J Yeungnam Med Sci.
2023 Jul;40(3):259-267. 10.12701/jyms.2022.00507.
Impact of Controlling Nutritional Status score on short-term outcomes after carotid endarterectomy: a retrospective cohort study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2544586
- DOI: http://doi.org/10.12701/jyms.2022.00507
Abstract
- Background
Malnutrition and impaired immune responses significantly affect the clinical outcomes of patients with atherosclerotic stenosis. The Controlling Nutritional Status (CONUT) score has recently been utilized to evaluate perioperative immunonutritional status. This study aimed to evaluate the relationship between immunonutritional status, indexed by CONUT score, and postoperative complications in patients undergoing carotid endarterectomy (CEA).
Methods
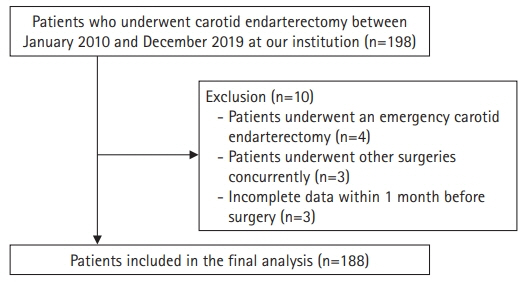
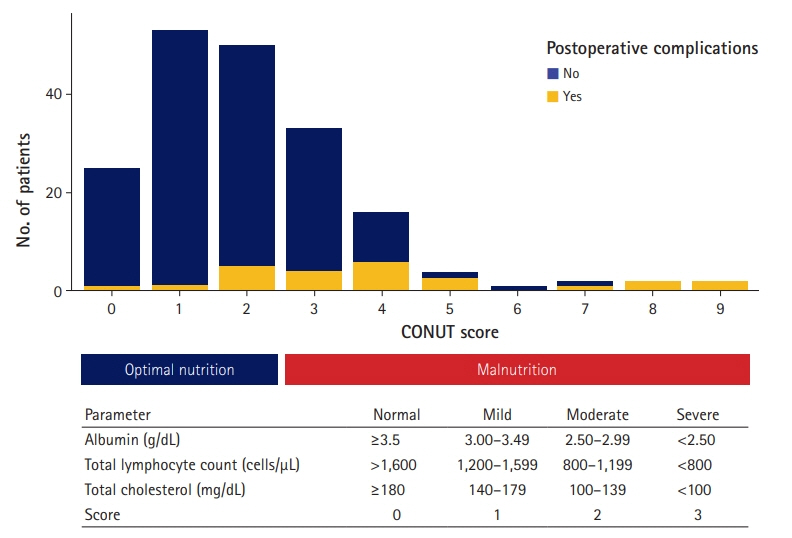
We retrospectively evaluated 188 patients who underwent elective CEA between January 2010 and December 2019. The preoperative CONUT score was calculated as the sum of the serum albumin concentration, total cholesterol level, and total lymphocyte count. The primary outcome was postoperative complications within 30 days after CEA, including major adverse cardiovascular events, pulmonary complications, stroke, renal failure, sepsis, wounds, and gastrointestinal complications. Cox proportional hazards regression analysis was used to estimate the factors associated with postoperative complications during the 30-day follow-up period.
Results
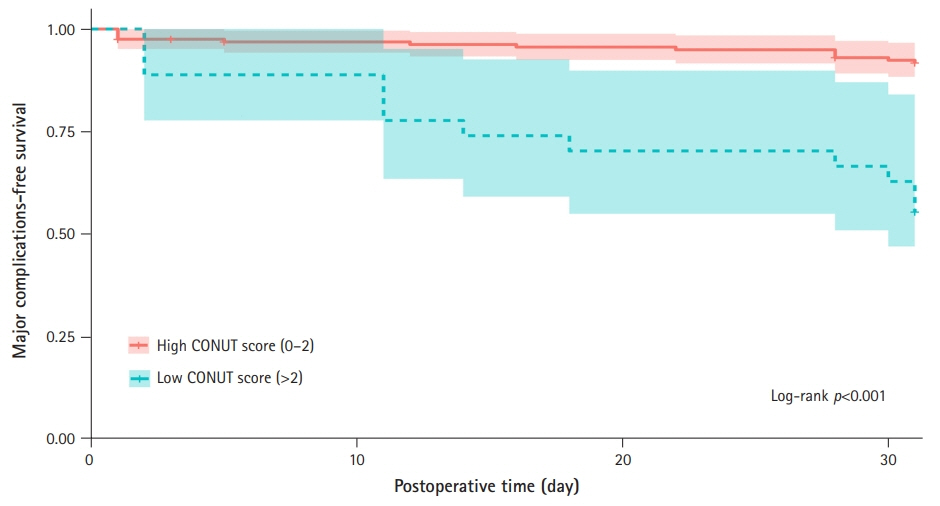
Twenty-five patients (13.3%) had at least one major complication. The incidence of postoperative complications was identified more frequently in the high CONUT group (12 of 27, 44.4% vs. 13 of 161, 8.1%; p<0.001). Multivariate analyses showed that a high preoperative CONUT score was independently associated with 30-day postoperative complications (hazard ratio, 5.98; 95% confidence interval, 2.56–13.97; p<0.001).
Conclusion
Our results showed that the CONUT score, a simple and readily available parameter using only objective laboratory values, is independently associated with early postoperative complications.
Keyword
Figure
Reference
-
References
1. French BR, Boddepalli RS, Govindarajan R. Acute ischemic stroke: current status and future directions. Mo Med. 2016; 113:480–6.2. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995; 273:1421–8.3. European Carotid Surgery Trialists’ Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet. 1991; 337:1235–43.4. Timmerman N, Waissi F, Dekker M, van de Pol QY, van Bennekom J, Schoneveld A, et al. Pre-operative plasma extracellular vesicle proteins are associated with a high risk of long term secondary major cardiovascular events in patients undergoing carotid endarterectomy. Eur J Vasc Endovasc Surg. 2021; 62:705–15.5. Jin H, Zhu K, Wang W. The predictive values of pretreatment controlling nutritional status (CONUT) score in estimating short- and long-term outcomes for patients with gastric cancer treated with neoadjuvant chemotherapy and curative gastrectomy. J Gastric Cancer. 2021; 21:155–68.6. Wang A, He Z, Cong P, Qu Y, Hu T, Cai Y, et al. Controlling nutritional status (CONUT) score as a new indicator of prognosis in patients with hilar cholangiocarcinoma is superior to NLR and PNI: a single-center retrospective study. Front Oncol. 2021; 10:593452.7. Müller L, Hahn F, Mähringer-Kunz A, Stoehr F, Gairing SJ, Foerster F, et al. Immunonutritive scoring in patients with hepatocellular carcinoma undergoing transarterial chemoembolization: Prognostic Nutritional Index or Controlling Nutritional Status score? Front Oncol. 2021; 11:696183.8. Kato T, Yaku H, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, et al. Association with controlling nutritional status (CONUT) score and in-hospital mortality and infection in acute heart failure. Sci Rep. 2020; 10:3320.9. Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015; 32:88–105.10. Poulia KA, Yannakoulia M, Karageorgou D, Gamaletsou M, Panagiotakos DB, Sipsas NV, et al. Evaluation of the efficacy of six nutritional screening tools to predict malnutrition in the elderly. Clin Nutr. 2012; 31:378–85.11. Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999; 15:116–22.12. Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987; 11:8–13.13. Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005; 82:777–83.14. Wang ZJ, Zhou YJ, Galper BZ, Gao F, Yeh RW, Mauri L. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: a systematic review and meta-analysis. Heart. 2015; 101:1631–8.15. Çakmak EÖ, Öcal L, Erdoğan E, Cerşit S, Efe SÇ, Karagöz A, et al. Prognostic value of 3 nutritional screening tools to predict 30-day outcome in patients undergoing carotid artery stenting. Angiology. 2022; 73:225–33.16. Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005; 20:38–45.17. Takagi K, Domagala P, Polak WG, Buettner S, Ijzermans JN. The controlling nutritional status score and postoperative complication risk in gastrointestinal and hepatopancreatobiliary surgical oncology: a systematic review and meta-analysis. Ann Nutr Metab. 2019; 74:303–12.18. Raposeiras Roubín S, Abu Assi E, Cespón Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada JA, et al. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome. J Am Coll Cardiol. 2020; 76:828–40.19. Foley NC, Salter KL, Robertson J, Teasell RW, Woodbury MG. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke. 2009; 40:e66–74.20. Steenhagen E. Preoperative nutritional optimization of esophageal cancer patients. J Thorac Dis. 2019; 11(Suppl 5):S645–53.21. Schillinger M, Exner M, Mlekusch W, Amighi J, Sabeti S, Schlager O, et al. Serum albumin predicts cardiac adverse events in patients with advanced atherosclerosis: interrelation with traditional cardiovascular risk factors. Thromb Haemost. 2004; 91:610–8.22. Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005; 45:1638–43.23. Cereda E, Pusani C, Limonta D, Vanotti A. The association of Geriatric Nutritional Risk Index and total lymphocyte count with short-term nutrition-related complications in institutionalised elderly. J Am Coll Nutr. 2008; 27:406–13.24. Gomes F, Emery PW, Weekes CE. Risk of malnutrition is an independent predictor of mortality, length of hospital stay, and hospitalization costs in stroke patients. J Stroke Cerebrovasc Dis. 2016; 25:799–806.25. Bandayrel K, Wong S. Systematic literature review of randomized control trials assessing the effectiveness of nutrition interventions in community-dwelling older adults. J Nutr Educ Behav. 2011; 43:251–62.26. Paraskevas KI, Mikhailidis DP, Veith FJ, Spence JD. Definition of best medical treatment in asymptomatic and symptomatic carotid artery stenosis. Angiology. 2016; 67:411–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical outcomes of staged bilateral carotid endarterectomy for bilateral carotid artery stenosis
- Is Carotid Stenting a Reasonable Alternative to Carotid Endarterectomy?
- Extracranial Carotid Disease: An Interpretation of Extracranial Carotid Artery Disease Guideline 2011
- Prognostic Significance of Preoperative Controlling Nutritional Status Score in Patients Who Underwent Hepatic Resection for Hepatocellular Carcinoma
- Recurrent Carotid Artery Stenosis