in Hematologic Malignancies: A Mini-Review
- Diabetes and COVID-19 Vaccination
- A Case of Aphthous Stomatitis in a Healthy Adult Following COVID-19 Vaccination: Clinical Reasoning
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era
- Delphi Survey for COVID-19 Vaccination in Korean Children Between 5 and 11 Years Old