J Korean Med Sci.
2023 Jul;38(30):e234. 10.3346/jkms.2023.38.e234.
Psychological and Personality Characteristics Associated With COVID-19 Vaccination Behavior in Korean General Population
- Affiliations
-
- 1Department of Psychiatry, Chonnam National University Medical School, Gwangju, Korea
- 2Department of Psychology, Chonnam National University, Gwangju, Korea
- 3Department of Biomedical Science, Chonnam National University Medical School, Gwangju, Korea
- 4Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea
- 5Mindlink, Gwangju Bukgu Mental Health Center, Gwangju, Korea
- KMID: 2544952
- DOI: http://doi.org/10.3346/jkms.2023.38.e234
Abstract
- Background
This study characterized coronavirus disease 2019 (COVID-19) vaccination behavior in the Korean general population using cluster analysis and explored related psychological factors.
Methods
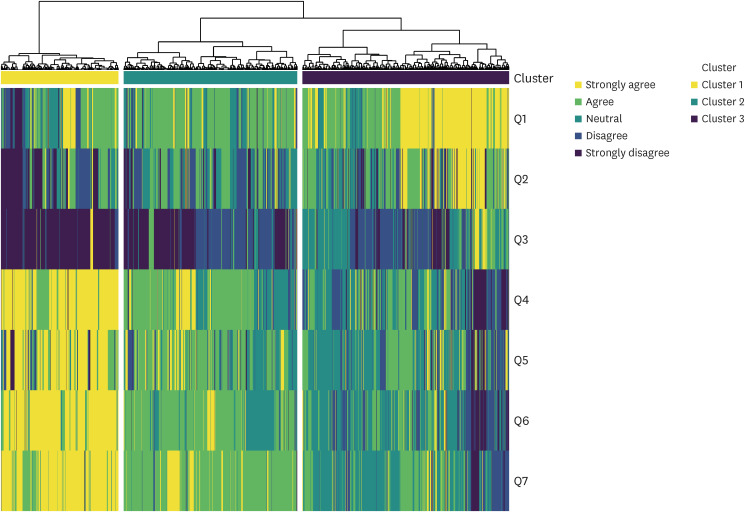
We categorized 1,500 individuals based on their attitudes toward COVID-19 vaccination using hierarchical clustering and identified their level of vaccine acceptance. We examined the associations between vaccine acceptance and behavioral and psychological characteristics.
Results
Clustering revealed three groups according to vaccine acceptance: ‘totally accepting’ (n = 354, 23.6%), ‘somewhat accepting’ (n = 523, 34.9%), and ‘reluctant’ (n = 623, 41.5%). Approximately 60% of all participants who belonged to the ‘totally accepting’ and ‘somewhat accepting’ groups were willing to receive a COVID-19 vaccine despite concerns about its side effects. High vaccine acceptance was associated with older age, regular influenza vaccination, and trust in formal sources of information. Participants with high vaccine acceptance had higher levels of gratitude, extraversion, agreeableness, and conscientiousness, and lower levels of depression, anxiety, and neuroticism.
Conclusions
People weighed the benefits of COVID-19 vaccination against the risk of side effects when deciding to receive the COVID-19 vaccine. Our findings also indicate that this vaccination behavior may be affected by coping mechanisms and psychological factors.
Keyword
Figure
Reference
-
1. Yoo JH, Hong ST. The outbreak cases with the novel coronavirus suggest upgraded quarantine and isolation in Korea. J Korean Med Sci. 2020; 35(5):e62. PMID: 32030926.2. Nham E, Song JY, Noh JY, Cheong HJ, Kim WJ. COVID-19 vaccination in Korea: past, present, and the way forward. J Korean Med Sci. 2022; 37(47):e351. PMID: 36472087.3. Landler M. Vaccine mandates rekindle fierce debate over civil liberties. The New York Times. 2021. 12. 10.4. Jiang S. Don’t rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020; 579(7799):321. PMID: 32179860.5. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021; 384(5):403–416. PMID: 33378609.6. Karlsson LC, Soveri A, Lewandowsky S, Karlsson L, Karlsson H, Nolvi S, et al. Fearing the disease or the vaccine: the case of COVID-19. Pers Individ Dif. 2021; 172:110590. PMID: 33518869.7. Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022; 28(3):456–459. PMID: 35273403.8. Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020; 263:113356. PMID: 32967786.9. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015; 33(34):4161–4164. PMID: 25896383.10. Dubé È, Ward JK, Verger P, MacDonald NE. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu Rev Public Health. 2021; 42(1):175–191. PMID: 33798403.11. Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021; 12(1):29. PMID: 33397962.12. Hwang SE, Kim WH, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccin Immunother. 2022; 18(1):1–8.13. Kreps S, Dasgupta N, Brownstein JS, Hswen Y, Kriner DL. Public attitudes toward COVID-19 vaccination: the role of vaccine attributes, incentives, and misinformation. NPJ Vaccines. 2021; 6(1):73. PMID: 33990614.14. Park HK, Ham JH, Jang DH, Lee JY, Jang WM. Political ideologies, government trust, and COVID-19 vaccine hesitancy in South Korea: a cross-sectional survey. Int J Environ Res Public Health. 2021; 18(20):10655. PMID: 34682401.15. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021; 27(2):225–228. PMID: 33082575.16. Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines (Basel). 2022; 10(1):110. PMID: 35062771.17. Kim M, Park IH, Kang YS, Kim H, Jhon M, Kim JW, et al. Comparison of psychosocial distress in areas with different COVID-19 prevalence in Korea. Front Psychiatry. 2020; 11:593105. PMID: 33329143.18. Lee YR, Lee JY, Park IH, Kim M, Jhon M, Kim JW, et al. The relationships among media usage regarding COVID-19, knowledge about infection, and anxiety: structural model analysis. J Korean Med Sci. 2020; 35(48):e426. PMID: 33316862.19. Jung HR, Park C, Kim M, Jhon M, Kim JW, Ryu S, et al. Factors associated with mask wearing among psychiatric inpatients during the COVID-19 pandemic. Schizophr Res. 2021; 228:235–236. PMID: 33476952.20. Kim SW, Park IH, Kim M, Park AL, Jhon M, Kim JW, et al. Risk and protective factors of depression in the general population during the COVID-19 epidemic in Korea. BMC Psychiatry. 2021; 21(1):445. PMID: 34496823.21. Lee JY, Kim M, Jhon M, Kim JW, Ryu S, Kim JM, et al. Factors associated with a negative emotional response to news media and nationwide emergency text alerts during the COVID-19 outbreak in Korea. Psychiatry Investig. 2021; 18(9):825–830.22. Ryu S, Park IH, Kim M, Lee YR, Lee J, Kim H, et al. Network study of responses to unusualness and psychological stress during the COVID-19 outbreak in Korea. PLoS One. 2021; 16(2):e0246894. PMID: 33635935.23. Jang H, Park AL, Lee YR, Ryu S, Lee JY, Kim JM, et al. Relationship between economic loss and anxiety during the coronavirus disease 2019 pandemic: moderating effects of knowledge, gratitude, and perceived stress. Front Psychiatry. 2022; 13:904449. PMID: 35770062.24. Lee YR, Chung YC, Kim JJ, Kang SH, Lee BJ, Lee SH, et al. Effects of COVID-19-related stress and fear on depression in schizophrenia patients and the general population. Schizophrenia (Heidelb). 2022; 8(1):15. PMID: 35249110.25. Korea Disease Control and Prevention Agency. COVID-19 vaccination. Accessed December 20, 2022. https://ncv.kdca.go.kr/eng/ .26. Park SJ, Choi HR, Choi JH, Kim KW, Hong JP. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood. 2010; 6(2):119–124.27. Lee SH, Shin C, Kim H, Jeon SW, Yoon HK, Ko YH, et al. Validation of the Korean version of the Generalized Anxiety Disorder 7 self-rating scale. Asia-Pac Psychiatry. 2022; 14(1):e12421. PMID: 32893471.28. Mccullough ME, Emmons RA, Tsang JA. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol. 2002; 82(1):112–127. PMID: 11811629.29. Kwon SJ, Kim KH, Lee HS. Validation of the Korean version of gratitude questionnaire. Korean J Health Psychol. 2006; 11(1):177–190.30. Rammstedt B, John OP. Measuring personality in one minute or less: a 10-item short version of the Big Five Inventory in English and German. J Res Pers. 2007; 41(1):203–212.31. Kim SY, Kim JM, Yoo JA, Bae KY, Kim SW, Yang SJ, et al. Standardization and validation of big five inventory-Korean version (BFI-K) in elders. Korean J Biol Psychiatry. 2010; 17(1):15–25.32. Bolin JH, Edwards JM, Finch WH, Cassady JC. Applications of cluster analysis to the creation of perfectionism profiles: a comparison of two clustering approaches. Front Psychol. 2014; 5:343. PMID: 24795683.33. Murtagh F, Contreras P. Algorithms for hierarchical clustering: an overview. Wiley Interdiscip Rev Data Min Knowl Discov. 2012; 2(1):86–97.34. Felten R, Dubois M, Ugarte-Gil MF, Chaudier A, Kawka L, Bergier H, et al. Cluster analysis reveals three main patterns of beliefs and intention with respect to SARS-CoV-2 vaccination in patients with autoimmune and inflammatory diseases. Rheumatology (Oxford). 2021; 60(SI):SI68–SI76. PMID: 33983432.35. Sallam M, Al-Sanafi M, Sallam M. A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. 2022; 15:21–45. PMID: 35046661.36. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020; 38(42):6500–6507. PMID: 32863069.37. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine : a survey of U.S. adults. Ann Intern Med. 2020; 173(12):964–973. PMID: 32886525.38. Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021; 94:41–50. PMID: 33713824.39. Al-Hanawi MK, Alshareef N, El-Sokkary RH. Willingness to receive COVID-19 vaccination among older adults in Saudi Arabia: a community-based survey. Vaccines (Basel). 2021; 9(11):1257. PMID: 34835188.40. Zintel S, Flock C, Arbogast AL, Forster A, von Wagner C, Sieverding M. Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis. Z Gesundh Wiss. 2022.41. Sprengholz P, Korn L, Eitze S, Felgendreff L, Siegers R, Goldhahn L, et al. Attitude toward a mandatory COVID-19 vaccination policy and its determinants: evidence from serial cross-sectional surveys conducted throughout the pandemic in Germany. Vaccine. 2022; 40(51):7370–7377. PMID: 35153092.42. Leuchter RK, Jackson NJ, Mafi JN, Sarkisian CA. Association between Covid-19 vaccination and influenza vaccination rates. N Engl J Med. 2022; 386(26):2531–2532. PMID: 35704429.43. Sharma B, Racey CS, Booth A, Albert A, Smith LW, Gottschlich A, et al. Characterizing intentions to receive the COVID-19 vaccine among the general population in British Columbia based on their future intentions towards the seasonal influenza vaccine. Vaccine X. 2022; 12:100208. PMID: 35996447.44. Kumar S, Shah Z, Garfield S. Causes of vaccine hesitancy in adults for the influenza and COVID-19 vaccines: a systematic literature review. Vaccines (Basel). 2022; 10(9):1518. PMID: 36146596.45. Klüver H, Hartmann F, Humphreys M, Geissler F, Giesecke J. Incentives can spur COVID-19 vaccination uptake. Proc Natl Acad Sci U S A. 2021; 118(36):e2109543118. PMID: 34413212.46. Tan M, Straughan PT, Cheong G. Information trust and COVID-19 vaccine hesitancy amongst middle-aged and older adults in Singapore: a latent class analysis Approach. Soc Sci Med. 2022; 296:114767. PMID: 35144226.47. Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020; 5(10):e004206.48. Lee SK, Sun J, Jang S, Connelly S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022; 12(1):13681. PMID: 35953500.49. Sekizawa Y, Hashimoto S, Denda K, Ochi S, So M. Association between COVID-19 vaccine hesitancy and generalized trust, depression, generalized anxiety, and fear of COVID-19. BMC Public Health. 2022; 22(1):126. PMID: 35042506.50. Koltai J, Raifman J, Bor J, McKee M, Stuckler D. COVID-19 vaccination and mental health: a difference-in-difference analysis of the understanding America study. Am J Prev Med. 2022; 62(5):679–687. PMID: 35012830.51. Wood AM, Froh JJ, Geraghty AW. Gratitude and well-being: a review and theoretical integration. Clin Psychol Rev. 2010; 30(7):890–905. PMID: 20451313.52. Kumar SA, Edwards ME, Grandgenett HM, Scherer LL, DiLillo D, Jaffe AE. Does gratitude promote resilience during a pandemic? An examination of mental health and positivity at the onset of COVID-19. J Happiness Stud. 2022; 23(7):3463–3483. PMID: 35855779.53. Jans-Beken L. A perspective on mature gratitude as a way of coping with COVID-19. Front Psychol. 2021; 12:632911. PMID: 33828504.54. Lee JY, Kim M, Jhon M, Kim H, Kang HJ, Ryu S, et al. The association of gratitude with perceived stress among nurses in Korea during COVID-19 outbreak. Arch Psychiatr Nurs. 2021; 35(6):647–652. PMID: 34861959.55. Karns CM, Moore WE 3rd, Mayr U. The cultivation of pure altruism via gratitude: a functional MRI study of change with gratitude practice. Front Hum Neurosci. 2017; 11:599. PMID: 29375336.56. Wilt J, Revelle W. Extraversion. Leary MR, Hoyle RH, editors. Handbook of Individual Differences in Social Behavior. New York, NY, USA: The Guilford Press;2009. p. 27–45.57. Graziano WG, Tobin RM. Agreeableness. Leary MR, Hoyle RH, editors. Handbook of Individual Differences in Social Behavior. New York, NY, USA: The Guilford Press;2009. p. 46–61.58. Roberts BW, Jackson JJ, Fayard JV, Edmonds G, Meints J. Conscientiousness. Leary MR, Hoyle RH, editors. Handbook of Individual Differences in Social Behavior. New York, NY, USA: The Guilford Press;2009. p. 369–381. .59. Lahey BB. Public health significance of neuroticism. Am Psychol. 2009; 64(4):241–256. PMID: 19449983.60. Lin FY, Wang CH. Personality and individual attitudes toward vaccination: a nationally representative survey in the United States. BMC Public Health. 2020; 20(1):1759. PMID: 33228661.61. Halstead IN, McKay RT, Lewis GJ. COVID-19 and seasonal flu vaccination hesitancy: Links to personality and general intelligence in a large, UK cohort. Vaccine. 2022; 40(32):4488–4495. PMID: 35710507.62. Howard MC. The good, the bad, and the neutral: vaccine hesitancy mediates the relations of Psychological Capital, the Dark Triad, and the Big Five with vaccination willingness and behaviors. Pers Individ Dif. 2022; 190:111523. PMID: 35079191.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Examination of Predicting Factors for COVID-19 Vaccination Behaviors of University Students Utilizing the Theory of Planned Behavior
- Immune Response to COVID-19 Vaccination in Hematologic Malignancies: A Mini-Review
- The Effect of Psychological Factors on COVID-19 Vaccination Side Effects: A Cross-Sectional Survey in South Korea
- A Case of Aphthous Stomatitis in a Healthy Adult Following COVID-19 Vaccination: Clinical Reasoning
- Why Fast COVID-19 Vaccination Needed for People with Disabilities and Autistics in Korea?