J Rhinol.
2023 Jul;30(2):105-114. 10.18787/jr.2023.00024.
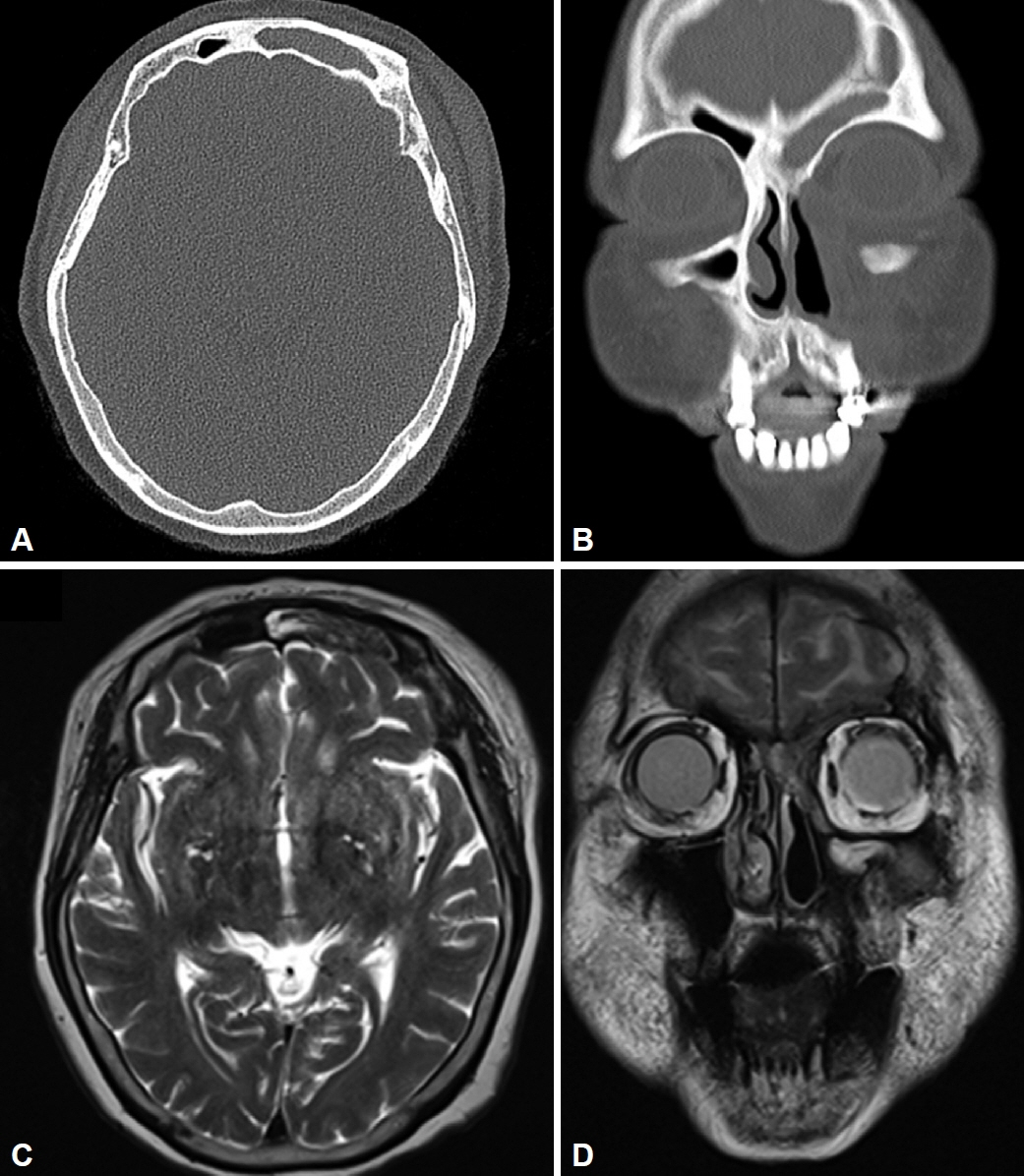
Two Cases of Frontal Sinus Inverted Papilloma Treated With a Combined Bifrontal Craniotomy and Endonasal Endoscopic Approach
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Suwon St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 2Department of Otolaryngology-Head and Neck Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- KMID: 2544620
- DOI: http://doi.org/10.18787/jr.2023.00024
Abstract
- An inverted papilloma of the frontal sinus is a challenging lesion for surgeons, for both anatomical and pathological reasons. Despite the trend away from an external approach and towards an endonasal endoscopic approach, indications for an external approach remain. The options for an external approach include endoscopic frontal trephination, transpalpebral orbital craniotomy, a supraorbital transeyebrow approach, an osteoplastic flap, and bifrontal craniotomy with cranialization. Each approach has advantages and disadvantages. Deciding on the appropriate approach is important for the patient’s prognosis and risk of complications. We report two cases of frontal sinus inverted papilloma treated with a combined bifrontal craniotomy with cranialization and endonasal endoscopic approach. We also present a general review of the external approaches mentioned above.
Figure
Reference
-
References
1. Pietrobon G, Karligkiotis A, Turri-Zanoni M, Fazio E, Battaglia P, Bignami M, et al. Surgical management of inverted papilloma involving the frontal sinus: a practical algorithm for treatment planning. Acta Otorhinolaryngol Ital. 2019; 39(1):28–39.2. Kamel RH, Abdel Fattah AF, Awad AG. Origin oriented management of inverted papilloma of the frontal sinus. Rhinology. 2012; 50(3):262–8.3. Lee YH, Lee JY, Lawson W. Indications and outcomes of the osteoplastic flap procedure with or without obliteration. J Craniofac Surg. 2020; 31(8):2243–9.4. Albathi M, Ramanathan M Jr, Lane AP, Boahene KDO. Combined endonasal and eyelid approach for management of extensive frontal sinus inverting papilloma. Laryngoscope. 2018; 128(1):3–9.5. Gotlib T, Krzeski A, Held-Ziółkowska M, Niemczyk K. Endoscopic transnasal management of inverted papilloma involving frontal sinuses. Wideochir Inne Tech Maloinwazyjne. 2012; 7(4):299–303.6. Fokkens W, Harvey R. Management of the frontal sinuses. In : Flint PW, Haughey BH, Lund VJ, Robbins KT, Thomas JR, Lesperance MM, editors. otolaryngology: head and neck surgery. 7th ed. Philadelphia (PA): Elsevier;2021. p. 719–32.7. Walgama E, Ahn C, Batra PS. Surgical management of frontal sinus inverted papilloma: a systematic review. Laryngoscope. 2012; 122(6):1205–9.8. Noller M, Fischer JL, Gudis DA, Riley CA. The Draf III procedure: a review of indications and techniques. World J Otorhinolaryngol Head Neck Surg. 2022; 8(1):1–7.9. Turner JH, Vaezeafshar R, Hwang PH. Indications and outcomes for Draf IIB frontal sinus surgery. Am J Rhinol Allergy. 2016; 30(1):70–3.10. Patel AB, Cain RB, Lal D. Contemporary applications of frontal sinus trephination: a systematic review of the literature. Laryngoscope. 2015; 125(9):2046–53.11. Adawi MM, Abdelbaky AM. Validity of the lateral supraorbital approach as a minimally invasive corridor for orbital lesions. World Neurosurg. 2015; 84(3):766–71.12. Pitskhelauri DI, Sanikidze AZ, Abramov IT, Moshchev DA, Anan’ev EP, Eliseeva NM, et al. [The trans-eyebrow supraorbital approach for removal of anterior cranial fossa and suprasellar meningiomas]. Zh Vopr Neirokhir Im N N Burdenko. 2017; 81(6):89–98. Russian.13. Yu P, Mao X, Li X, Hu X, Li J, Sun G. Endoscopic frontal trephination verse the osteoplastic flap in patients with frontal sinus disease after bifrontal craniotomy. Br J Neurosurg. 2021; 35(1):65–7.14. Morse JC, Chandra RK. Is there still a role for cranialization in modern sinus surgery? Curr Opin Otolaryngol Head Neck Surg. 2021; 29(1):53–8.15. Ozlen F, Abuzayed B, Dashti R, Isler C, Tanriover N, Sanus GZ. Lowprofile 1-piece bifrontal craniotomy for anterior skull base approach and reconstruction. J Craniofac Surg. 2010; 21(1):233–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Surgery for Inverted Papilloma
- Widespread Inverted Papilloma in the Frontal Sinus Treated by Unilateral Osteoplastic Flap Surgery without Obliteration
- Clinical Analysis of Sinonasal Inverted Papilloma according to Surgical Approach
- Extensive Transbasal Approach to Skull Base Tumor
- Inverted Papilloma of the Sinonasal Cavity: The Surgical Strategy of Endoscopic Management Based on the Site of Attachment