Korean J Orthod.
2023 Jul;53(4):264-275. 10.4041/kjod22.243.
Maxillary alveolar bone evaluation following dentoalveolar expansion with clear aligners in adults: A cone-beam computed tomography study
- Affiliations
-
- 1Department of Pediatric Dentistry, School of Dentistry of Ribeirão Preto, University of São Paulo, São Paulo, Brazil
- 2Department of Orthodontics, School of Dentistry, Guarulhos University (UNG), São Paulo, Brazil
- KMID: 2545042
- DOI: http://doi.org/10.4041/kjod22.243
Abstract
Objective
To investigate the effects of maxillary orthodontic expansion on the alveolar bone tissue in adult patients treated with aligners by using conebeam computed tomography.
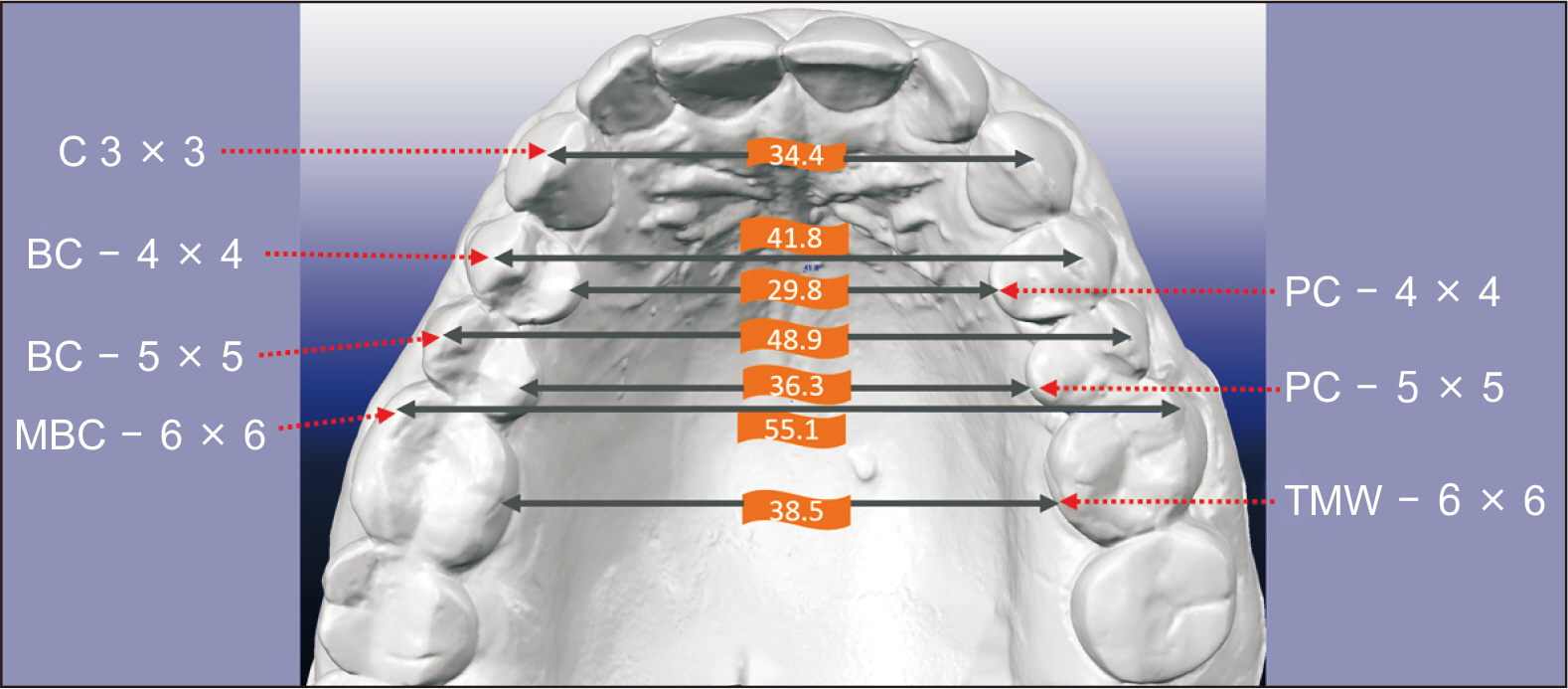
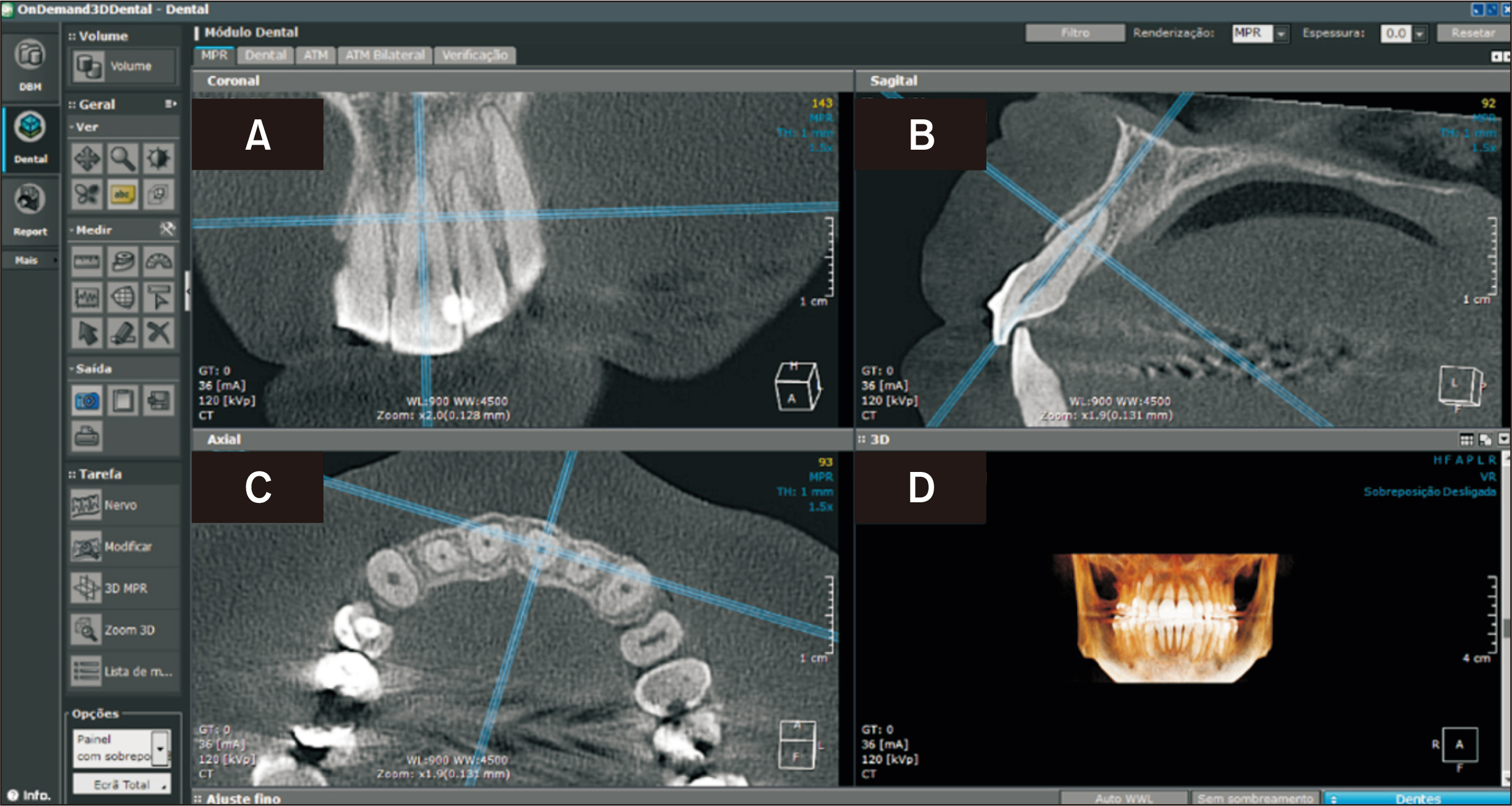
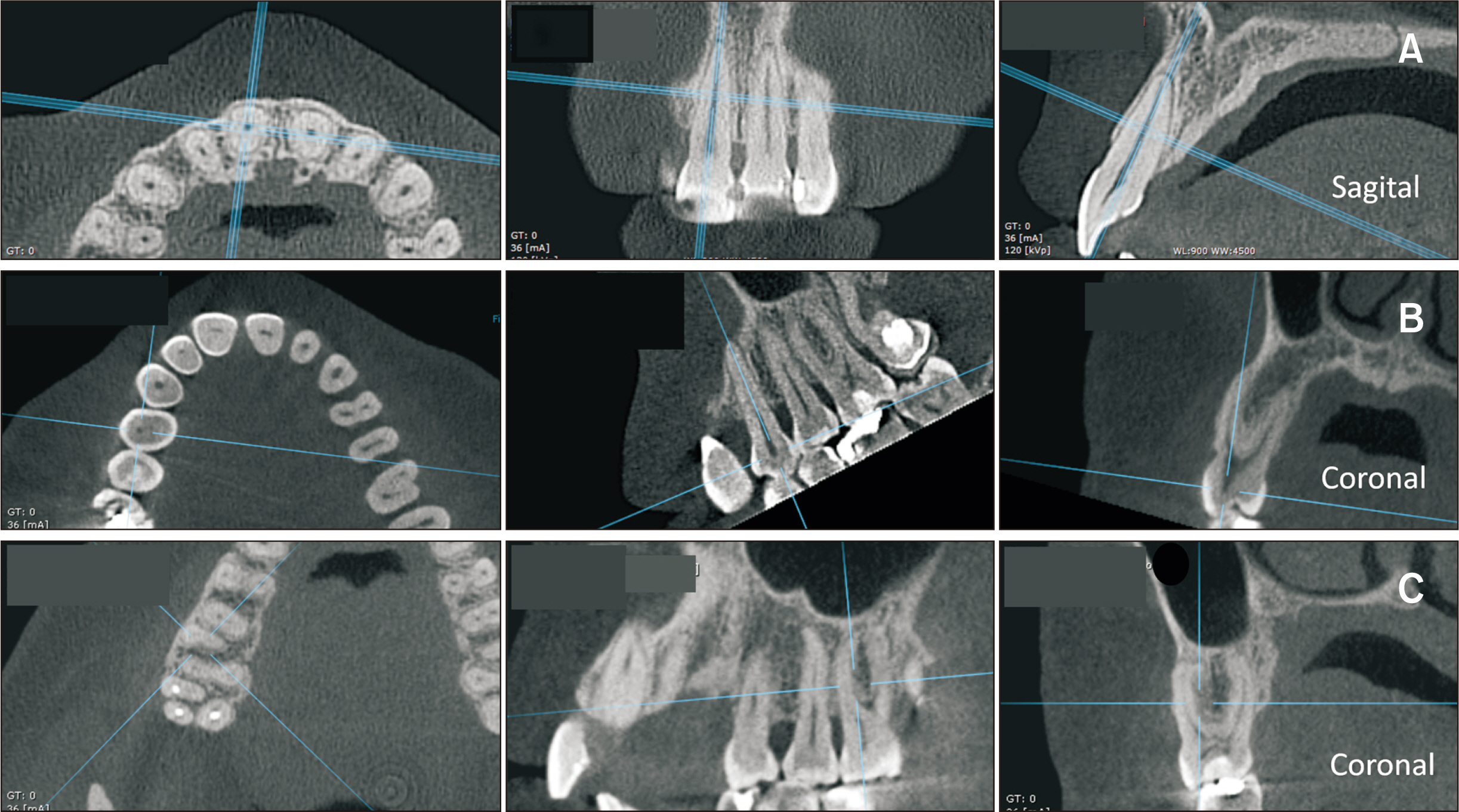
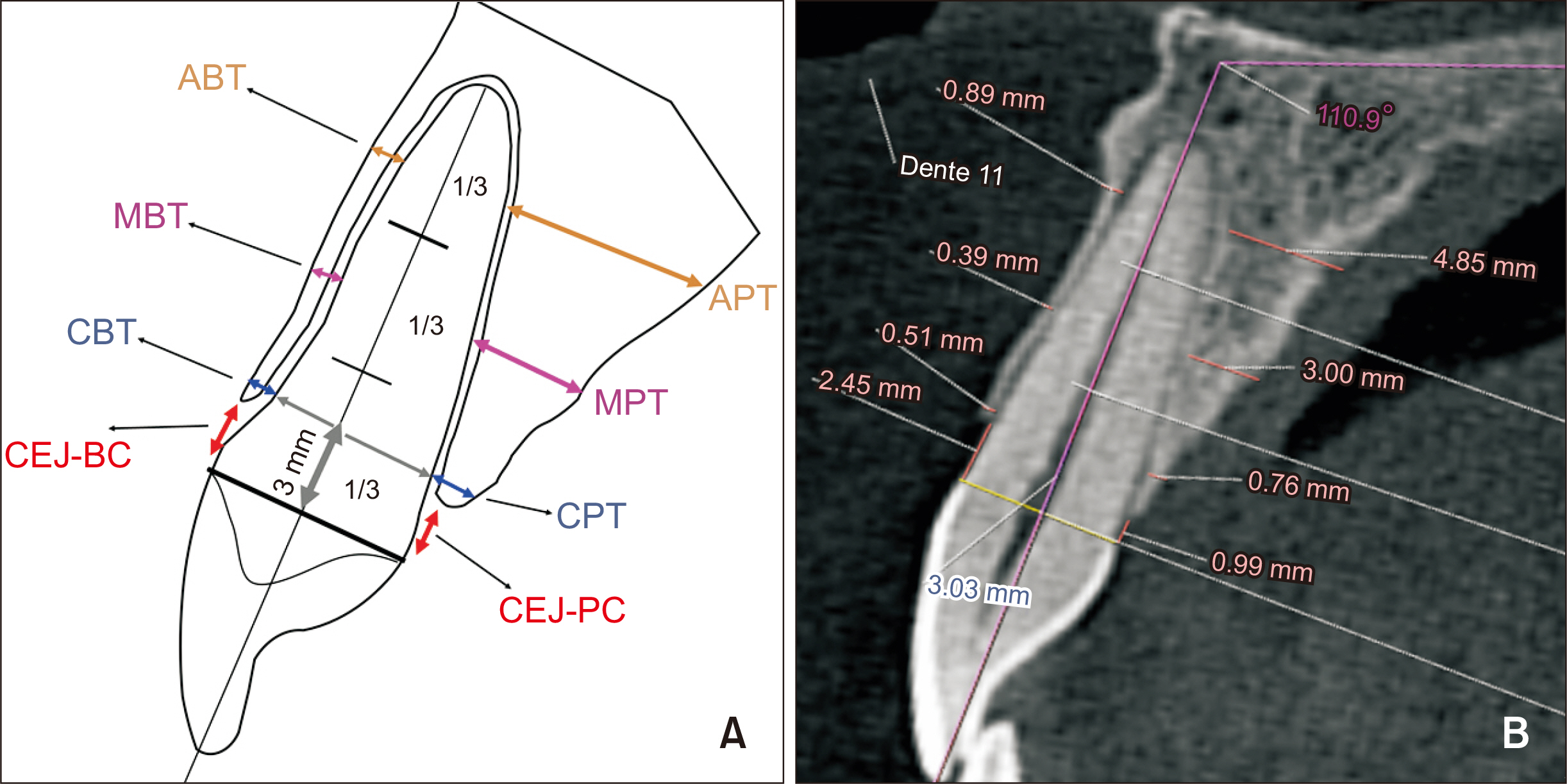
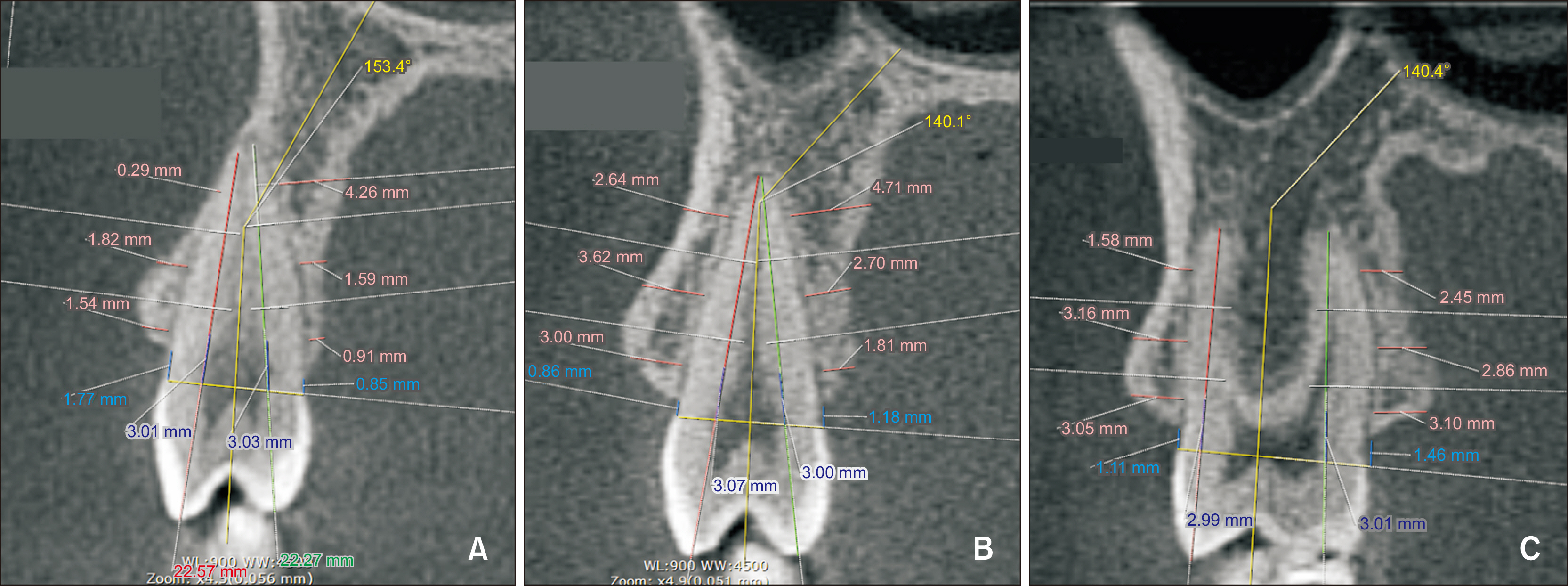
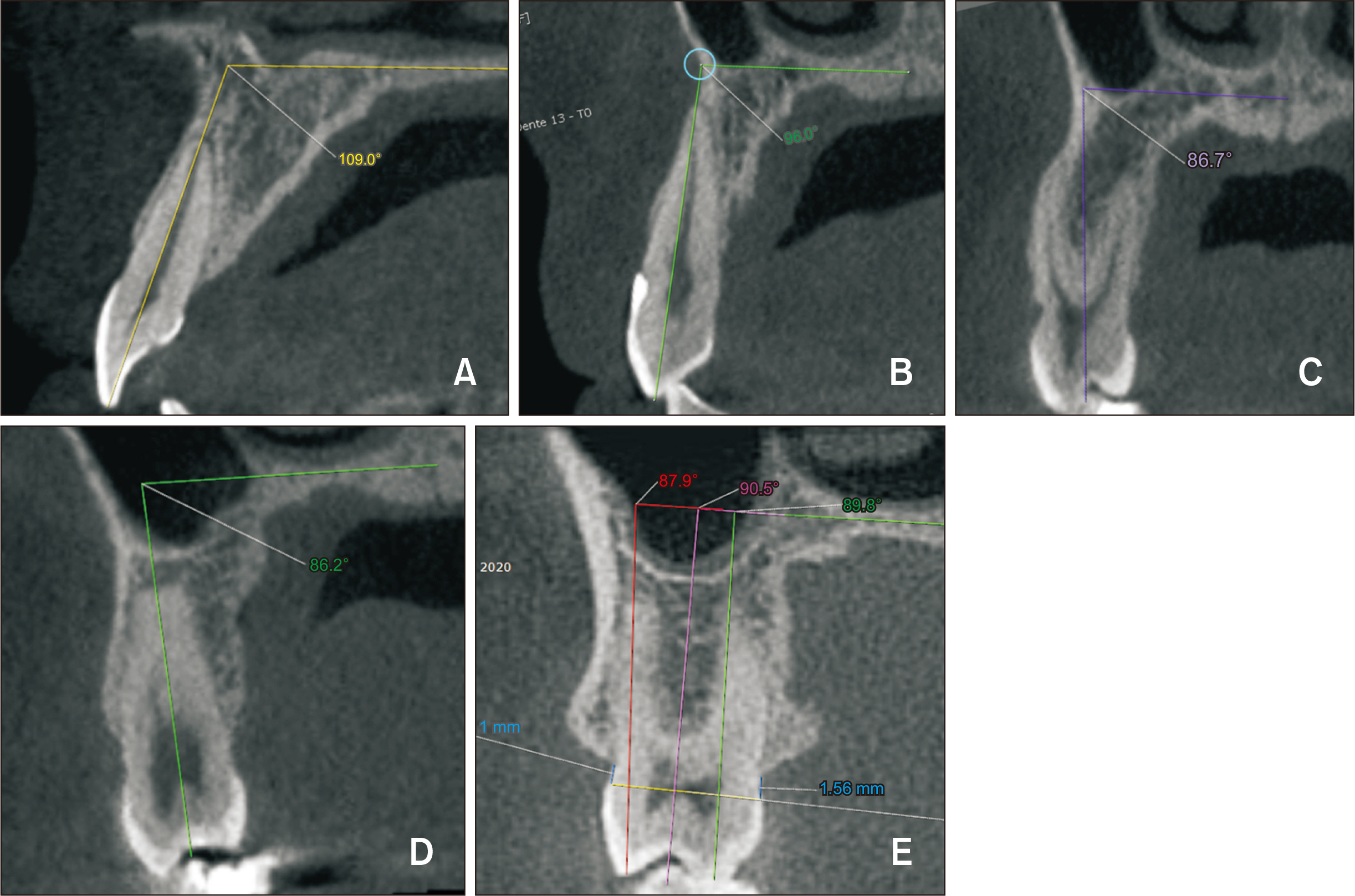
Methods
Thirty patients (22 females and 8 males; mean age: 36.3 years) were treated with Invisalign® aligners. Conebeam computed tomography and digital models were obtained before (T0) and after (T1) upper arch expansion. The bone thicknesses in the cervical, middle, and apical areas of the incisors, canines, premolar, and first molars were buccally and palatally measured, totaling 96 areas and 2,880 measurements. The buccolingual inclinations and transverse measurements of the teeth were obtained from digital models to correlate them with the bone changes. The statistical tests used were Student’s t-test, analysis of variance, and Pearson’s correlation tests (p < 0.05).
Results
From the 96 areas evaluated, 84 revealed an increase or stability in the alveolar bone thickness and twelve displayed significant bone loss. Bone changes did not correlate with the tooth inclination and transverse measurements.
Conclusions
Within the limitation of the present study, mild levels of upper arch expansion obtained with Invisalign® aligners in adult patients did not result in any clinically significant loss of alveolar bone thickness.
Figure
Reference
-
1. Christoph KM, Campbell PM, Feng JQ, Taylor RW, Jacob HB, Buschang PH. 2020; Effects of transverse bodily movements of maxillary premolars on the surrounding hard tissue. Am J Orthod Dentofacial Orthop. 157:490–502. https://doi.org/10.1016/j.ajodo.2018.11.022. DOI: 10.1016/j.ajodo.2018.11.022. PMID: 32241356.
Article2. Andrucioli MCD, Matsumoto MAN. 2020; Transverse maxillary deficiency: treatment alternatives in face of early skeletal maturation. Dental Press J Orthod. 25:70–9. https://doi.org/10.1590/2177-6709.25.1.070-079.bbo. DOI: 10.1590/2177-6709.25.1.070-079.bbo. PMID: 32215481. PMCID: PMC7077945. PMID: 01155444ca104e78b1e85f3c4c4297dc.
Article3. Zhou N, Guo J. 2020; Efficiency of upper arch expansion with the Invisalign system. Angle Orthod. 90:23–30. https://doi.org/10.2319/022719-151.1. DOI: 10.2319/022719-151.1. PMID: 31368778. PMCID: PMC8087062.
Article4. Bin Bahar BSK, Alkhalidy SR, Kaklamanos EG, Athanasiou AE. 2020; Do orthodontic patients develop more gingival recession in anterior teeth compared to untreated individuals? A systematic review of controlled studies. Int Orthod. 18:1–9. https://doi.org/10.1016/j.ortho.2019.08.025. DOI: 10.1016/j.ortho.2019.08.025. PMID: 31685434.
Article5. Morais JF, Melsen B, de Freitas KMS, Castello Branco N, Garib DG, Cattaneo PM. 2018; Evaluation of maxillary buccal alveolar bone before and after orthodontic alignment without extractions: a cone beam computed tomographic study. Angle Orthod. 88:748–56. https://doi.org/10.2319/101117-686.1. DOI: 10.2319/101117-686.1. PMID: 29911904. PMCID: PMC8174062.
Article6. Antoun JS, Mei L, Gibbs K, Farella M. 2017; Effect of orthodontic treatment on the periodontal tissues. Periodontol 2000. 74:140–57. https://doi.org/10.1111/prd.12194. DOI: 10.1111/prd.12194. PMID: 28429487.
Article7. Machado AW, MacGinnis M, Damis L, Moon W. 2014; Spontaneous improvement of gingival recession after correction of tooth positioning. Am J Orthod Dentofacial Orthop. 145:828–35. https://doi.org/10.1016/j.ajodo.2013.05.012. DOI: 10.1016/j.ajodo.2013.05.012. PMID: 24880854.
Article8. Cattaneo PM, Treccani M, Carlsson K, Thorgeirsson T, Myrda A, Cevidanes LH, et al. 2011; Transversal maxillary dento-alveolar changes in patients treated with active and passive self-ligating brackets: a randomized clinical trial using CBCT-scans and digital models. Orthod Craniofac Res. 14:222–33. https://doi.org/10.1111/j.1601-6343.2011.01527.x. DOI: 10.1111/j.1601-6343.2011.01527.x. PMID: 22008302.
Article9. Sendyk M, Linhares DS, Pannuti CM, Paiva JB, Rino Neto J. 2019; Effect of orthodontic treatment on alveolar bone thickness in adults: a systematic review. Dental Press J Orthod. 24:34–45. https://doi.org/10.1590/2177-6709.24.4.034-045.oar. DOI: 10.1590/2177-6709.24.4.034-045.oar. PMID: 31508705. PMCID: PMC6733232.
Article10. Nahás-Scocate AC, de Siqueira Brandão A, Patel MP, Lipiec-Ximenez ME, Chilvarquer I, do Valle-Corotti KM. 2014; Bone tissue amount related to upper incisors inclination. Angle Orthod. 84:279–85. https://doi.org/10.2319/031213-211.1. DOI: 10.2319/031213-211.1. PMID: 23883305. PMCID: PMC8673802.
Article11. Jäger F, Mah JK, Bumann A. 2017; Peridental bone changes after orthodontic tooth movement with fixed appliances: a cone-beam computed tomographic study. Angle Orthod. 87:672–80. https://doi.org/10.2319/102716-774.1. DOI: 10.2319/102716-774.1. PMID: 28553985. PMCID: PMC8357220.
Article12. Wang CW, Yu SH, Mandelaris GA, Wang HL. 2020; Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An American Academy of Periodontology best evidence review. J Periodontol. 91:299–310. https://doi.org/10.1002/JPER.19-0037. DOI: 10.1002/JPER.19-0037. PMID: 31670836.13. Matsumoto K, Sherrill-Mix S, Boucher N, Tanna N. 2020; A cone-beam computed tomographic evaluation of alveolar bone dimensional changes and the periodontal limits of mandibular incisor advancement in skeletal Class II patients. Angle Orthod. 90:330–8. https://doi.org/10.2319/080219-510.1. DOI: 10.2319/080219-510.1. PMID: 33378440. PMCID: PMC8032294.14. Castro LO, Castro IO, de Alencar AH, Valladares-Neto J, Estrela C. 2016; Cone beam computed tomography evaluation of distance from cementoenamel junction to alveolar crest before and after nonextraction orthodontic treatment. Angle Orthod. 86:543–9. https://doi.org/10.2319/040815-235.1. DOI: 10.2319/040815-235.1. PMID: 26379114. PMCID: PMC8601496.15. White DW, Julien KC, Jacob H, Campbell PM, Buschang PH. 2017; Discomfort associated with Invisalign and traditional brackets: a randomized, prospective trial. Angle Orthod. 87:801–8. https://doi.org/10.2319/091416-687.1. DOI: 10.2319/091416-687.1. PMID: 28753032. PMCID: PMC8317568.16. Timock AM, Cook V, McDonald T, Leo MC, Crowe J, Benninger BL, et al. 2011; Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 140:734–44. https://doi.org/10.1016/j.ajodo.2011.06.021. DOI: 10.1016/j.ajodo.2011.06.021. PMID: 22051495.17. Patcas R, Müller L, Ullrich O, Peltomäki T. 2012; Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 141:41–50. https://doi.org/10.1016/j.ajodo.2011.06.034. DOI: 10.1016/j.ajodo.2011.06.034. PMID: 22196184.18. Enhos S, Uysal T, Yagci A, Veli İ, Ucar FI, Ozer T. 2012; Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod. 82:868–74. https://doi.org/10.2319/111211-702.1. DOI: 10.2319/111211-702.1. PMID: 22356702. PMCID: PMC8823119.19. Barreda GJ, Dzierewianko EA, Mazza V, Muñoz KA, Piccoli GI, Romanelli HJ. 2020; Expansion treatment using Invisalign®: periodontal health status and maxillary buccal bone changes. A clinical and tomographic evaluation. Acta Odontol Latinoam. 33:69–81. https://doi.org/10.54589/aol.33/2/069. DOI: 10.54589/aol.33/2/069. PMID: 32920608.20. Jiang T, Wang JK, Jiang YY, Hu Z, Tang GH. 2021; How well do integrated 3D models predict alveolar defects after treatment with clear aligners? Angle Orthod. 91:313–9. https://doi.org/10.2319/042220-342.1. DOI: 10.2319/042220-342.1. PMID: 33492354. PMCID: PMC8084466.21. Levrini L, Carganico A, Abbate L. 2021; Maxillary expansion with clear aligners in the mixed dentition: a preliminary study with Invisalign® First system. Eur J Paediatr Dent. 22:125–8. https://doi.org/10.23804/ejpd.2021.22.02.7.22. Montaruli G, Virgilio S, Laurenziello M, Tepedino M, Ciavarella D. 2022; Maxillary transverse deficit: a retrospective study of two biologically oriented devices through a digital workflow. Bioengineering (Basel). 9:31. https://doi.org/10.3390/bioengineering9010031. DOI: 10.3390/bioengineering9010031. PMID: 35049740. PMCID: PMC8773167. PMID: 0ff8e3388f2a41eca01a9782ccb3c74e.23. Daou R, Nassar R, Khoury E, Ghoubril J. 2020; Changes of arch form at the end of orthodontic treatment, based on the Ricketts pentamorphic arch forms. Am J Orthod Dentofacial Orthop. 158:807–15. https://doi.org/10.1016/j.ajodo.2019.10.023. DOI: 10.1016/j.ajodo.2019.10.023. PMID: 33012595.24. Nahás-Scocate AC, Scocate MC. 2014; A classification of alveolar bone tissue. Quintessence Int. 45:515–9. https://doi.org/10.3290/j.qi.a31542. DOI: 10.3290/j.qi.a31542. PMID: 24618573.25. Zasčiurinskienė E, Lund H, Lindsten R, Jansson H, Bjerklin K. 2019; Outcome of periodontal-orthodontic treatment in subjects with periodontal disease. Part II: a CBCT study of alveolar bone level changes. Eur J Orthod. 41:565–74. https://doi.org/10.1093/ejo/cjz039. DOI: 10.1093/ejo/cjz039. PMID: 31276583.26. Maspero C, Gaffuri F, Castro IO, Lanteri V, Ugolini A, Farronato M. 2019; Correlation between dental vestibular-palatal inclination and alveolar bone remodeling after orthodontic treatment: a CBCT analysis. Materials (Basel). 12:4225. https://doi.org/10.3390/ma12244225. DOI: 10.3390/ma12244225. PMID: 31888251. PMCID: PMC6947223.27. Ramos AL, Dos Santos MC, de Almeida MR, Mir CF. 2020; Bone dehiscence formation during orthodontic tooth movement through atrophic alveolar ridges. Angle Orthod. 90:321–9. https://doi.org/10.2319/063019-443.1. DOI: 10.2319/063019-443.1. PMID: 33378432. PMCID: PMC8032313.28. Sheng Y, Guo HM, Bai YX, Li S. 2020; Dehiscence and fenestration in anterior teeth: comparison before and after orthodontic treatment. J Orofac Orthop. 81:1–9. https://doi.org/10.1007/s00056-019-00196-4. DOI: 10.1007/s00056-019-00196-4. PMID: 31646344.29. Garib DG, Yatabe MS, Ozawa TO, Silva Filho OG. 2010; Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dental Press J Orthod. 15:192–205. https://doi.org/10.1590/S2176-94512010000500023. DOI: 10.1590/S2176-94512010000500023. PMID: d2fe53efb95a45d2b5a8ab6eef782798.30. Sun L, Zhang L, Shen G, Wang B, Fang B. 2015; Accuracy of cone-beam computed tomography in detecting alveolar bone dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 147:313–23. https://doi.org/10.1016/j.ajodo.2014.10.032. DOI: 10.1016/j.ajodo.2014.10.032. PMID: 25726398.31. Fuhrmann RA, Bücker A, Diedrich PR. 1995; Assessment of alveolar bone loss with high resolution computed tomography. J Periodontal Res. 30:258–63. https://doi.org/10.1111/j.1600-0765.1995.tb02131.x. DOI: 10.1111/j.1600-0765.1995.tb02131.x. PMID: 7562322.32. Leung CC, Palomo L, Griffith R, Hans MG. 2010; Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 137(4 Suppl):S109–19. https://doi.org/10.1016/j.ajodo.2009.07.013. DOI: 10.1016/j.ajodo.2009.07.013. PMID: 20381751.33. Menezes CC, Janson G, da Silveira Massaro C, Cambiaghi L, Garib DG. 2016; Precision, reproducibility, and accuracy of bone crest level measurements of CBCT cross sections using different resolutions. Angle Orthod. 86:535–42. https://doi.org/10.2319/040115-214.1. DOI: 10.2319/040115-214.1. PMID: 26488463. PMCID: PMC8601492.34. Staderini E, Meuli S, Gallenzi P. 2019; Orthodontic treatment of class three malocclusion using clear aligners: a case report. J Oral Biol Craniofac Res. 9:360–2. https://doi.org/10.1016/j.jobcr.2019.09.004. DOI: 10.1016/j.jobcr.2019.09.004. PMID: 31667066. PMCID: PMC6811999.35. Figueiredo MA, Romano FL, Feres MFN, Stuani MBS, Nahás-Scocate ACR, Matsumoto MAN. 2021; Effectiveness of Invisalign® aligners in the treatment of severe gingival recession: a case report. Korean J Orthod. 51:293–300. https://doi.org/10.4041/kjod.2021.51.4.293. DOI: 10.4041/kjod.2021.51.4.293. PMID: 34275885. PMCID: PMC8290087.36. Evangelista K, Vasconcelos Kde F, Bumann A, Hirsch E, Nitka M, Silva MA. 2010; Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 138:133.e1–7. https://doi.org/10.1016/j.ajodo.2010.02.021. DOI: 10.1016/j.ajodo.2010.02.021. PMID: 20691344.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study
- A cone-beam computed tomography evaluation of buccal bone thickness following maxillary expansion
- Skeletal and dentoalveolar effects of different types of microimplant-assisted rapid palatal expansion
- Integrated three-dimensional digital assessment of accuracy of anterior tooth movement using clear aligners
- Evaluation of alveolar bone loss following rapid maxillary expansion using cone-beam computed tomography